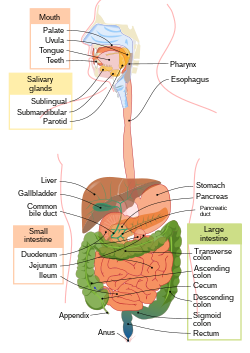
Thehuman digestive systemconsists of thegastrointestinal tractplus the accessory organs of digestion (thetongue,salivary glands,pancreas,liver,andgallbladder).Digestioninvolves the breakdown of food into smaller and smaller components, until they can be absorbed and assimilated into the body. The process of digestion has three stages: thecephalic phase,thegastric phase,and theintestinal phase.
| Human digestive system | |
|---|---|
 Human digestive system | |
| Details | |
| Identifiers | |
| Latin | systema digestorium |
| MeSH | D004064 |
| TA98 | A05.0.00.000 |
| TA2 | 2773 |
| TH | H3.04 |
| FMA | 7152 |
| Anatomical terminology | |
The first stage, the cephalic phase of digestion, begins with secretions fromgastric glandsin response to the sight and smell of food. This stage includes the mechanical breakdown of food bychewing,and the chemical breakdown bydigestive enzymes,that takes place in themouth.Salivacontains the digestive enzymesamylase,andlingual lipase,secreted by the salivary andserous glandson the tongue. Chewing, in which the food is mixed with saliva, begins the mechanical process of digestion. This produces aboluswhich is swallowed down theesophagusto enter thestomach.
The second stage, the gastric phase, happens in the stomach. Here, the food is further broken down by mixing withgastric aciduntil it passes into theduodenum,the first part of thesmall intestine.
The third stage, the intestinal phase, begins in the duodenum. Here, the partially digested food is mixed with a number ofenzymesproduced by the pancreas.
Digestion is helped by the chewing of food carried out by themuscles of mastication,the tongue, and theteeth,and also by thecontractionsofperistalsis,andsegmentation.Gastric acid, and the production ofmucusin the stomach, are essential for the continuation of digestion.
Peristalsis is the rhythmic contraction ofmusclesthat begins in the esophagus and continues along the wall of the stomach and the rest of the gastrointestinal tract. This initially results in the production ofchymewhich when fully broken down in the small intestine is absorbed aschyleinto thelymphatic system.Most of the digestion of food takes place in the small intestine. Water and somemineralsare reabsorbed back into the blood in the colon of thelarge intestine.The waste products of digestion (feces) aredefecatedfrom therectumvia theanus.
Components
There are several organs and other components involved in the digestion of food. The organs known as theaccessory digestive organsare theliver,gall bladderandpancreas.Other components include themouth,salivary glands,tongue,teethandepiglottis.
The largest structure of the digestivesystemis thegastrointestinal tract(GI tract). This starts at the mouth and ends at theanus,covering a distance of about nine metres (30 ft).[1]
A major digestive organ is thestomach.Within itsmucosaare millions of embeddedgastric glands.Their secretions are vital to the functioning of the organ.
Most of the digestion of food takes place in thesmall intestinewhich is the longest part of the GI tract.
The largest part of the GI tract is the colon orlarge intestine.Water is absorbed here and the remaining waste matter is stored prior todefecation.[2]
There are many specialisedcellsof the GI tract. These include the various cells of the gastric glands,taste cells,pancreatic duct cells,enterocytesandmicrofold cells.
Some parts of the digestive system are also part of theexcretory system,including the large intestine.[2]
Mouth
Themouthis the first part of theupper gastrointestinal tractand is equipped with several structures that begin the first processes of digestion.[3]These include salivary glands, teeth and the tongue. The mouth consists of two regions; the vestibule and the oral cavity proper. The vestibule is the area between the teeth, lips and cheeks,[4]and the rest is the oral cavity proper. Most of the oral cavity is lined withoral mucosa,amucous membranethat produces a lubricatingmucus,of which only a small amount is needed. Mucous membranes vary in structure in the different regions of the body but they all produce a lubricating mucus, which is either secreted by surface cells or more usually by underlying glands. The mucous membrane in the mouth continues as the thin mucosa which lines the bases of the teeth. The main component of mucus is aglycoproteincalledmucinand the type secreted varies according to the region involved. Mucin is viscous, clear, and clinging. Underlying the mucous membrane in the mouth is a thin layer ofsmooth muscle tissueand the loose connection to the membrane gives it its great elasticity.[5]It covers the cheeks, inner surfaces of thelips,and floor of the mouth, and the mucin produced is highly protective againsttooth decay.[6]
The roof of the mouth is termed thepalateand it separates the oral cavity from the nasal cavity. The palate is hard at the front of the mouth since the overlying mucosa is covering a plate ofbone;it is softer and more pliable at the back being made of muscle and connective tissue, and it can move to swallow food and liquids. Thesoft palateends at theuvula.[7]The surface of thehard palateallows for the pressure needed in eating food, to leave the nasal passage clear.[8]The opening between the lips is termed the oral fissure, and the opening into the throat is called thefauces.[9]
At either side of the soft palate are thepalatoglossus muscleswhich also reach into regions of the tongue. These muscles raise the back of the tongue and also close both sides of the fauces to enable food to be swallowed.[10]: 1208 Mucus helps in the mastication of food in its ability to soften and collect the food in the formation of the bolus.
Salivary glands
There are three pairs of mainsalivary glandsand between 800 and 1,000 minor salivary glands, all of which mainly serve the digestive process, and also play an important role in the maintenance of dental health and general mouth lubrication, without which speech would be impossible.[11]The main glands are allexocrine glands,secreting via ducts. All of these glands terminate in the mouth. The largest of these are theparotid glands—their secretion is mainlyserous.The next pair are underneath the jaw, thesubmandibular glands,these produce both serous fluid and mucus. The serous fluid is produced byserous glandsin these salivary glands which also producelingual lipase.They produce about 70% of the oral cavity saliva. The third pair are thesublingual glandslocated underneath the tongue and their secretion is mainly mucous with a small percentage of saliva.
Within the oral mucosa, and also on the tongue, palates, and floor of the mouth, are the minor salivary glands; their secretions are mainly mucous and they are innervated by thefacial nerve(CN7).[12]The glands also secreteamylasea first stage in the breakdown of food acting on the carbohydrate in the food to transform the starch content into maltose. There are other serous glands on the surface of the tongue that encircletaste budson the back part of the tongue and these also produce linguallipase.Lipase is adigestive enzymethat catalyses thehydrolysisoflipids(fats). These glands are termedVon Ebner's glandswhich have also been shown to have another function in the secretion ofhistatinswhich offer an early defense (outside of the immune system) against microbes in food, when it makes contact with these glands on the tongue tissue.[11][13]Sensory information can stimulate the secretion of saliva providing the necessary fluid for the tongue to work with and also to ease swallowing of the food.
Saliva
Salivamoistens and softens food, and along with the chewing action of the teeth, transforms the food into a smoothbolus.The bolus is further helped by the lubrication provided by the saliva in its passage from the mouth into the esophagus. Also of importance is the presence in saliva of the digestive enzymes amylase and lipase. Amylase starts to work on thestarchincarbohydrates,breaking it down into the simplesugarsofmaltoseanddextrosethat can be further broken down in the small intestine. Saliva in the mouth can account for 30% of this initial starch digestion. Lipase starts to work on breaking downfats.Lipase is further produced in the pancreas where it is released to continue this digestion of fats. The presence of salivary lipase is of prime importance in young babies whose pancreatic lipase has yet to be developed.[14]
As well as its role in supplying digestive enzymes, saliva has a cleansing action for the teeth and mouth.[15]It also has animmunologicalrole in supplying antibodies to the system, such asimmunoglobulin A.[16]This is seen to be key in preventinginfectionsof the salivary glands, importantly that ofparotitis.
Saliva also contains a glycoprotein calledhaptocorrinwhich is a binding protein to vitamin B12.[17]It binds with the vitamin in order to carry it safely through the acidic content of the stomach. When it reaches the duodenum, pancreatic enzymes break down the glycoprotein and free the vitamin which then binds withintrinsic factor.
Tongue
Food enters the mouth where the first stage in the digestive process takes place, with the action of thetongueand the secretion of saliva. The tongue is a fleshy andmuscularsensory organ,and the first sensory information is received via the taste buds in thepapillaeon its surface. If the taste is agreeable, the tongue will go into action, manipulating the food in the mouth which stimulates the secretion of saliva from the salivary glands. The liquid quality of the saliva will help in the softening of the food and its enzyme content will start to break down the food whilst it is still in the mouth. The first part of the food to be broken down is the starch of carbohydrates (by the enzyme amylase in the saliva).
The tongue is attached to the floor of the mouth by a ligamentous band called thefrenum[5]and this gives it great mobility for the manipulation of food (andspeech); the range of manipulation is optimally controlled by the action of several muscles and limited in its external range by the stretch of the frenum. The tongue's two sets of muscles, are fourintrinsic musclesthat originate in the tongue and are involved with its shaping, and fourextrinsic musclesoriginating in bone that are involved with its movement.
Taste
Tasteis a form ofchemoreceptionthat takes place in the specialisedtaste receptors,contained in structures calledtaste budsin the mouth. Taste buds are mainly on the upper surface (dorsum) of the tongue. The function of taste perception is vital to help prevent harmful or rotten foods from being consumed. There are also taste buds on theepiglottisand upper part of theesophagus.The taste buds are innervated by a branch of the facial nerve thechorda tympani,and theglossopharyngeal nerve.Taste messages are sent via thesecranial nervesto thebrain.The brain can distinguish between the chemical qualities of the food. The fivebasic tastesare referred to as those ofsaltiness,sourness,bitterness,sweetness,andumami.The detection of saltiness and sourness enables the control of salt and acid balance. The detection of bitterness warns of poisons—many of a plant's defences are of poisonous compounds that are bitter. Sweetness guides to those foods that will supply energy; the initial breakdown of the energy-giving carbohydrates by salivary amylase creates the taste of sweetness since simple sugars are the first result. The taste of umami is thought to signal protein-rich food. Sour tastes are acidic which is often found in bad food. The brain has to decide very quickly whether the food should be eaten or not. It was the findings in 1991, describing the firstolfactoryreceptors that helped to prompt the research into taste. The olfactory receptors are located on cell surfaces in thenosewhich bind to chemicals enabling the detection of smells. It is assumed that signals from taste receptors work together with those from the nose, to form an idea of complex food flavours.[18]
Teeth
Teethare complex structures made of materials specific to them. They are made of a bone-like material calleddentin,which is covered by the hardest tissue in the body—enamel.[8]Teeth have different shapes to deal with different aspects ofmasticationemployed in tearing and chewing pieces of food into smaller and smaller pieces. This results in a much larger surface area for the action of digestive enzymes. The teeth are named after their particular roles in the process of mastication—incisorsare used for cutting or biting off pieces of food;canines,are used for tearing,premolarsandmolarsare used for chewing and grinding. Mastication of the food with the help of saliva and mucus results in the formation of a soft bolus which can then beswallowedto make its way down theupper gastrointestinal tractto the stomach.[19] The digestive enzymes in saliva also help in keeping the teeth clean by breaking down any lodged food particles.[20][15]
Epiglottis
Theepiglottisis a flap ofelastic cartilageattached to the entrance of thelarynx.It is covered with a mucous membrane and there are taste buds on its lingual surface which faces into the mouth.[21]Its laryngeal surface faces into the larynx. The epiglottis functions to guard the entrance of theglottis,the opening between thevocal folds.It is normally pointed upward during breathing with its underside functioning as part of the pharynx, but during swallowing, the epiglottis folds down to a more horizontal position, with its upper side functioning as part of the pharynx. In this manner it prevents food from going into the trachea and instead directs it to the esophagus, which is behind. During swallowing, the backward motion of the tongue forces the epiglottis over the glottis' opening to prevent any food that is being swallowed from entering the larynx which leads to the lungs; the larynx is also pulled upwards to assist this process. Stimulation of the larynx by ingested matter produces a strongcough reflexin order to protect the lungs.
Pharynx
Thepharynxis a part of theconducting zoneof therespiratory systemand also a part of the digestive system. It is the part of the throat immediately behind thenasal cavityat the back of the mouth and above the esophagus andlarynx.The pharynx is made up of three parts. The lower two parts—theoropharynxand thelaryngopharynxare involved in the digestive system. The laryngopharynx connects to the esophagus and it serves as a passageway for both air and food. Air enters the larynx anteriorly but anything swallowed has priority and the passage of air is temporarily blocked. The pharynx is innervated by thepharyngeal plexus of the vagus nerve.[10]: 1465 Muscles in the pharynxpush the food into the esophagus. The pharynx joins the esophagus at the oesophageal inlet which is located behind thecricoid cartilage.
Esophagus
Theesophagus,commonly known as the foodpipe or gullet, consists of a muscular tube through which food passes from the pharynx to the stomach. The esophagus is continuous with the laryngopharynx. It passes through the posteriormediastinumin thethoraxand enters thestomachthrough a hole in thethoracic diaphragm—theesophageal hiatus,at the level of the tenththoracic vertebra(T10). Its length averages 25 cm, varying with an individual's height. It is divided into cervical,thoracicandabdominalparts. The pharynx joins the esophagus at the esophageal inlet which is behind thecricoid cartilage.
At rest the esophagus is closed at both ends, by theupper and lower esophageal sphincters.The opening of the upper sphincter is triggered by theswallowing reflexso that food is allowed through. The sphincter also serves to prevent back flow from the esophagus into the pharynx. The esophagus has a mucous membrane and the epithelium which has a protective function is continuously replaced due to the volume of food that passes inside the esophagus. During swallowing, food passes from the mouth through the pharynx into the esophagus. The epiglottis folds down to a more horizontal position to direct the food into the esophagus, and away from thetrachea.
Once in the esophagus, the bolus travels down to the stomach via rhythmic contraction and relaxation of muscles known asperistalsis.The lower esophageal sphincter is a muscular sphincter surrounding the lower part of the esophagus. Thegastroesophageal junctionbetween the esophagus and the stomach is controlled by the lower esophageal sphincter, which remains constricted at all times other than during swallowing and vomiting to prevent the contents of the stomach from entering the esophagus. As the esophagus does not have the same protection from acid as the stomach, any failure of this sphincter can lead to heartburn.
Diaphragm
Thediaphragmis an important part of the body's digestive system. The muscular diaphragm separates thethoracic cavityfrom theabdominal cavitywhere most of the digestive organs are located. Thesuspensory muscleattaches the ascending duodenum to the diaphragm. This muscle is thought to be of help in the digestive system in that its attachment offers a wider angle to theduodenojejunal flexurefor the easier passage of digesting material. The diaphragm also attaches to, and anchors the liver at itsbare area.The esophagus enters the abdomen through ahole in the diaphragmat the level ofT10.
Stomach
Thestomachis a major organ of the gastrointestinal tract and digestive system. It is a consistently J-shaped organ joined to the esophagus at its upper end and to the duodenum at its lower end. Gastric acid(informallygastric juice), produced in the stomach plays a vital role in the digestive process, and mainly containshydrochloric acidandsodium chloride.Apeptide hormone,gastrin,produced byG cellsin thegastric glands,stimulates the production of gastric juice which activates the digestive enzymes.Pepsinogenis a precursor enzyme (zymogen) produced by thegastric chief cells,and gastric acid activates this to the enzymepepsinwhich begins the digestion ofproteins.As these two chemicals would damage the stomach wall, mucus is secreted by innumerable gastric glands in the stomach, to provide a slimy protective layer against the damaging effects of the chemicals on the inner layers of the stomach.
At the same time that protein is being digested, mechanical churning occurs through the action of peristalsis, waves of muscular contractions that move along the stomach wall. This allows the mass of food to further mix with the digestive enzymes.Gastric lipasesecreted by the chief cells in the fundic glands in the gastric mucosa of the stomach, is an acidic lipase, in contrast with the alkaline pancreatic lipase. This breaks down fats to some degree though is not as efficient as the pancreatic lipase.
Thepylorus,the lowest section of the stomach which attaches to theduodenumvia thepyloric canal,contains countless glands which secrete digestive enzymes including gastrin. After an hour or two, a thick semi-liquid calledchymeis produced. When thepyloric sphincter,or valve opens, chyme enters the duodenum where it mixes further with digestive enzymes from the pancreas, and then passes through the small intestine, where digestion continues.
Theparietal cellsin the fundus of the stomach, produce a glycoprotein called intrinsic factor which is essential for the absorption ofvitamin B12.Vitamin B12 (cobalamin), is carried to, and through the stomach, bound to a glycoprotein secreted by the salivary glands –transcobalamin Ialso called haptocorrin, which protects the acid-sensitive vitamin from the acidic stomach contents. Once in the more neutral duodenum, pancreatic enzymes break down the protective glycoprotein. The freed vitamin B12 then binds to intrinsic factor which is then absorbed by the enterocytes in the ileum.
The stomach is a distensible organ and can normally expand to hold about one litre of food.[22]This expansion is enabled by a series ofgastric foldsin the inner walls of the stomach. The stomach of a newborn baby will only be able to expand to retain about 30 ml.
Spleen
Thespleenis the largest lymphoid organ in the body but has other functions.[23]It breaks down both red and whiteblood cellsthat arespent.This is why it is sometimes known as the 'graveyard of red blood cells'.[23]A product of thisdigestionis the pigmentbilirubin,which is sent to theliverand secreted in thebile.Another product isiron,which is used in the formation of new blood cells in thebone marrow.[5]Medicinetreats the spleen solely as belonging to thelymphatic system,though it is acknowledged that the full range of its important functions is not yet understood.[10]: 1751
Liver
Theliveris the second largest organ (after theskin) and is an accessory digestive gland which plays a role in the body'smetabolism.The liver has many functions some of which are important to digestion. The liver can detoxify variousmetabolites;synthesise proteins and producebiochemicalsneeded for digestion. It regulates the storage ofglycogenwhich it can form fromglucose(glycogenesis). The liver can also synthesise glucose from certainamino acids.Its digestive functions are largely involved with the breaking down of carbohydrates. It also maintains protein metabolism in its synthesis and degradation. In lipid metabolism it synthesisescholesterol.Fats are also produced in the process oflipogenesis.The liver synthesises the bulk of lipoproteins. The liver is located in the upper right quadrant of the abdomen and below the diaphragm to which it is attached at one part, the bare area of the liver. This is to the right of the stomach and it overlies the gall bladder. The liver synthesisesbile acidsandlecithinto promote the digestion of fat.[24]
Bile
Bileproduced by the liver is made up of water (97%),bile salts,mucus andpigments,1% fats and inorganic salts.[25]Bilirubinis its major pigment. Bile acts partly as asurfactantwhich lowers the surface tension between either two liquids or a solid and a liquid and helps toemulsifythe fats in the chyme. Food fat is dispersed by the action of bile into smaller units calledmicelles.The breaking down into micelles creates a much larger surface area for the pancreatic enzyme, lipase to work on. Lipase digests thetriglycerideswhich are broken down into twofatty acidsand amonoglyceride.These are then absorbed byvillion the intestinal wall. If fats are not absorbed in this way in the small intestine problems can arise later in the large intestine which is not equipped to absorb fats. Bile also helps in the absorption ofvitamin Kfrom the diet. Bile is collected and delivered through thecommon hepatic duct.This duct joins with thecystic ductto connect in acommon bile ductwith the gallbladder. Bile is stored in the gallbladder for release when food is discharged into the duodenum and also after a few hours.[5]
Gallbladder
Thegallbladderis a hollow part of thebiliary tractthat sits just beneath the liver, with the gallbladder body resting in a small depression.[26]It is a small organ where the bile produced by the liver is stored, before being released into the small intestine. Bile flows from the liver through thebile ductsand into the gall bladder for storage. The bile is released in response tocholecystokinin(CCK), a peptide hormone released from the duodenum. The production of CCK (by endocrine cells of the duodenum) is stimulated by the presence of fat in the duodenum.[27]
It is divided into three sections, a fundus, body and neck. The neck tapers and connects to the biliary tract via thecystic duct,which then joins the common hepatic duct to form the common bile duct. At this junction is a mucosal fold calledHartmann's pouch,wheregallstonescommonly get stuck. Themuscular layerof the body is of smooth muscle tissue that helps the gallbladder contract, so that it can discharge its bile into the bile duct. The gallbladder needs to store bile in a natural, semi-liquid form at all times.Hydrogen ionssecreted from the inner lining of the gallbladder keep the bile acidic enough to prevent hardening. To dilute the bile, water andelectrolytesfrom the digestion system are added. Also, salts attach themselves to cholesterol molecules in the bile to keep them fromcrystallising.If there is too much cholesterol or bilirubin in the bile, or if the gallbladder does not empty properly the systems can fail. This is how gallstones form when a small piece of calcium gets coated with either cholesterol or bilirubin and the bile crystallises and forms a gallstone. The main purpose of the gallbladder is to store and release bile, orgall.Bile is released into the small intestine in order to help in the digestion of fats by breaking down larger molecules into smaller ones. After the fat is absorbed, the bile is also absorbed and transported back to the liver for reuse.
Pancreas
Thepancreasis a major organ functioning as an accessory digestive gland in the digestive system. It is both anendocrine glandand anexocrine gland.[28]The endocrine part secretesinsulinwhen theblood sugarbecomes high; insulin moves glucose from the blood into the muscles and other tissues for use as energy. The endocrine part releasesglucagonwhen the blood sugar is low; glucagon allows stored sugar to be broken down into glucose by the liver in order to re-balance the sugar levels. The pancreas produces and releases important digestive enzymes in thepancreatic juicethat it delivers to the duodenum.[24]The pancreas lies below and at the back of the stomach. It connects to the duodenum via thepancreatic ductwhich it joins near to the bile duct's connection where both the bile and pancreatic juice can act on the chyme that is released from the stomach into the duodenum. Aqueous pancreatic secretions frompancreatic duct cellscontainbicarbonateions which are alkaline and help with the bile to neutralise the acidic chyme that is churned out by the stomach.
The pancreas is also the main source of enzymes for the digestion of fats and proteins. Some of these are released in response to the production of cholecystokinin in the duodenum. (The enzymes that digest polysaccharides, by contrast, are primarily produced by the walls of the intestines.) The cells are filled with secretory granules containing the precursor digestive enzymes. The majorproteases,the pancreatic enzymes which work on proteins, aretrypsinogenandchymotrypsinogen.Elastaseis also produced. Smaller amounts of lipase and amylase are secreted. The pancreas also secretesphospholipase A2,lysophospholipase,and cholesterolesterase.The precursorzymogens,are inactive variants of the enzymes; which avoids the onset ofpancreatitiscaused by autodegradation. Once released in the intestine, the enzymeenteropeptidasepresent in the intestinal mucosa activates trypsinogen by cleaving it to form trypsin; further cleavage results in chymotripsin.
Lower gastrointestinal tract
The lower gastrointestinal tract (GI), includes thesmall intestineand all of thelarge intestine.[29]The intestine is also called the bowel or the gut. The lower GI starts at the pyloric sphincter of the stomach and finishes at the anus. The small intestine is subdivided into theduodenum,thejejunumand theileum.The cecum marks the division between the small and large intestine. The large intestine includes the rectum andanal canal.[2]
Small intestine
Partially digested food starts to arrive in thesmall intestineas semi-liquidchyme,one hour after it is eaten.[citation needed]The stomach is half empty after an average of 1.2 hours.[30]After four or five hours the stomach has emptied.[31]
In the small intestine, thepHbecomes crucial; it needs to be finely balanced in order to activate digestive enzymes. The chyme is very acidic, with a low pH, having been released from the stomach and needs to be made much more alkaline. This is achieved in theduodenumby the addition of bile from the gall bladder combined with thebicarbonatesecretions from the pancreatic duct and also from secretions of bicarbonate-rich mucus from duodenal glands known asBrunner's glands.The chyme arrives in the intestines having been released from the stomach through the opening of thepyloric sphincter.The resulting alkaline fluid mix neutralises the gastric acid which would damage the lining of the intestine. The mucus component lubricates the walls of the intestine.
When the digested food particles are reduced enough in size and composition, they can be absorbed by the intestinal wall and carried to the bloodstream. The first receptacle for this chyme is theduodenal bulb.From here it passes into the first of the three sections of the small intestine, the duodenum (the next section is thejejunumand the third is theileum). The duodenum is the first and shortest section of the small intestine. It is a hollow, jointed C-shaped tube connecting the stomach to the jejunum. It starts at the duodenal bulb and ends at thesuspensory muscle of duodenum.The attachment of the suspensory muscle to the diaphragm is thought to help the passage of food by making a wider angle at its attachment.
Most food digestion takes place in the small intestine.Segmentation contractionsact to mix and move the chyme more slowly in the small intestine allowing more time for absorption (and these continue in the large intestine). In the duodenum, pancreatic lipase is secreted together with aco-enzyme,colipaseto further digest the fat content of the chyme. From this breakdown, smaller particles of emulsified fats calledchylomicronsare produced. There are also digestive cells calledenterocyteslining the intestines (the majority being in the small intestine). They are unusual cells in that they havevillion their surface which in turn have innumerablemicrovillion their surface. All these villi make for a greater surface area, not only for the absorption of chyme but also for its further digestion by large numbers of digestive enzymes present on the microvilli.
The chylomicrons are small enough to pass through the enterocyte villi and into theirlymphcapillaries calledlacteals.A milky fluid calledchyle,consisting mainly of the emulsified fats of the chylomicrons, results from the absorbed mix with the lymph in the lacteals.[clarification needed]Chyle is then transported through thelymphatic systemto the rest of the body.
The suspensory muscle marks the end of the duodenum and the division between the upper gastrointestinal tract and the lower GI tract. The digestive tract continues as the jejunum which continues as the ileum. The jejunum, the midsection of the small intestine containscircular folds,flaps of doubled mucosal membrane which partially encircle and sometimes completely encircle thelumenof the intestine. These folds together with villi serve to increase the surface area of the jejunum enabling an increased absorption of digested sugars, amino acids and fatty acids into the bloodstream. The circular folds also slow the passage of food giving more time for nutrients to be absorbed.
The last part of the small intestine is the ileum. This also contains villi andvitamin B12;bile acids and any residue nutrients are absorbed here. When the chyme is exhausted of its nutrients the remaining waste material changes into the semi-solids calledfeces,which pass to the large intestine, where bacteria in thegut florafurther break down residual proteins and starches.[32]
Transit time through the small intestine is an average of 4 hours. Half of the food residues of a meal have emptied from the small intestine by an average of 5.4 hours after ingestion. Emptying of the small intestine is complete after an average of 8.6 hours.[30]
Cecum
Thececumis a pouch marking the division between the small intestine and the large intestine. It lies below theileocecal valvein thelower right quadrantof the abdomen.[33]The cecum receives chyme from the last part of the small intestine, theileum,and connects to theascending colonof the large intestine. At this junction there is a sphincter or valve, the ileocecal valve which slows the passage of chyme from the ileum, allowing further digestion. It is also the site of theappendixattachment.[33]
Large intestine
In thelarge intestine,[2]the passage of the digesting food in thecolonis a lot slower, taking from 30 to 40 hours until it is removed bydefecation.[31]The colon mainly serves as a site for the fermentation of digestible matter by thegut flora.The time taken varies considerably between individuals. The remaining semi-solid waste is termedfecesand is removed by the coordinated contractions of the intestinal walls, termedperistalsis,which propels theexcretaforward to reach therectumand exit through theanusvia defecation. The wall has an outer layer of longitudinal muscles, thetaeniae coli,and an inner layer of circular muscles. The circular muscle keeps the material moving forward and also prevents any back flow of waste. Also of help in the action of peristalsis is thebasal electrical rhythmthat determines the frequency of contractions.[34]The taeniae coli can be seen and are responsible for the bulges (haustra) present in the colon. Most parts of the GI tract are covered withserous membranesand have amesentery.Other more muscular parts are lined withadventitia.
Blood supply
The digestive system is supplied by theceliac artery.The celiac artery is the first major branch from theabdominal aorta,and is the only major artery that nourishes the digestive organs.
There are three main divisions – theleft gastric artery,thecommon hepatic arteryand thesplenic artery.
The celiac artery supplies the liver, stomach, spleen and the upper 1/3 of the duodenum (to thesphincter of Oddi) and the pancreas with oxygenated blood. Most of the blood is returned to the liver via theportal venous systemfor further processing and detoxification before returning to thesystemic circulationvia thehepatic veins.
The next branch from the abdominal aorta is thesuperior mesenteric artery,which supplies the regions of the digestive tract derived from the midgut, which includes the distal 2/3 of the duodenum, jejunum, ileum, cecum, appendix, ascending colon, and the proximal 2/3 of the transverse colon.
The final branch which is important for the digestive system is theinferior mesenteric artery,which supplies the regions of the digestive tract derived from the hindgut, which includes the distal 1/3 of the transverse colon, descending colon, sigmoid colon, rectum, and the anus above thepectinate line.
Blood flow to the digestive tract reaches its maximum 20–40 minutes after a meal and lasts for 1.5–2 hours.[35]
Nerve supply
Theenteric nervous systemconsists of some one hundred millionneurons[36]that are embedded in theperitoneum,the lining of thegastrointestinal tractextending from the esophagus to the anus.[37]These neurons are collected into twoplexuses– themyenteric (or Auerbach's) plexusthat lies between the longitudinal and the smooth muscle layers, and thesubmucosal (or Meissner's) plexusthat lies between the circular smooth muscle layer and the mucosa.[38][39][40]
Parasympathetic innervationto theascending colonis supplied by thevagus nerve.Sympathetic innervationis supplied by thesplanchnic nervesthat join theceliac ganglia.Most of the digestive tract is innervated by the two large celiac ganglia, with the upper part of each ganglion joined by thegreater splanchnic nerveand the lower parts joined by thelesser splanchnic nerve.It is from these ganglia that many of thegastric plexusesarise.
Development
Early inembryonic development,theembryohas threegerm layersand abuts ayolk sac.During the second week of development, the embryo grows and begins to surround and envelop portions of this sac. The enveloped portions form the basis for the adult gastrointestinal tract. Sections of thisforegutbegin to differentiate into the organs of the gastrointestinal tract, such as the esophagus, stomach, and intestines.[41]
During the fourth week of development, the stomach rotates. The stomach, originally lying in the midline of the embryo, rotates so that its body is on the left. This rotation also affects the part of the gastrointestinal tube immediately below the stomach, which will go on to become the duodenum. By the end of the fourth week, the developing duodenum begins to spout a small outpouching on its right side, thehepatic diverticulum,which will go on to become thebiliary tree.Just below this is a second outpouching, known as thecystic diverticulum,that will eventually develop into the gallbladder.[41]
Clinical significance
Each part of the digestive system is subject to a wide range of disorders many of which can becongenital.Mouth diseasescan also be caused bypathogenicbacteria,viruses,fungiand as a side effect of somemedications.Mouth diseases includetongue diseasesandsalivary gland diseases.A commongumdisease in the mouth isgingivitiswhich is caused by bacteria inplaque.The most common viral infection of the mouth isgingivostomatitiscaused byherpes simplex.A commonfungalinfection iscandidiasiscommonly known asthrushwhich affects themucous membranesof the mouth.
There are a number ofesophageal diseasessuch as the development ofSchatzki ringsthat can restrict the passageway, causing difficulties in swallowing. They can also completely block the esophagus.[42]
Stomach diseasesare often chronic conditions and includegastroparesis,gastritis,andpeptic ulcers.
A number of problems includingmalnutritionandanemiacan arise frommalabsorption,the abnormal absorption of nutrients in the GI tract. Malabsorption can have many causes ranging frominfection,to enzyme deficiencies such asexocrine pancreatic insufficiency.It can also arise as a result of other gastrointestinal diseases such ascoeliac disease.Coeliac disease is anautoimmunedisorder of the small intestine. This can causevitamin deficienciesdue to the improper absorption of nutrients in the small intestine. The small intestine can also beobstructedby avolvulus,a loop of intestine that becomes twisted enclosing its attachedmesentery.This can causemesenteric ischemiaif severe enough.
A common disorder of the bowel isdiverticulitis.Diverticulaare small pouches that can form inside the bowel wall, which can become inflamed to give diverticulitis. This disease can have complications if an inflamed diverticulum bursts and infection sets in. Any infection can spread further to the lining of the abdomen (peritoneum) and cause potentially fatalperitonitis.[43]
Crohn's diseaseis a common chronicinflammatory bowel disease(IBD), which can affect any part of the GI tract,[44]but it mostly starts in theterminal ileum.
Ulcerative colitis,an ulcerative form ofcolitis,is the other major inflammatory bowel disease which is restricted to the colon and rectum. Both of these IBDs can give an increased risk of the development ofcolorectal cancer.Ulcerative colitis is the most common of the IBDs[45]
Irritable bowel syndrome(IBS) is the most common of thefunctional gastrointestinal disorders.These areidiopathicdisorders that theRome processhas helped to define.[46]
Giardiasisis a disease of the small intestine caused by aprotistparasiteGiardia lamblia.This does not spread but remains confined to the lumen of the small intestine.[47]It can often beasymptomatic,but as often can be indicated by a variety of symptoms. Giardiasis is the most commonpathogenicparasitic infectionin humans.[48]
There are diagnostic tools mostly involving the ingestion ofbarium sulphateto investigate disorders of the GI tract.[49]These are known asupper gastrointestinal seriesthat enableimagingof the pharynx, larynx, oesophagus, stomach and small intestine[50]andlower gastrointestinal seriesfor imaging of the colon.
In pregnancy
Gestationcan predispose for certain digestive disorders.Gestational diabetescan develop in the mother as a result ofpregnancyand while this often presents with few symptoms it can lead topre-eclampsia.[51]
History
In the early 11th century, the Islamic medical philosopherAvicennawrote extensively on many subjects including medicine. Forty of these treatises on medicine survive, and in the most famous one titled theCanon of Medicinehe discusses "rising gas". Avicenna believed that digestive system dysfunction was responsible for the overproduction of gas in the gastrointestinal tract. He suggested lifestyle changes and a compound of herbal drugs for its treatment.[52]
In 1497,Alessandro Benedettiviewed the stomach as an unclean organ separated off by the diaphragm. This view of the stomach and intestines as being base organs was generally held until the mid-17th century.[53]
In the Renaissance of the 16th century,Leonardo da Vinciproduced some early drawings of the stomach and intestines. He thought that the digestive system aided the respiratory system.[53]Andreas Vesaliusprovided some early anatomical drawings of the abdominal organs in the 16th century.
In the middle of the 17th century, a Flemish physicianJan Baptist van Helmontoffered the firstchemical account of digestionwhich was later described as being very close to the later conceptualised enzyme.[53]
In 1653,William Harveydescribed the intestines in terms of their length, their blood supply, the mesenteries, and fat (adenylyl cyclase).[53]
In 1823,William Proutdiscoveredhydrochloric acidin the gastric juice.[54]In 1895,Ivan Pavlovdescribed its secretion as being stimulated by a neurologic reflex with thevagus nervehaving a crucial role. Black in the 19th century suggested an association of histamine with this secretion. In 1916, Popielski described histamine as a gastric secretagogue of hydrochloric acid.
William Beaumontwas an army surgeon who in 1825, was able to observe digestion as it took place in the stomach.[55]This was made possible by experiments on a man with a stomach wound that did not fully heal leaving an opening into the stomach. The churning motion of the stomach was described among other findings.[53]
In the 19th century, it was accepted that chemical processes were involved in the process of digestion.Physiological researchinto secretion and the gastrointestinal tract was pursued with experiments undertaken by Claude Bernard, Rudolph Heidenhain and Ivan Pavlov.
The rest of the 20th century was dominated by research into enzymes. The first to be discovered wassecretinbyErnest Starlingin 1902, with ensuing results from John Edkins in 1905 who first suggestedgastrinwith its structure being determined in 1964.[54]Andre Latarjet and Lester Dragstedt found a role foracetylcholinein the digestive system.[54]In 1972,H2 receptor agonistswere described by J. Black, that block the action of histamine and decrease the production of hydrochloric acid. In 1980,proton pump inhibitorswere described by Sachs. In 1983, the role ofHelicobacter pyloriin the formation of ulcers was described byBarry Marshall,andRobin Warren.[56]
Art historians have often noted thatbanqueterson iconographic records of ancient Mediterranean societies almost always appear to be lying down on their left sides. One possible explanation could lie in the anatomy of the stomach and in the digestive mechanism. When lying on the left, the food has room to expand because the curvature of the stomach is enhanced in that position.[57]
See also
References
- ^Kong F, Singh RP (June 2008)."Disintegration of solid foods in human stomach".Journal of Food Science.73(5):R67 –R80.doi:10.1111/j.1750-3841.2008.00766.x.PMID18577009.
- ^abcd"Large intestine".Encyclopedia Britannica. 2016.Retrieved1 October2016.
- ^Hopkins J, Maton A, Charles WM, Susan J, Maryanna QW, David L, Jill DW (1993).Human Biology and Health.Englewood Cliffs, New Jersey, US: Prentice Hall.ISBN978-0-13-981176-0.
- ^Pocock G (2006).Human Physiology(Third ed.). Oxford University Press. p. 382.ISBN978-0-19-856878-0.
- ^abcdMacpherson G (1999).Black's Medical Dictionary.A & C. Black Ltd.ISBN978-0-7136-4566-8.
- ^Frenkel ES, Ribbeck K (January 2015)."Salivary mucins protect surfaces from colonization by cariogenic bacteria".Applied and Environmental Microbiology.81(1):332–338.Bibcode:2015ApEnM..81..332F.doi:10.1128/aem.02573-14.PMC4272720.PMID25344244.
- ^Nanci A, Ten Cate AR (2008).Ten Cate's Oral Histology: Development, Structure, and Function(7th ed.). St. Louis, Mo.: Mosby Elsevier. p. 321.ISBN978-0-323-04557-5.
- ^abBritannica Concise Encyclopedia.Encyclopedia Britannica, Inc. 2007.ISBN978-1-59339-293-2.
- ^Saladin K (2011).Human Anatomy.McGraw Hill. p. 659.ISBN978-0-07-122207-5.
- ^abcDorland WA (2012).Dorland's illustrated medical dictionary(32nd ed.). Philadelphia, PA: Saunders/Elsevier.ISBN978-1-4160-6257-8.
- ^abNanci A (2013).Ten Cate's Oral Histology: Development, Structure, and Function(8th ed.). St. Louis, Mo.: Elsevier. pp.275–276.ISBN978-0-323-07846-7.
- ^Illustrated Anatomy of the Head and Neck, Fehrenbach and Herring, Elsevier, 2012, p. 157
- ^Piludu M, Lantini MS, Cossu M, Piras M, Oppenheim FG, Helmerhorst EJ, et al. (November 2006). "Salivary histatins in human deep posterior lingual glands (of von Ebner)".Archives of Oral Biology.51(11):967–973.doi:10.1016/j.archoralbio.2006.05.011.PMID16859632.
- ^Maton A (1993-01-01).Human Biology and Health.Prentice Hall 1993.ISBN978-0-13-981176-0.
- ^abEdgar WM (April 1992). "Saliva: its secretion, composition and functions".British Dental Journal.172(8):305–312.doi:10.1038/sj.bdj.4807861.PMID1591115.S2CID205670543.
- ^Făgărășan S.;Honjo T. (January 2003). "Intestinal IgA synthesis: regulation of front-line body defences".Nature Reviews. Immunology.3(1):63–72.doi:10.1038/nri982.PMID12511876.S2CID2586305.
- ^Pettit JD, Moss P (2006).Essential Haematology(5e (Essential) ed.). Blackwell Publishing Professional. p. 44.ISBN978-1-4051-3649-5.
- ^Bradbury J (March 2004)."Taste perception: cracking the code".PLOS Biology.2(3): E64.doi:10.1371/journal.pbio.0020064.PMC368160.PMID15024416.
- ^Bowen R."Prehension, Mastication and Swallowing".Hypertexts for Biomedical Sciences.Archived fromthe originalon 12 December 2009 – via About.com.
- ^Fejerskov O, Kidd E, Nyvad B, Baelum V, eds. (2008).Dental caries: the disease and its clinical management(2nd ed.). Oxford: Blackwell Munksgaard.ISBN978-1-4051-3889-5.
- ^Jowett A, Shrestha R (November 1998)."Mucosa and taste buds of the human epiglottis".Journal of Anatomy.193(4):617–618.doi:10.1046/j.1469-7580.1998.19340617.x.PMC1467887.PMID10029195.
- ^Sherwood L (1997).Human physiology: from cells to systems.Belmont, CA: Wadsworth Pub. Co.ISBN978-0-314-09245-8.OCLC35270048.
- ^abSaladin K (2011).Human Anatomy.McGraw Hill. pp.621–622.ISBN978-0-07-122207-5.
- ^abSaladin K (2011).Human Anatomy.McGraw Hill. pp.674–679.ISBN978-0-07-122207-5.
- ^Hall JE, Hall ME (2011).Guyton and Hall Textbook of Medical Physiology.U.S.: Saunders Elsevier. p. 784.ISBN978-1-4160-4574-8.
- ^Drake RL, Vogl W, Mitchell AW, Richardson P (2005).Gray's Anatomy for students.Philadelphia: Elsevier/Churchill Livingstone. p. 287.ISBN978-0-8089-2306-0.
- ^"Histology guide".Retrieved22 May2015.
- ^Ahrens T, Prentice D (1998).Critical care certification: preparation, review & practice exams.Norwalk, CT: Appleton & Lange. p. 265.ISBN978-0-8385-1474-0.
- ^Lower+Gastrointestinal+Tractat the U.S. National Library of MedicineMedical Subject Headings(MeSH)
- ^abRead NW, Al-Janabi MN, Holgate AM, Barber DC, Edwards CA (March 1986)."Simultaneous measurement of gastric emptying, small bowel residence and colonic filling of a solid meal by the use of the gamma camera".Gut.27(3):300–308.doi:10.1136/gut.27.3.300.PMC1433420.PMID3699551.
- ^abBowen R."Gastrointestinal Transit: How Long Does It Take?".Hypertexts for Biomedical Sciences.Colorado State University.RetrievedApril 1,2020.
- ^Cummings JH, Macfarlane GT (November 1997). "Role of intestinal bacteria in nutrient metabolism".Journal of Parenteral and Enteral Nutrition.21(6):357–365.doi:10.1177/0148607197021006357.PMID9406136.
- ^abSaladin K (2011).Human Anatomy.McGraw Hill. p. 672.ISBN978-0-07-122207-5.
- ^Wood JD (2009). "Gastrointestinal Physiology". In Rhoades RA, Bell DR (eds.).Medical Physiology: Principles for Clinical Medicine(3rd ed.). Philadelphia, PA: Lippincott Williams & Wilkins. pp.463–496.
- ^Waaler BA, Toska K (February 1999). "[Digestive system's large and changing needs of blood supply]".Tidsskrift for den Norske Laegeforening.119(5):664–666.PMID10095388.
- ^Boron WG, Boulpaep EL (2005).Medical Physiology.Elsevier Saunders. p. 883.ISBN978-1-4160-2328-9.
- ^Hall JE (2011). "General Principles of Gastrointestinal Function".Guyton and Hal Textbook of Medical Physiology(12th ed.). Saunders Elsevier. p. 755.ISBN978-1-4160-4574-8.
- ^Bowen R."The Enteric Nervous System".Hypertexts for Biomedical Sciences.Archived fromthe originalon 2019-01-20.Retrieved2008-11-29.
- ^Canning BJ, Spina D (5 August 2009).Sensory Nerves.Handbook of Experimental Pharmacology. Vol. 194. Springer. p. 341.ISBN978-3-540-79090-7.
- ^Costa M,Brookes SJ, Hennig GW (December 2000)."Anatomy and physiology of the enteric nervous system".Gut.47(Suppl 4): iv15-9, discussion iv26.doi:10.1136/gut.47.suppl_4.iv15.PMC1766806.PMID11076898.
- ^abSchoenwolf GC, Bleyl SB, Brauer PR, Francis-West PH (2009).Larsen's human embryology(4th Thoroughly rev. and updated ed.). Philadelphia: Churchill Livingstone/Elsevier. pp. Development of the Gastrointestinal Tract.ISBN978-0-443-06811-9.
- ^Cotran RS, Kumar V, Fausto N, Nelson F, Robbins SL, Abbas AK (2005).Robbins and Cotran pathologic basis of disease.St. Louis, Mo: Elsevier Saunders. p. 800.ISBN978-0-7216-0187-8.
- ^Morris AM, Regenbogen SE, Hardiman KM, Hendren S (January 2014). "Sigmoid diverticulitis: a systematic review".JAMA.311(3):287–297.doi:10.1001/jama.2013.282025.PMID24430321.
- ^"Crohn's Disease".National Digestive Diseases Information Clearinghouse (NDDIC).July 10, 2013. Archived fromthe originalon 9 June 2014.Retrieved12 June2014.
- ^Danese S, Fiocchi C (November 2011). "Ulcerative colitis".The New England Journal of Medicine.365(18):1713–1725.doi:10.1056/NEJMra1102942.PMID22047562.S2CID38073643.
- ^Thompson WG, Longstreth GL, Drossman DA, Heaton K, Irvine EJ, Muller-Lissner S (2000). "Functional Bowel Disorders.". In Drossman DA, Corazziari E, Talley NJ, et al. (eds.).Rome II: The Functional Gastrointestinal Disorders. Diagnosis, Pathophysiology and Treatment. A Multinational Consensus.Lawrence, KS: Allen Press.ISBN978-0-9656837-2-2.
- ^Weller PF (2015)."Protozoal Intestinal Infections and Trichomoniasi".In Kasper D, Fauci A, Hauser S, Longo D, Jameson JL, Loscalzo J (eds.).Harrison's Principles of Internal Medicine(19th ed.). McGraw-Hill.
- ^Esch KJ, Petersen CA (January 2013)."Transmission and epidemiology of zoonotic protozoal diseases of companion animals".Clinical Microbiology Reviews.26(1):58–85.doi:10.1128/CMR.00067-12.PMC3553666.PMID23297259.
- ^Boland GW (2013).Gastrointestinal imaging: the requisites(4th ed.). Philadelphia: Elsevier/Saunders.ISBN978-0-323-10199-8.
- ^British Medical Association (2013).BMA Illustrated Medical Dictionary.Dorling Kindersley Ltd.ISBN978-1-4093-4966-2.
- ^Mack LR, Tomich PG (June 2017). "Gestational Diabetes: Diagnosis, Classification, and Clinical Care".Obstetrics and Gynecology Clinics of North America.44(2):207–217.doi:10.1016/j.ogc.2017.02.002.PMID28499531.
- ^Heydari M, Hashempur MH, Mosavat SH (23 November 2021)."Avicenna's diagnosis of Darwin's disease".Retrieved23 November2021.
- ^abcde"History of the Stomach and Intestines".web.stanford.edu.Retrieved10 November2021.
- ^abcSródka A (December 2003). "The short history of gastroenterology".Journal of Physiology and Pharmacology.54(Suppl 3):9–21.PMID15075462.
- ^Beaumont W."William Beaumont Papers (1812-1959)]"– via U.S. National Library of Medicine.
Beaumont is known as the father of gastric physiology. Photocopies of originals held atWashington University in St. LouisSchool of Medicine, Library--letters, notebooks, certificates, and related papers.
- ^Marshall BJ, Warren JR (June 1984). "Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration".Lancet.1(8390):1311–1315.doi:10.1016/S0140-6736(84)91816-6.PMID6145023.S2CID10066001.
- ^Mazzarello P, Harari M (2007-08-15)."Left to digest".Nature.448(7155): 753.doi:10.1038/448753a.ISSN1476-4687.