Anitch(also known aspruritus) is asensationthat causes a strong desire orreflex to scratch.[1]Itches have resisted many attempts to be classified as any one type ofsensoryexperience. Itches have many similarities topain,and while both are unpleasant sensory experiences, their behavioral response patterns are different. Pain creates awithdrawal reflex,whereas itches leads to ascratch reflex.[2]
| Itch | |
|---|---|
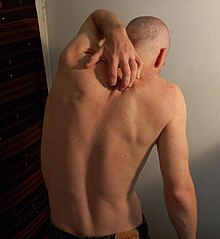 | |
| A man scratching his back | |
| Specialty | Dermatology |
| Symptoms | Compulsion to scratchan irritated area of skin |
| Causes | Certain infections, allergies, blood derangements and environmental factors |
| Risk factors | Dry skin |
| Diagnostic method | Often based on the causes of itching |
| Differential diagnosis | Pain |
| Treatment | Antipruritics,phototherapy |
Unmyelinatednerve fibersfor itches and pain both originate in theskin.Information for them is conveyed centrally in two distinct systems that both use the samenervebundle andspinothalamic tract.[3]
Classification
editMost commonly, an itch is felt in one place. If it is felt all over the body, then it is calledgeneralized itchorgeneralized pruritus.[4]Generalized itch is infrequently a symptom of a serious underlying condition, such as cholestatic liver disease.
If the sensation of itching persists for six weeks or longer, then it is calledchronic itchorchronic pruritus.[4][5]Chronic idiopathic pruritusorChronic Pruritus of Unknown Originis a form of itch that persists for longer than six weeks, and for whichno clear cause can be identified.[6][7]
Signs and symptoms
editPain and itch have very different behavioral response patterns. Pain elicits a withdrawal reflex, which leads to retraction and therefore a reaction trying to protect an endangered part of the body. Itch in contrast creates ascratch reflex,which draws one to the affected skin site. Itch generates stimulus of a foreign object underneath or upon the skin and also the urge to remove it. For example, responding to a local itch sensation is an effective way to remove insects from one's skin.
Scratching has traditionally been regarded as a way to relieve oneself by reducing the annoying itch sensation. However, there arehedonicaspects to scratching, as one would find noxious scratching highly pleasurable.[2]This can be problematic withchronicitch patients, such as ones withatopic dermatitis,who may scratch affected spots until they no longer produce a pleasant or painful sensation, instead of when the itch sensation disappears.[8]It has been hypothesized that motivational aspects of scratching include the frontal brain areas of reward and decision making. These aspects might therefore contribute to the compulsive nature of itch and scratching.[2]
Contagious itch
editEvents of "contagiousitch "are very common occurrences. Even a discussion on the topic of itch can give one the desire to scratch. Itch is likely to be more than a localized phenomenon in the place one scratches. Results from a study showed that itching and scratching were induced purely by visualstimuliin a public lecture on itching.[9]The sensation of pain can also be induced in a similar fashion, often by listening to a description of an injury, or viewing an injury itself.
There is little detailed data on central activation for contagious itching, but it is hypothesized that a humanmirror neuronsystem exists in which one imitates certain motor actions when they view others performing the same action. A similar hypothesis has been used to explain the cause of contagiousyawning.[2]
Itch inhibition due to pain
editStudies done in the last decade have shown that itch can be inhibited by many other forms of painful stimuli, such asnoxiousheat,[10]physical rubbing/scratching, noxious chemicals, andelectric shock.[11]
Causes
editInfectious
edit- Body louse,found in substandard living conditions
- Cutaneous larva migrans,a skin disease caused byhookworminfection
- Head lice,if limited to the neck and scalp
- Herpes,a viral disease
- Insect bites,such as those frommosquitosorchiggers
- Pubic lice,if limited to thegenital area
- Scabies,especially when several other persons in close contact also itch
- Shaving,which may irritate the skin
- Swimmer's itch,a short-term immune reaction
- Varicella– i.e. chickenpox, prevalent among young children and highly contagious
- Tungiasis,ectoparasite of skin
Environmental and allergic
edit- Allergic reactionto contact with specific chemicals, such asurushiol,derived frompoison ivyorpoison oak,orBalsam of Peru,found in many foods and fragrances.[12][13]Certain allergens may be diagnosed in apatch test.[14][15]
- Foreign objectson the skin are the most common cause of non-pathological itching.
- Photodermatitis–sunlightreacts with chemicals in the skin, leading to the formation of irritant metabolites.
- Urticaria(also calledhives) usually causes itching.
Dermatologic
edit- Dandruff,an unusually large amount of flaking is associated with this sensation.
- Punctate palmoplantar keratoderma,a group of disorders characterized by abnormal thickening of the palms and soles.
- Skin conditions(such aspsoriasis,eczema,seborrhoeic dermatitis,sunburn,athlete's foot,andhidradenitis suppurativa). Most are of an inflammatory nature.
- Scabhealing,scargrowth, and the development or emergence ofmoles,pimples,andingrown hairsfrom below the epidermis.
- Xerosis,dry skin, frequently seen in the winter and also associated with older age, frequent bathing in hot showers or baths, and high-temperature and low-humidity environments.
Other diseases
edit- Diabetes mellitus,a group of metabolic diseases in which a person has high blood sugar
- Hyperparathyroidism,overactivity of the parathyroid glands resulting in excess production of parathyroid hormone (PTH)[16]
- Iron deficiency anemia,a common anemia (low red blood cell or hemoglobin levels)
- Cholestasis,where bile acids leaking into the serum activate peripheral opioid receptors, resulting in the characteristic generalized, severe itching
- Malignancyor internal cancer, such aslymphomaorHodgkin's disease[17]
- Polycythemia,which can cause generalized itching due to increased histamines
- Psychiatricdisease ( "psychogenic itch",as may be seen indelusional parasitosis)
- Thyroidillness
- Uraemia– the itching sensation this causes is known asuremic pruritus
Medication
edit- Drugs (such asopioids) that activate histamine (H1) receptors or trigger histamine release
- Chloroquine,a drug used in the treatment and prevention ofmalaria
- Bile acidcongeners such as obeticholic acid
Related to pregnancy
edit- Gestational pemphigoid,a dermatosis of pregnancy
- Intrahepatic cholestasis of pregnancy,a medical condition in which cholestasis occurs
- Pruritic urticarial papules and plaques of pregnancy(PUPPP), a chronic hives-like rash
Other
edit- Menopause,or changes in hormonal balances associated with aging
- Terminal illness[18]
Mechanism
editItch can originate in theperipheral nervous system(dermalorneuropathic) or in thecentral nervous system(neuropathic,neurogenic,orpsychogenic).[19][20][21]
Pruritoceptive
editItch originating in the skin is known aspruritoceptive,and can be induced by a variety of stimuli, including mechanical, chemical, thermal, and electrical stimulation, or infection. The primaryafferent neuronsresponsible forhistamine-induced itch areunmyelinatedC-fibres.[1]
Nociceptors.Two major classes of humanC-fibrenociceptorsexist: mechano-responsivenociceptorsand mechano-insensitive nociceptors. Mechano-responsive nociceptors have been shown in studies to respond to mostly pain, and mechano-insensitive receptors respond mostly to itch induced by histamine. However, it does not explain mechanically induced itch or itch produced without aflarereaction that involves no histamine.[1]Therefore, it is possible that pruritoceptivenerve fibreshave different classes of fibres, which is unclear in current research.[2]
Histology and skin layers.Studies have been done to show that itch receptors are found only on the top twoskinlayers, theepidermisand the epidermal/dermaltransition layers.[citation needed]Shelley and Arthur verified the depth by injecting individual itch powder (Mucuna pruriens)spiculesand noting that maximal sensitivity occurred at thebasal cell layeror the innermost layer of the epidermis. Surgical removal of those skin layers removed the ability for a patient to perceive itch.[citation needed]Itch is never felt inmuscleor joints, which strongly suggests that deep tissue probably does not contain itch signaling apparatuses.[citation needed]
Sensitivity to pruritic stimuli is evenly distributed across the skin and has a clear spot distribution with similar density to that of pain. The different substances that elicit itch upon intracutaneous injection (injection within the skin) elicit only pain when injectedsubcutaneously(beneath the skin).[citation needed]
Molecular basis
editItch is often classified as that which is histamine mediated (histaminergic) and nonhistaminergic.
Itch is readily abolished in skin areas treated with nociceptorexcitotoxincapsaicinbut remains unchanged in skin areas rendered touch insensitive by pretreatment withanti-inflammatorysaponins.Although experimentally induced itch can still be perceived under a complete A-fiberconduction block,it is significantly diminished. Overall, itch sensation is mediated by A-delta and C nociceptors located in the uppermost layer of the skin.[22]
Gene expression.Using single-cell mRNA sequencing, clusters of genes expressed in itch-related tissues were identified, e.g. NP1-3, transmitting itch information; where NP3 expresses neuropeptidesNppbandSstas well as genes involved in inflammatory itch (Il31ra,Osmr andCrystrl2). The histamine receptor geneHrh1was found in NP2 and NP3, suggesting that histaminergic itch is transmitted by both these pruriceptive sub clusters.[23]
Infection.Staphylococcus aureus,a bacterial pathogen associated with itchy skin diseases, directly activates pruriceptor sensory neurons to drive itch. Skin exposure toS. aureuscauses robust itch and scratch-induced damage. This reaction is mediated byS. aureusserine protease V8 which cleaves proteinase-activated receptor 1 (PAR1) on mouse and human sensory neurons. Targeting PAR1 through genetic deficiency, small interfering RNA (siRNA) knockdown, or pharmacological blockade decreases itch and skin damage caused by V8 andS. aureusexposure.[24]
Spinal itch pathway
editAfter the pruriceptive primary afferent has been activated, the signal is transmitted from the skin into the spinal dorsal horn. In this area, a number of interneurons will either be inhibited or activated to promote activation of projection neurons, mediating the pruriceptive signal to the brain. The GRP-GRPR interneuron system has been found to be important for mediating both histaminergic and non-histaminergic itch, where the GRP neurons activate GRPR neurons to promote itch[25][26]
Neuropathic
editNeuropathic itch can originate at any point along the afferent pathway as a result of damage of thenervous system.They could include diseases or disorders in thecentral nervous systemorperipheral nervous system.[20]Examples of neuropathic itch in origin are notalgia paresthetica,brachioradial pruritus,brain tumors,multiple sclerosis,peripheral neuropathy,andnerve irritation.[27]
Neurogenic
editNeurogenic itch, which is itch induced centrally but with no neural damage, is mostly associated with increased accumulation of exogenousopioidsand possiblysyntheticopioids.[20]
Psychogenic
editItch is also associated with some symptoms ofpsychiatricdisorders such as tactilehallucinations,delusionsofparasitosis,orobsessive-compulsive disorders(as inOCD-relatedneuroticscratching).[20]
Peripheral sensitization
editInflammatorymediators—such asbradykinin,serotonin(5-HT) andprostaglandins—released during a painful or pruritic inflammatory condition not only activate pruriceptors but also causeacutesensitization of the nociceptors. In addition, expression of neuro growth factors (NGF) can cause structural changes innociceptors,such as sprouting. NGF is high in injured or inflamed tissue. Increased NGF is also found inatopic dermatitis,ahereditaryand non-contagious skin disease withchronicinflammation.[28]NGF is known to up-regulate neuropeptides, especiallysubstance P.Substance P has been found to have an important role in inducing pain; however, there is no confirmation that substance P directly causes acute sensitization. Instead, substance P may contribute to itch by increasingneuronalsensitization and may affect release ofmast cells,which contain many granules rich in histamine, during long-term interaction.[2]
Central sensitization
editNoxious input to thespinal cordis known to produce central sensitization, which consists ofallodynia,exaggeration of pain, and punctuatehyperalgesia,extreme sensitivity to pain. Two types of mechanical hyperalgesia can occur: 1) touch that is normally painless in the uninjured surroundings of a cut or tear can trigger painful sensations (touch-evoked hyperalgesia), and 2) a slightly painful pin prick stimulation is perceived as more painful around a focused area of inflammation (punctuate hyperalgesia). Touch-evoked hyperalgesia requires continuous firing of primary afferent nociceptors, and punctuatehyperalgesiadoes not require continuous firing which means it can persist for hours after atraumaand can be stronger than normally experienced. In addition, it was found that patients withneuropathicpain, histamineionophoresisresulted in a sensation of burning pain rather than itch, which would be induced in normal healthy patients. This shows that there is spinal hypersensitivity toC-fiberinput inchronicpain.[2]
Treatment
editA variety of over-the-counter and prescription anti-itch drugs are available. Some plant products have been found to be effective anti-pruritics, others not. Non-chemical remedies include cooling, warming, soft stimulation.
Topicalantipruritics in the form ofcreamsandspraysare often availableover-the-counter.Oralanti-itch drugs also exist and are usuallyprescription drugs.Theactive ingredientsusually belong to the following classes:
- Antihistamines,such asdiphenhydramine(Benadryl)[29]
- Corticosteroids,such ashydrocortisonetopical cream;seetopical steroid
- Counterirritants,such asmint oil,menthol,orcamphor[30]
- Crotamiton(trade name Eurax) is an antipruritic agent available as a cream or lotion, often used to treatscabies.Its mechanism of action remains unknown.
- JAK inhibitors,such asruxolitinibtopical cream;seetopical JAK inhibitor
- Local anesthetics,such asbenzocainetopical cream (Lanacane)
Phototherapyis helpful for severe itching, especially if caused bychronic kidney disease.The common type of light used isUVB.[31]
Sometimes scratching relieves isolated itches, hence the existence of devices such as theback scratcher.Often, however, scratching only offers temporary relief and can intensify itching, even causing further damage to the skin, dubbed the "itch-scratch cycle".[32]
The mainstay of therapy for dry skin is maintaining adequate skin moisture and topicalemollients.
No studies have been conducted to investigate the effectiveness of emollient creams, cooling lotions, topical corticosteroids, topical antidepressants, systemic antihistamines, systemic antidepressants, systemic anticonvulsants, and phototherapy on chronic pruritus of unknown origin.[29]However, there are clinical trials currently underway with dupilumab which is thought to alleviate itch by acting on the IL-4 receptor on sensory neurons.[33][34]The effectiveness of therapeutic options for people who are terminally ill with malignant cancer is not known.[18]
Epidemiology
editApproximately 280 million people globally, 4% of the population, have difficulty with itchiness.[35]This is comparable to the 2–3% of the population who havepsoriasis.
History
editIn 1660, German physicianSamuel Hafenrefferintroduced the definition of pruritus (itch).[36]
See also
edit- Feeling,a perceptual state of conscious experience.
- Formication,a sensation that resembles that of small insects crawling on or under the skin
- Pruritus ani(also known as anusitis), irritation of skin at the exit of the rectum (anus), causing the desire to scratch
- Referred itch,a phenomenon in which a stimulus applied in one region of the body is felt as an itch or irritation in a different part of the body
- Itching powder,a powder or powder-like substance that induces itching when applied onto human skin.
References
edit- ^abcAndersen HH, Elberling J, Arendt-Nielsen L (September 2015)."Human surrogate models of histaminergic and non-histaminergic itch".Acta Dermato-Venereologica.95(7): 771–777.doi:10.2340/00015555-2146.PMID26015312.
- ^abcdefgIkoma A, Steinhoff M, Ständer S, et al. (July 2006). "The neurobiology of itch".Nature Reviews. Neuroscience.7(7): 535–547.doi:10.1038/nrn1950.PMID16791143.S2CID9373105.
- ^Greaves MW, Khalifa N (October 2004). "Itch: more than skin deep".International Archives of Allergy and Immunology.135(2): 166–172.doi:10.1159/000080898.PMID15375326.S2CID13376216.
- ^abMolkara S, Sabourirad S, Molooghi K (July 2019)."Infectious differential diagnosis of chronic generalized pruritus without primary cutaneous lesions: a review of the literature".International Journal of Dermatology.59(1): 30–36.doi:10.1111/ijd.14587.PMID31364165.S2CID198998956.
- ^Harrison IP, Spada F (July 2019)."Breaking the Itch-Scratch Cycle: Topical Options for the Management of Chronic Cutaneous Itch in Atopic Dermatitis".Medicines.6(3): 76.doi:10.3390/medicines6030076.PMC6789602.PMID31323753.
- ^Erickson S, Nahmias Z, Rosman IS, Kim BS (July 2018). "Immunomodulating Agents as Antipruritics".Dermatologic Clinics.36(3): 325–334.doi:10.1016/j.det.2018.02.014.PMID29929604.S2CID49336771.
- ^Hinkle JL, Cheever KH (2018-08-30).Brunner and Suddarth's Textbook of Medical-Surgical Nursing.Wolters kluwer india Pvt Ltd. p. 1269.ISBN978-93-87963-72-6.Archivedfrom the original on 2023-09-23.Retrieved2022-07-02.
- ^Karsak M, Gaffal E, Date R, et al. (June 2007). "Attenuation of allergic contact dermatitis through the endocannabinoid system".Science.316(5830): 1494–1497.Bibcode:2007Sci...316.1494K.doi:10.1126/science.1142265.PMID17556587.S2CID37611370.
- ^[citation needed]
- ^Yosipovitch G, Fast K, Bernhard JD (December 2005)."Noxious heat and scratching decrease histamine-induced itch and skin blood flow".The Journal of Investigative Dermatology.125(6): 1268–1272.doi:10.1111/j.0022-202X.2005.23942.x.PMID16354198.
- ^Ward L, Wright E, McMahon SB (January 1996). "A comparison of the effects of noxious and innocuous counterstimuli on experimentally induced itch and pain".Pain.64(1): 129–138.doi:10.1016/0304-3959(95)00080-1.PMID8867255.S2CID25772165.
- ^Pfützner W, Thomas P, Niedermeier A, et al. (2003-02-20)."Systemic contact dermatitis elicited by oral intake of Balsam of Peru".Acta Dermato-Venereologica.83(4): 294–295.doi:10.1080/00015550310016599.PMID12926805.
- ^Usatine RP, Riojas M (August 2010)."Diagnosis and management of contact dermatitis".American Family Physician.82(3). Aafp.org: 249–255.PMID20672788.Archivedfrom the original on 2014-04-09.Retrieved2014-04-09.
- ^Byers JP (2006).Metalworking Fluids(Second ed.). CRC Press.ISBN142001773X.Archivedfrom the original on 2023-01-12.Retrieved2016-03-05.
- ^Feingold BF (1973). Byers JP (ed.).Introduction to clinical allergy.the University of Michigan.ISBN0398027978.Archivedfrom the original on 2023-01-12.Retrieved2020-06-24.
- ^LaBagnara, James.eMedicine –HyperparathyroidismArchived2008-12-02 at theWayback Machine.emedicine.com
- ^Jovičić, Sanja; Balaban, Jagoda; Gajanin, Vesna (2023-06-24)."Association of systemic diseases with chronic pruritus".Scripta Medica.54(2): 163–167.doi:10.5937/scriptamed54-43882.ISSN2490-3329.
- ^abBoehlke, Christopher; Joos, Lisa; Coune, Bettina; Becker, Carola; Meerpohl, Joerg J.; Buroh, Sabine; Hercz, Daniel; Schwarzer, Guido; Becker, Gerhild (2023-04-14)."Pharmacological interventions for pruritus in adult palliative care patients".The Cochrane Database of Systematic Reviews.4(2023): CD008320.doi:10.1002/14651858.CD008320.pub4.ISSN1469-493X.PMC11339634.PMID37314034.Archivedfrom the original on 2023-07-27.Retrieved2023-07-27.
- ^Yosipovitch G, Greaves MW, Schmelz M (February 2003). "Itch".Lancet.361(9358): 690–694.doi:10.1016/S0140-6736(03)12570-6.PMID12606187.S2CID208793207.
- ^abcdTwycross R, Greaves MW, Handwerker H, et al. (January 2003)."Itch: scratching more than the surface".QJM.96(1): 7–26.doi:10.1093/qjmed/hcg002.PMID12509645.
- ^"Essential pruritus".Archivedfrom the original on 6 August 2020.Retrieved25 July2019.
- ^Schmelz M, Schmidt R, Bickel A, et al. (October 1997)."Specific C-receptors for itch in human skin".The Journal of Neuroscience.17(20): 8003–8008.doi:10.1523/JNEUROSCI.17-20-08003.1997.PMC6793906.PMID9315918.
- ^Usoskin D, Furlan A, Islam S, et al. (January 2015). "Unbiased classification of sensory neuron types by large-scale single-cell RNA sequencing".Nature Neuroscience.18(1): 145–153.doi:10.1038/nn.3881.PMID25420068.S2CID205437148.
- ^Deng, Liwen; Costa, Flavia; Blake, Kimbria J.; Choi, Samantha; Chandrabalan, Arundhasa; Yousuf, Muhammad Saad; Shiers, Stephanie; Dubreuil, Daniel; Vega-Mendoza, Daniela; Rolland, Corinne; Deraison, Celine; Voisin, Tiphaine; Bagood, Michelle D.; Wesemann, Lucia; Frey, Abigail M.; Palumbo, Joseph S.; Wainger, Brian J.; Gallo, Richard L.; Leyva-Castillo, Juan-Manuel; Vergnolle, Nathalie; Price, Theodore J.; Ramachandran, Rithwik; Horswill, Alexander R.; Chiu, Isaac M. (2023)."S. aureus drives itch and scratch-induced skin damage through a V8 protease-PAR1 axis".Cell.186(24): 5375–5393.e25.doi:10.1016/j.cell.2023.10.019.PMC10669764.PMID37995657.
{{cite journal}}:CS1 maint: PMC embargo expired (link) - ^Han L, Ma C, Liu Q, et al. (February 2013)."A subpopulation of nociceptors specifically linked to itch".Nature Neuroscience.16(2): 174–182.doi:10.1038/nn.3289.PMC3557753.PMID23263443.
- ^Sun YG, Chen ZF (August 2007). "A gastrin-releasing peptide receptor mediates the itch sensation in the spinal cord".Nature.448(7154): 700–703.Bibcode:2007Natur.448..700S.doi:10.1038/nature06029.PMID17653196.S2CID4407979.
- ^Bernhard JD (2005)."Itch and pruritus: what are they, and how should itches be classified?".Dermatologic Therapy.18(4): 288–291.doi:10.1111/j.1529-8019.2005.00040.x.PMID16296999.S2CID7107271.
- ^Rukwied R, Lischetzki G, McGlone F, et al. (June 2000). "Mast cell mediators other than histamine induce pruritus in atopic dermatitis patients: a dermal microdialysis study".The British Journal of Dermatology.142(6): 1114–1120.doi:10.1046/j.1365-2133.2000.03535.x.PMID10848733.S2CID23996950.
- ^abAndrade A, Kuah CY, Martin-Lopez JE, et al. (Cochrane Skin Group) (January 2020)."Interventions for chronic pruritus of unknown origin".The Cochrane Database of Systematic Reviews.1(1): CD013128.doi:10.1002/14651858.CD013128.pub2.PMC6984650.PMID31981369.
- ^Hercogová J (2005)."Topical anti-itch therapy".Dermatologic Therapy.18(4): 341–343.doi:10.1111/j.1529-8019.2005.00033.x.PMID16297007.S2CID31573591.
- ^El Mulla KF, Khalifa DE, Gawish RI, Eldeeb ME (2023)."Phototherapy versus pregabalin in treatment of chronic kidney disease associated pruritus: randomized controlled study".Journal of the Egyptian Women's Dermatologic Society.20(2): 81.doi:10.4103/jewd.jewd_50_22.ISSN1687-1537.
- ^Rinaldi G (April 2019)."The Itch-Scratch Cycle: A Review of the Mechanisms".Dermatology Practical & Conceptual.9(2): 90–97.doi:10.5826/dpc.0902a03.PMC6502296.PMID31106010.
- ^Oetjen LK, Mack MR, Feng J, et al. (2017)."Sensory Neurons Co-opt Classical Immune Signaling Pathways to Mediate Chronic Itch".Cell.171(1): 217–228.e13.doi:10.1016/j.cell.2017.08.006.PMC5658016.PMID28890086.
- ^"Efficacy and Safety of Subcutaneous Dupilumab for the Treatment of Adult Participants With Chronic Pruritus of Unknown Origin (CPUO) (LIBERTY-CPUO-CHIC)".ClinicalTrials.gov.NCT05263206.Archivedfrom the original on 2023-01-14.Retrieved2023-01-14.
- ^Vos T, Flaxman AD, Naghavi M, et al. (Global Burden of Disease Study Collaborators) (December 2012)."Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010".Lancet.380(9859): 2163–2196.doi:10.1016/S0140-6736(12)61729-2.PMC6350784.PMID23245607.
- ^Jean Bolognia; Joseph L. Jorizzo; Ronald P. Rapini (2008).Dermatology(2nd ed.). St. Louis, Mo.: Mosby/Elsevier.ISBN978-1-4160-2999-1.OCLC212399895.
Further reading
edit- Han L, Dong X (6 May 2014)."Itch mechanisms and circuits".Annual Review of Biophysics.43(1): 331–355.doi:10.1146/annurev-biophys-051013-022826.PMC4081479.PMID24819620.
- Andrew D, Craig AD (January 2001). "Spinothalamic lamina I neurons selectively sensitive to histamine: a central neural pathway for itch".Nature Neuroscience.4(1): 72–77.doi:10.1038/82924.PMID11135647.S2CID28727869.
- "Pruritus".National Cancer Institute. 2003. Archived fromthe originalon 25 December 2005.Retrieved22 August2005.