Painis a distressing feeling often caused by intense or damagingstimuli.TheInternational Association for the Study of Paindefines pain as "an unpleasantsensoryandemotionalexperience associated with, or resembling that associated with, actual or potential tissue damage. "[1]
| Pain | |
|---|---|
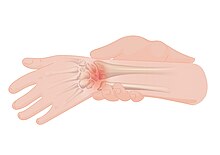 | |
| An illustration ofwrist pain | |
| Specialty | Neurology Pain medicine |
| Symptoms | Unpleasant sensory and emotional sensations[1] |
| Duration | Typically depends on the cause |
| Types | Physical,psychological,psychogenic |
| Medication | Analgesic |
Pain motivatesorganismsto withdraw from damaging situations, to protect a damaged body part while it heals, and to avoid similar experiences in the future.[2]Congenital insensitivity to painmay result in reducedlife expectancy.[3]Most pain resolves once thenoxious stimulusis removed and the body has healed, but it may persist despite removal of the stimulus and apparent healing of the body. Sometimes pain arises in the absence of any detectable stimulus, damage or disease.[4]
Pain is the most common reason for physician consultation in most developed countries.[5][6]It is a major symptom in many medical conditions, and can interfere with a person'squality of lifeand general functioning.[7]People in pain experience impaired concentration,working memory,mental flexibility,problem solving and information processing speed, and are more likely to experience irritability, depression, and anxiety.
Simple pain medications are useful in 20% to 70% of cases.[8]Psychological factors such associal support,cognitive behavioral therapy,excitement, or distraction can affect pain's intensity or unpleasantness.[9][10]
Etymology
editFirst attested in English in 1297, the wordpeyncomes from theOld Frenchpeine,in turn fromLatinpoenameaning "punishment, penalty"[11][12](also meaning "torment, hardship, suffering" in Late Latin) and that fromGreekποινή (poine), generally meaning "price paid, penalty, punishment".[13][14]
Classification
editTheInternational Association for the Study of Painrecommends using specific features to describe a patient's pain:
- Region of the body involved (e.g. abdomen, lower limbs)
- System whose dysfunction may be causing the pain (e.g., nervous, gastrointestinal)
- Duration and pattern of occurrence
- Intensity
- Cause[15]
Chronic versus acute
editPain is usually transitory, lasting only until the noxious stimulus is removed or the underlying damage or pathology has healed. But some painful conditions, such asrheumatoid arthritis,peripheral neuropathy,cancer,andidiopathicpain, may persist for years. Pain that lasts a long time is called "chronic"or" persistent ", and pain that resolves quickly is called"acute".Traditionally, the distinction between acute and chronic pain has relied upon an arbitrary interval of time between onset and resolution; the two most commonly used markers being 3 months and 6 months since the onset of pain,[16]though some theorists and researchers have placed the transition from acute to chronic pain at 12 months.[17]: 93 Others apply "acute" to pain that lasts less than 30 days, "chronic" to pain of more than six months' duration, and "subacute" to pain that lasts from one to six months.[18]A popular alternative definition of "chronic pain", involving no arbitrarily fixed duration, is "pain that extends beyond the expected period of healing".[16]Chronic pain may be classified as "cancer-related"or" benign. "[18]
Allodynia
editAllodyniais pain experienced in response to a normally painless stimulus.[19]It has no biological function and is classified by characteristics of the stimuli as cold, heat, touch, pressure or a pinprick.[19][20]
Phantom
editPhantom painis pain felt in a part of the body that has beenamputated,or from which the brain no longer receives signals. It is a type of neuropathic pain.[21]
Theprevalenceof phantom pain in upper limb amputees is nearly 82%, and in lower limb amputees is 54%.[21]One study found that eight days after amputation, 72% of patients had phantom limb pain, and six months later, 67% reported it.[22][23]Some amputees experience continuous pain that varies in intensity or quality; others experience several bouts of pain per day, or it may reoccur less often. It is often described as shooting, crushing, burning or cramping. If the pain is continuous for a long period, parts of the intact body may become sensitized, so that touching them evokes pain in the phantom limb. Phantom limb pain may accompanyurinationordefecation.[24]: 61–69
Local anestheticinjections into the nerves or sensitive areas of the stump may relieve pain for days, weeks, or sometimes permanently, despite the drug wearing off in a matter of hours; and small injections ofhypertonicsaline into the soft tissue between vertebrae produces local pain that radiates into the phantom limb for ten minutes or so and may be followed by hours, weeks, or even longer of partial or total relief from phantom pain. Vigorous vibration or electrical stimulation of the stump, or current from electrodes surgically implanted onto the spinal cord, all produce relief in some patients.[24]: 61–69
Mirror boxtherapy produces the illusion of movement and touch in a phantom limb which in turn may cause a reduction in pain.[25]
Paraplegia,the loss of sensation and voluntary motor control after serious spinal cord damage, may be accompanied bygirdle painat the level of the spinal cord damage,visceral painevoked by a filling bladder or bowel, or, in five to ten percent of paraplegics, phantom body pain in areas of complete sensory loss. This phantom body pain is initially described as burning or tingling but may evolve into severe crushing or pinching pain, or the sensation of fire running down the legs or of a knife twisting in the flesh. Onset may be immediate or may not occur until years after the disabling injury. Surgical treatment rarely provides lasting relief.[24]: 61–69
Breakthrough
editBreakthrough pain is transitory pain that comes on suddenly and is not alleviated by the patient's regularpain management.It is common in cancer patients who often have background pain that is generally well-controlled by medications, but who also sometimes experience bouts of severe pain that from time to time "breaks through" the medication. The characteristics of breakthroughcancer painvary from person to person and according to the cause. Management of breakthrough pain can entail intensive use ofopioids,includingfentanyl.[26][27]
Asymbolia and insensitivity
editThe ability to experience pain is essential for protection from injury, and recognition of the presence of injury. Episodicanalgesiamay occur under special circumstances, such as in the excitement of sport or war: a soldier on the battlefield may feel no pain for many hours from a traumatic amputation or other severe injury.[28]
Although unpleasantness is an essential part of theIASPdefinition of pain,[29]it is possible in some patients to induce a state known as pain asymbolia, described as intense pain devoid of unpleasantness, withmorphineinjection orpsychosurgery.[30]Such patients report that they have pain but are not bothered by it; they recognize the sensation of pain but suffer little, or not at all.[31]Indifference to pain can also rarely be present from birth; these people have normal nerves on medical investigations, and find pain unpleasant, but do not avoid repetition of the pain stimulus.[3]
Insensitivity to pain may also result from abnormalities in thenervous system.This is usually the result ofacquireddamage to the nerves, such asspinal cord injury,diabetes mellitus(diabetic neuropathy), orleprosyin countries where that disease is prevalent.[32]These individuals are at risk of tissue damage and infection due to undiscovered injuries. People with diabetes-related nerve damage, for instance, sustain poorly-healing foot ulcers as a result of decreased sensation.[33]
A much smaller number of people are insensitive to pain due to an inborn abnormality of the nervous system, known as "congenital insensitivity to pain".[3]Children with this condition incur carelessly-repeated damage to their tongues, eyes, joints, skin, and muscles. Some die before adulthood, and others have a reduced life expectancy.[34]Most people with congenital insensitivity to pain have one of fivehereditary sensory and autonomic neuropathies(which includesfamilial dysautonomiaandcongenital insensitivity to pain with anhidrosis).[35]These conditions feature decreased sensitivity to pain together with other neurological abnormalities, particularly of theautonomic nervous system.[3][35]A very rare syndrome with isolated congenital insensitivity to pain has been linked with mutations in theSCN9Agene, which codes for a sodium channel (Nav1.7) necessary in conducting pain nerve stimuli.[36]
Functional effects
editExperimental subjects challenged by acute pain and patients in chronic pain experience impairments in attention control,working memory capacity,mental flexibility,problem solving, and information processing speed.[37]Pain is also associated with increased depression, anxiety, fear, and anger.[38]
If I have matters right, the consequences of pain will include direct physical distress, unemployment, financial difficulties, marital disharmony, and difficulties in concentration and attention…
— Harold Merskey2000[39]
On subsequent negative emotion
editAlthough pain is considered to be aversive and unpleasant and is therefore usually avoided, ameta-analysiswhich summarized and evaluated numerous studies from various psychological disciplines, found a reduction innegative affect.Across studies, participants that were subjected to acute physical pain in the laboratory subsequently reported feeling better than those in non-painful control conditions, a finding which was also reflected in physiological parameters.[40]A potential mechanism to explain this effect is provided by theopponent-process theory.
Theory
editHistorical
editBefore the relatively recent discovery ofneuronsand their role in pain, various body functions were proposed to account for pain. There were several competing early theories of pain among the ancient Greeks:Hippocratesbelieved that it was due to an imbalance invital fluids.[41]In the 11th century,Avicennatheorized that there were a number of feeling senses, including touch, pain, and titillation.[42]
In 1644,René Descartestheorized that pain was a disturbance that passed along nerve fibers until the disturbance reached the brain.[41][43]The work of Descartes and Avicenna prefigured the 19th-century development ofspecificity theory.Specificity theory saw pain as "a specific sensation, with its own sensory apparatus independent of touch and other senses".[44]Another theory that came to prominence in the 18th and 19th centuries wasintensive theory,which conceived of pain not as a unique sensory modality, but an emotional state produced by stronger than normal stimuli such as intense light, pressure or temperature.[45]By the mid-1890s,specificitywas backed primarily by physiologists and physicians, and psychologists mostly backed theintensive theory.However, after a series of clinical observations byHenry Headand experiments byMax von Frey,the psychologists migrated tospecificityalmost en masse. By the century's end, most physiology and psychology textbooks presented painspecificityas fact.[42][44]
Modern
editSome sensory fibers do not differentiate betweennoxiousand non-noxious stimuli, while others (i.e.,nociceptors) respond only to noxious, high-intensity stimuli. At the peripheral end of the nociceptor, noxious stimuli generate currents that, above a given threshold, sendsignalsalong the nerve fiber to the spinal cord. The "specificity" (whether it responds to thermal, chemical, or mechanical features of its environment) of a nociceptor is determined by whichion channelsit expresses at its peripheral end. So far, dozens of types of nociceptor ion channels have been identified, and their exact functions are still being determined.[46]
The pain signal travels from the periphery to the spinal cord alongA-deltaandCfibers. Because the A-delta fiber is thicker than the C fiber, and is thinly sheathed in an electrically insulating material (myelin), it carries its signal faster (5–30m/s) than the unmyelinated C fiber (0.5–2 m/s).[47]Pain evoked by the A-delta fibers is described as sharp and is felt first. This is followed by a duller pain—often described as burning—carried by the C fibers.[48]These A-delta and C fibers enter the spinal cord viaLissauer's tractand connect with spinal cord nerve fibers in thecentral gelatinous substance of the spinal cord.These spinal cord fibers then cross the cord via theanterior white commissureand ascend in thespinothalamic tract.Before reaching the brain, the spinothalamic tract splits into thelateral,neospinothalamic tractand themedial,paleospinothalamic tract.The neospinothalamic tract carries the fast, sharp A-delta signal to the ventral posterolateral nucleus of thethalamus.The paleospinothalamic tract carries the slow, dull C fiber pain signal. Some of the paleospinothalamic fibers peel off in the brain stem—connecting with the reticular formation or midbrain periaqueductal gray—and the remainder terminate in the intralaminar nuclei of the thalamus.[49]
Pain-related activity in the thalamus spreads to theinsular cortex(thought to embody, among other things, the feeling that distinguishes pain from otherhomeostatic emotionssuch as itch and nausea) andanterior cingulate cortex(thought to embody, among other things, the affective/motivational element, the unpleasantness of pain),[50]and pain that is distinctly located also activates theprimaryandsecondary somatosensory cortex.[51]
Spinal cord fibers dedicated to carrying A-delta fiber pain signals and others that carry both A-delta and C fiber pain signals to thethalamushave been identified. Other spinal cord fibers, known aswide dynamic range neurons,respond to A-delta and C fibers and the much larger, more heavily myelinated A-beta fibers that carry touch, pressure, and vibration signals.[47]
Ronald MelzackandPatrick Wallintroduced theirgate control theoryin the 1965Sciencearticle "Pain Mechanisms: A New Theory".[52]The authors proposed that the thin C and A-delta (pain) and large diameter A-beta (touch, pressure, vibration) nerve fibers carry information from the site of injury to two destinations in thedorsal hornof the spinal cord, and that A-beta fiber signals acting on inhibitory cells in the dorsal horn can reduce the intensity of pain signals sent to the brain.[43]
Three dimensions of pain
editIn 1968,Ronald MelzackandKenneth Caseydescribed chronic pain in terms of its three dimensions:
- "sensory-discriminative" (sense of the intensity, location, quality, and duration of the pain),
- "affective-motivational" (unpleasantness and urge to escape the unpleasantness) and
- "cognitive-evaluative" (cognitions such as appraisal, cultural values, distraction, and hypnotic suggestion).
They theorized that pain intensity (the sensory discriminative dimension) and unpleasantness (the affective-motivational dimension) are not simply determined by the magnitude of the painful stimulus, but "higher" cognitive activities can influence perceived intensity and unpleasantness. Cognitive activities may affect both sensory and affective experience, or they may modify primarily the affective-motivational dimension. Thus, excitement in games or war appears to block both the sensory-discriminative and affective-motivational dimensions of pain, while suggestion and placebos may modulate only the affective-motivational dimension and leave the sensory-discriminative dimension relatively undisturbed.[53](p. 432)
The paper ends with a call to action: "Pain can be treated not only by trying to cut down the sensory input by anesthetic block, surgical intervention and the like, but also by influencing the motivational-affective and cognitive factors as well."[53](p. 435)
Evolutionary and behavioral role
editPain is part of the body's defense system, producing areflexiveretraction from the painful stimulus, and tendencies to protect the affected body part while it heals, and avoid that harmful situation in the future.[54][55]It is an important part of animal life, vital to healthy survival. People withcongenital insensitivity to painhave reducedlife expectancy.[3]
InThe Greatest Show on Earth: The Evidence for Evolution,biologistRichard Dawkinsaddresses the question of why pain should have the quality of being painful. He describes the alternative as a mental raising of a "red flag". To argue why that red flag might be insufficient, Dawkins argues that drives must compete with one another within living beings. The most "fit" creature would be the one whose pains are well balanced. Those pains which mean certain death when ignored will become the most powerfully felt. The relative intensities of pain, then, may resemble the relative importance of that risk to our ancestors.[a]This resemblance will not be perfect, however, because natural selection can be apoor designer.This may have maladaptive results such assupernormal stimuli.[56]
Pain, however, does not only wave a "red flag" within living beings but may also act as a warning sign and a call for help to other living beings. Especially in humans who readily helped each other in case of sickness or injury throughout their evolutionary history, pain might be shaped by natural selection to be a credible and convincing signal of the need for relief, help, and care.[57]
Idiopathic pain (pain that persists after the trauma or pathology has healed, or that arises without any apparent cause) may be an exception to the idea that pain is helpful to survival, although somepsychodynamicpsychologists argue that such pain is psychogenic, enlisted as a protective distraction to keep dangerous emotions unconscious.[58]
Thresholds
editIn pain science, thresholds are measured by gradually increasing the intensity of a stimulus in a procedure calledquantitative sensory testingwhich involves such stimuli aselectric current,thermal (heat or cold), mechanical (pressure, touch, vibration),ischemic,or chemical stimuli applied to the subject to evoke a response.[59]The "pain perception threshold"is the point at which the subject begins to feel pain, and the" pain threshold intensity "is the stimulus intensity at which the stimulus begins to hurt. The"pain tolerancethreshold "is reached when the subject acts to stop the pain.[59]
Assessment
editA person's self-report is the most reliable measure of pain.[60][61][62]Some health care professionals may underestimate pain severity.[63]A definition of pain widely employed in nursing, emphasizing its subjective nature and the importance of believing patient reports, was introduced byMargo McCafferyin 1968: "Pain is whatever the experiencing person says it is, existing whenever he says it does".[64]To assess intensity, the patient may be asked to locate their pain on a scale of 0 to 10, with 0 being no pain at all, and 10 the worst pain they have ever felt. Quality can be established by having the patient complete theMcGill Pain Questionnaireindicating which words best describe their pain.[7]
Visual analogue scale
editThe visual analogue scale is a common, reproducible tool in the assessment of pain and pain relief.[65]The scale is a continuous line anchored by verbal descriptors, one for each extreme of pain where a higher score indicates greater pain intensity. It is usually 10 cm in length with no intermediate descriptors as to avoid marking of scores around a preferred numeric value. When applied as a pain descriptor, these anchors are often 'no pain' and 'worst imaginable pain ". Cut-offs for pain classification have been recommended as no pain (0–4mm), mild pain (5–44mm), moderate pain (45–74mm) and severe pain (75–100mm).[66][check quotation syntax]
Multidimensional pain inventory
editThe Multidimensional Pain Inventory (MPI) is a questionnaire designed to assess thepsychosocialstate of a person with chronic pain. Combining the MPI characterization of the person with theirIASP five-category pain profileis recommended for deriving the most useful case description.[16]
Assessment in non-verbal people
editNon-verbalpeople cannot use words to tell others that they are experiencing pain. However, they may be able to communicate through other means, such as blinking, pointing, or nodding.[67]
With a non-communicative person, observation becomes critical, and specific behaviors can be monitored as pain indicators. Behaviors such as facial grimacing and guarding (trying to protect part of the body from being bumped or touched) indicate pain, as well as an increase or decrease in vocalizations, changes in routine behavior patterns and mental status changes. Patients experiencing pain may exhibit withdrawnsocial behaviorand possibly experience adecreased appetiteand decreased nutritional intake. A change in condition that deviates from baseline, such as moaning with movement or when manipulating a body part, and limitedrange of motionare also potential pain indicators. In patients who possess language but are incapable of expressing themselves effectively, such as those with dementia, an increase in confusion or display of aggressive behaviors or agitation may signal that discomfort exists, and further assessment is necessary. Changes in behavior may be noticed by caregivers who are familiar with the person's normal behavior.[67]
Infants do feel pain,but lack the language needed to report it, and so communicate distress by crying. A non-verbal pain assessment should be conducted involving the parents, who will notice changes in the infant which may not be obvious to the health care provider.Pre-term babiesare more sensitive to painful stimuli than those carried to full term.[68]
Another approach, when pain is suspected, is to give the person treatment for pain, and then watch to see whether the suspected indicators of pain subside.[67]
Other reporting barriers
editThe way in which one experiences and responds to pain is related to sociocultural characteristics, such as gender, ethnicity, and age.[69][70]An aging adult may not respond to pain in the same way that a younger person might. Their ability to recognize pain may be blunted by illness or the use ofmedication.Depression may also keep older adult from reporting they are in pain. Decline inself-caremay also indicate the older adult is experiencing pain. They may be reluctant to report pain because they do not want to be perceived as weak, or may feel it is impolite or shameful to complain, or they may feel the pain is a form of deserved punishment.[71][72]
Cultural barriers may also affect the likelihood of reporting pain. Patients may feel that certain treatments go against their religious beliefs. They may not report pain because they feel it is a sign that death is near. Many people fear the stigma of addiction, and avoid pain treatment so as not to be prescribed potentially addicting drugs. Many Asians do not want to lose respect in society by admitting they are in pain and need help, believing the pain should be borne in silence, while other cultures feel they should report pain immediately to receive immediate relief.[68]
Gender can also be a perceived factor in reporting pain.Gender differencescan be the result of social and cultural expectations, with, in some cultures, women expected to be more emotional and show pain, and men to be more stoic.[68]As a result, female pain may be at a higher risk of being stigmatized, leading to less urgent treatment of women based on social expectations of their ability to accurately report it.[73]This has been postulated to lead to extended emergency room wait times for women and frequent dismissal of their ability to accurately report pain.[74][75]
Diagnostic aid
editPain is a symptom of many medical conditions. Knowing the time of onset, location, intensity, pattern of occurrence (continuous, intermittent, etc.), exacerbating and relieving factors, and quality (burning, sharp, etc.) of the pain will help the examining physician to accurately diagnose the problem. For example, chest pain described as extreme heaviness may indicatemyocardial infarction,while chest pain described as tearing may indicateaortic dissection.[76][77]
Physiological measurement
editFunctional magnetic resonance imagingbrain scanning has been used to measure pain, and correlates well with self-reported pain.[78][79][80]
Mechanisms
editNociceptive
editNociceptive pain is caused by stimulation ofsensory nerve fibersthat respond to stimuli approaching or exceeding harmful intensity (nociceptors), and may be classified according to the mode of noxious stimulation. The most common categories are "thermal" (e.g. heat or cold), "mechanical" (e.g. crushing, tearing, shearing, etc.) and "chemical" (e.g.iodinein a cut or chemicals released duringinflammation). Some nociceptors respond to more than one of these modalities and are consequently designated polymodal.
Nociceptive pain may also be classed according to the site of origin and divided into "visceral", "deep somatic" and "superficial somatic" pain.Visceral structures(e.g., the heart, liver and intestines) are highly sensitive to stretch,ischemiaandinflammation,but relatively insensitive to other stimuli that normally evoke pain in other structures, such as burning and cutting.Visceral painis diffuse, difficult to locate and oftenreferredto a distant, usually superficial, structure. It may be accompanied by nausea and vomiting and may be described as sickening, deep, squeezing, and dull.[81]Deep somaticpain is initiated by stimulation of nociceptors in ligaments, tendons, bones, blood vessels,fasciaeand muscles, and is dull, aching, poorly-localized pain. Examples includesprainsand broken bones.Superficial somaticpain is initiated by activation of nociceptors in the skin or other superficial tissue, and is sharp, well-defined and clearly located. Examples of injuries that produce superficial somatic pain include minor wounds and minor (first degree) burns.[17]
Neuropathic
editNeuropathic pain is caused by damage or disease affecting any part of thenervous systeminvolved in bodily feelings (thesomatosensory system).[82]Neuropathic pain may be divided into peripheral,central,or mixed (peripheral and central) neuropathic pain.Peripheralneuropathic pain is often described as "burning", "tingling", "electrical", "stabbing", or "pins and needles".[83]Bumping the "funny bone"elicits acute peripheral neuropathic pain.
Some manifestations of neuropathic pain include: traumatic neuropathy,tic douloureux,painfuldiabetic neuropathy,andpostherpetic neuralgia.[84]
Nociplastic
editNociplastic pain is pain characterized by a changednociception(but without evidence of real or threatened tissue damage, or without disease or damage in thesomatosensory system).[10]
Psychogenic
editPsychogenic pain, also calledpsychalgiaorsomatoform pain,is pain caused, increased or prolonged by mental, emotional or behavioral factors.[85]Headaches, back pain and stomach pain are sometimes diagnosed as psychogenic.[85]Those affected are often stigmatized, because both medical professionals and the general public tend to think that pain from a psychological source is not "real". However, specialists consider that it is no less actual or hurtful than pain from any other source.[30]
People withlong-term painfrequently display psychological disturbance, with elevated scores on theMinnesota Multiphasic Personality Inventoryscales ofhysteria,depression andhypochondriasis(the "neurotic triad"). Some investigators have argued that it is this neuroticism that causes acute pain to turn chronic, but clinical evidence points in the other direction, to chronic pain causingneuroticism.When long-term pain is relieved by therapeutic intervention, scores on the neurotic triad andanxietyfall, often to normal levels.Self-esteem,often low in chronic pain patients, also shows improvement once pain has resolved.[24]: 31–32
Management
editPain can be treated through a variety of methods. The most appropriate method depends upon the situation. Management ofchronic paincan be difficult and may require the coordinated efforts of apain managementteam, which typically includesmedical practitioners,clinical pharmacists,clinical psychologists,physiotherapists,occupational therapists,physician assistants,andnurse practitioners.[86]
Inadequate treatment of pain is widespread throughout surgical wards,intensive care units,and accident andemergency departments,ingeneral practice,in the management of all forms of chronic pain including cancer pain, and inend of life care.[87][88][89][90][91][92][93]This neglect extends to all ages, from newborns tomedically frailelderly.[94][95]In the US,AfricanandHispanic Americansare more likely than others to suffer unnecessarily while in the care of a physician;[96][97]and women's pain is more likely to be undertreated than men's.[98]
TheInternational Association for the Study of Painadvocates that the relief of pain should be recognized as ahuman right,that chronic pain should be considered a disease in its own right, and thatpain medicineshould have the full status of amedical specialty.[99]It is a specialty only in China and Australia at this time.[100]Elsewhere, pain medicine is a subspecialty under disciplines such asanesthesiology,physiatry,neurology,palliative medicineandpsychiatry.[101]In 2011,Human Rights Watchalerted that tens of millions of people worldwide are still denied access to inexpensive medications for severe pain.[102]
Medication
editAcute pain is usually managed with medications such asanalgesicsandanesthetics.[103]Caffeinewhen added to pain medications such asibuprofen,may provide some additional benefit.[104][105]Ketaminecan be used instead of opioids for short-term pain.[106]Pain medications can cause paradoxical side effects, such asopioid-induced hyperalgesia(severe generalized pain caused by long-term opioid use).[107][108]
Sugar (sucrose) when taken by mouth reducespain in newborn babiesundergoing some medical procedures (alancingof the heel,venipuncture,andintramuscular injections). Sugar does not remove pain fromcircumcision,and it is unknown if sugar reduces pain for other procedures.[109]Sugar did not affect pain-relatedelectrical activityin the brains of newborns one second after the heel lance procedure.[110]Sweet liquid by mouth moderately reduces the rate and duration of crying caused by immunization injection in children between one and twelve months of age.[111]
Psychological
editIndividuals with moresocial supportexperience less cancer pain, take less pain medication, report less labor pain and are less likely to useepidural anesthesiaduring childbirth, or suffer from chest pain aftercoronary artery bypass surgery.[9]
Suggestioncan significantly affect pain intensity. About 35% of people report marked relief after receiving asalineinjection they believed to bemorphine.Thisplaceboeffect is more pronounced in people who are prone to anxiety, and so anxiety reduction may account for some of the effect, but it does not account for all of it. Placebos are more effective for intense pain than mild pain; and they produce progressively weaker effects with repeated administration.[24]: 26–28 It is possible for many with chronic pain to become so absorbed in an activity or entertainment that the pain is no longer felt, or is greatly diminished.[24]: 22–23
A number of meta-analyses have foundclinical hypnosisto be effective in controlling pain associated with diagnostic and surgical procedures in both adults and children, as well as pain associated with cancer and childbirth.[112]A 2007 review of 13 studies found evidence for the efficacy of hypnosis in the reduction of chronic pain under some conditions, though the number of patients enrolled in the studies was low, raising issues related to the statistical power to detect group differences, and most lacked credible controls for placebo or expectation. The authors concluded that "although the findings provide support for the general applicability of hypnosis in the treatment of chronic pain, considerably more research will be needed to fully determine the effects of hypnosis for different chronic-pain conditions."[113]
Alternative medicine
editAn analysis of the 13 highest quality studies of pain treatment withacupuncture,published in January 2009, concluded there was little difference in the effect of real, fake and no acupuncture.[114]However, more recent reviews have found some benefit.[115][116][117]
Additionally, there is tentative evidence for a few herbal medicines.[118]
For chronic (long-term)lower back pain,spinal manipulationproduces tiny,clinically insignificant,short-term improvements in pain and function, compared withsham therapyand other interventions.[119]Spinal manipulation produces the same outcome as other treatments, such as general practitioner care, pain-relief drugs, physical therapy, and exercise, for acute (short-term) lower back pain.[119]
There has been some interest in the relationship betweenvitamin Dand pain, but the evidence so far fromcontrolled trialsfor such a relationship, other than inosteomalacia,is inconclusive.[120]
The International Association for the Study of Pain (IASP) says that due to a lack of evidence from high quality research, it does not endorse the general use of cannabinoids to treat pain.[121]
Epidemiology
editPain is the main reason for visiting anemergency departmentin more than 50% of cases,[122]and is present in 30% of family practice visits.[123]Severalepidemiologicalstudies have reported widely varying prevalence rates for chronic pain, ranging from 12 to 80% of the population.[124]It becomes more common as people approach death. A study of 4,703 patients found that 26% had pain in the last two years of life, increasing to 46% in the last month.[125]
A survey of 6,636 children (0–18 years of age) found that, of the 5,424 respondents, 54% had experienced pain in the preceding three months. A quarter reported having experienced recurrent or continuous pain for three months or more, and a third of these reported frequent and intense pain. The intensity of chronic pain was higher for girls, and girls' reports of chronic pain increased markedly between ages 12 and 14.[126]
Society and culture
editPhysical pain is a universal experience, and a strong motivator of human and animal behavior. As such, physical pain is used politically in relation to various issues such aspain managementpolicy,drug control, animal rightsor animal welfare, torture,andpain compliance.The deliberate infliction of pain and the medical management of pain are both important aspects ofbiopower,a concept that encompasses the "set of mechanisms through which the basic biological features of the human species became the object of a political strategy".[127]
In various contexts, the deliberate infliction of pain in the form ofcorporal punishmentis used as retribution for an offence, for the purpose of disciplining or reforming a wrongdoer, or to deter attitudes or behaviour deemed unacceptable. In Western societies, the intentional infliction of severe pain (torture) was principally used to extract confession prior to its abolition in the latter part of the 19th century. Torture as a means to punish thecitizenhas been reserved for offences posing a severe threat to the social fabric (for example,treason).[128]
The administration of torture on bodies othered by the cultural narrative, those observed as not 'full members of society'[128]: 101–121[AD1] met a resurgence in the 20th century, possibly due to the heightened warfare.[128]: 101–121 [AD2]
Many cultures use painful ritual practices as a catalyst for psychological transformation.[129]The use of pain to transition to a 'cleansed and purified' state is seen in religiousself-flagellationpractices (particularly those ofChristianityandIslam), or personalcatharsisinneo-primitive body suspensionexperiences.[130]
Beliefs about pain play an important role in sporting cultures. Pain may be viewed positively, exemplified by the 'no pain, no gain' attitude, with pain seen as an essential part of training. Sporting culture tends to normalise experiences of pain and injury and celebrate athletes who 'play hurt'.[131]
Pain has psychological, social, and physical dimensions, and is greatly influenced by cultural factors.[132]
Non-humans
editRené Descartesargued that animals lack consciousness and therefore do not experience pain and suffering in the way that humans do.[133]Bernard RollinofColorado State University,the principal author of two U.S. federal laws regulating pain relief for animals,[b]wrote that researchers remained unsure into the 1980s as to whether animals experience pain, and that veterinarians trained in the U.S. before 1989 were simply taught to ignore animal pain.[135][136]The ability of invertebrate species of animals, such as insects, to feel pain and suffering is unclear.[137][138][139]
Specialists believe that all vertebrates can feel pain, and that certain invertebrates, like the octopus, may also.[137][140][141]The presence of pain in animals is unknown, but can be inferred through physical and behavioral reactions,[142]such as paw withdrawal from various noxious mechanical stimuli in rodents.[143]
Whileplants,as living beings, can perceive and communicate physical stimuli and damage, they do not feel pain simply because of the lack of any pain receptors, nerves, or a brain,[144]and, by extension, a lack of consciousness.[145]Many plants are known to perceive and respond to mechanical stimuli at a cellular level, and some plants such as thevenus flytraportouch-me-not,are known for their "obvious sensory abilities".[144]Nevertheless, no member of the plant kingdom does feel pain notwithstanding their abilities to respond to sunlight, gravity, wind, and any external stimuli such as insect bites since they lack any nervous system. The primary reason for this is that, unlike the members of theanimal kingdomwhose evolutionary successes and failures are shaped by suffering, the evolution of plants are simply shaped by life and death.[144]
See also
edit- Feeling,a perceptual state of conscious experience.
- Hedonic adaptation,the tendency to quickly return to a relatively stable level of happiness despite major positive or negative events
- Pain (philosophy),the branch of philosophy concerned with suffering and physical pain
- Pain and suffering,the legal term for the physical and emotional stress caused from an injury
Explanatory notes
edit- ^For example, lack of food, extreme cold, or serious injuries are felt as exceptionally painful, whereas minor damage is felt as mere discomfort.
- ^Rollin drafted the 1985 Health Research Extension Act and ananimal welfareamendment to the 1985 Food Security Act.[134]
References
edit- ^abRaja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. (September 2020)."The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises".Pain.161(9):1976–1982.doi:10.1097/j.pain.0000000000001939.PMC7680716.PMID32694387.
- ^Cervero F (2012).Understanding Pain: Exploring the Perception of Pain.Cambridge, Mass.: MIT Press. pp. Chapter 1.ISBN9780262305433.OCLC809043366.
- ^abcdeNagasako EM, Oaklander AL, Dworkin RH (February 2003). "Congenital insensitivity to pain: an update".Pain.101(3):213–219.doi:10.1016/S0304-3959(02)00482-7.PMID12583863.S2CID206055264.
- ^Raj PP (2007)."Taxonomy and classification of pain".In: The Handbook of Chronic Pain.Nova Biomedical Books.ISBN9781600210440.Archivedfrom the original on 30 March 2021.Retrieved3 February2016.
- ^Debono DJ, Hoeksema LJ, Hobbs RD (August 2013)."Caring for patients with chronic pain: pearls and pitfalls".The Journal of the American Osteopathic Association.113(8):620–7.doi:10.7556/jaoa.2013.023.PMID23918913.
- ^Turk DC, Dworkin RH (2004)."What should be the core outcomes in chronic pain clinical trials?".Arthritis Research & Therapy.6(4):151–4.doi:10.1186/ar1196.PMC464897.PMID15225358.
- ^abBreivik H, Borchgrevink PC, Allen SM, Rosseland LA, Romundstad L, Hals EK, Kvarstein G, Stubhaug A (July 2008)."Assessment of pain".British Journal of Anaesthesia.101(1):17–24.doi:10.1093/bja/aen103.PMID18487245.
- ^Moore RA, Wiffen PJ, Derry S, Maguire T, Roy YM, Tyrrell L (November 2015)."Non-prescription (OTC) oral analgesics for acute pain – an overview of Cochrane reviews".The Cochrane Database of Systematic Reviews.11(11): CD010794.doi:10.1002/14651858.CD010794.pub2.PMC6485506.PMID26544675.
- ^abEisenberger NI, Lieberman M (2005)."Why it hurts to be left out: The neurocognitive overlap between physical and social pain".In Williams KD (ed.).The Social Outcast: Ostracism, Social Exclusion, Rejection, & Bullying (Sydney Symposium of Social Psychology).East Sussex: Psychology Press. p. 210.ISBN9781841694245.
- ^abGarland EL, Brintz CE, Hanley AW, Roseen EJ, Atchley RM, Gaylord SA, et al. (January 2020)."Mind-Body Therapies for Opioid-Treated Pain: A Systematic Review and Meta-analysis".JAMA Internal Medicine.180(1):91–105.doi:10.1001/jamainternmed.2019.4917.PMC6830441.PMID31682676.
- ^Lewis CT, Short C."Poena".A Latin Dictionary.Archived fromthe originalon 13 May 2011 – via Perseus Digital Library.
- ^Lavoie, Anne; Toledo, Paloma (1 September 2013)."Multimodal Postcesarean Delivery Analgesia".Clinics in Perinatology.Pain Management in the Peripartum Period.40(3):443–455.doi:10.1016/j.clp.2013.05.008.ISSN0095-5108.PMID23972750.
- ^Liddell HG, Scott R."ποινή".A Greek-English Lexicon.Archived fromthe originalon 13 May 2011 – via Perseus Digital Library.
- ^"Pain".Archived fromthe originalon 28 July 2011 – via Online Etymology Dictionary.
- ^Merskey H, Bogduk N (1994).Classification of Chronic Pain(2 nd ed.). Seattle: International Association for the Study of Pain. pp.3 & 4.ISBN978-0931092053.
- ^abcTurk DC, Okifuji A (2001). "Pain terms and taxonomies of pain". In Bonica JJ, Loeser JD, Chapman CR, Turk DC (eds.).Bonica's management of pain.Hagerstwon, MD: Lippincott Williams & Wilkins.ISBN978-0781768276.
- ^abCoda BA, Bonica JJ (2000)."General considerations of acute pain".In Panswick CC, Main CJ (eds.).Pain management: an interdisciplinary approach.Edinburgh: Churchill Livingstone.ISBN978-0443056833.
- ^abThienhaus O, Cole BE (2002). "Classification of pain". In Weiner R (ed.).Pain management: a practical guide for clinicians.Boca Raton: CRC Press. pp.28.ISBN978-0849322624.
- ^abJensen TS, Finnerup NB (September 2014). "Allodynia and hyperalgesia in neuropathic pain: clinical manifestations and mechanisms".The Lancet. Neurology.13(9):924–935.doi:10.1016/s1474-4422(14)70102-4.PMID25142459.S2CID25011309.
- ^Lolignier S, Eijkelkamp N, Wood JN (January 2015)."Mechanical allodynia".Pflügers Archiv.467(1):133–139.doi:10.1007/s00424-014-1532-0.PMC4281368.PMID24846747.
- ^abKooijman CM, Dijkstra PU, Geertzen JH, Elzinga A, van der Schans CP (July 2000)."Phantom pain and phantom sensations in upper limb amputees: an epidemiological study".Pain.87(1):33–41.doi:10.1016/S0304-3959(00)00264-5.PMID10863043.S2CID7565030.[permanent dead link]
- ^Jensen TS, Krebs B, Nielsen J, Rasmussen P (November 1983). "Phantom limb, phantom pain and stump pain in amputees during the first 6 months following limb amputation".Pain.17(3):243–256.doi:10.1016/0304-3959(83)90097-0.PMID6657285.S2CID10304696.
- ^Jensen TS, Krebs B, Nielsen J, Rasmussen P (March 1985). "Immediate and long-term phantom limb pain in amputees: incidence, clinical characteristics and relationship to pre-amputation limb pain".Pain.21(3):267–278.doi:10.1016/0304-3959(85)90090-9.PMID3991231.S2CID24358789.
- ^abcdefWall PD, Melzack R (1996).The challenge of pain(2nd ed.). New York: Penguin Books.ISBN978-0140256703.
- ^Ramachandran VS, Rogers-Ramachandran D (April 1996). "Synaesthesia in phantom limbs induced with mirrors".Proceedings. Biological Sciences.263(1369):377–386.Bibcode:1996RSPSB.263..377R.doi:10.1098/rspb.1996.0058.PMID8637922.S2CID4819370.
- ^Mishra S, Bhatnagar S, Chaudhary P, Rana SP (January 2009)."Breakthrough cancer pain: review of prevalence, characteristics and management".Indian Journal of Palliative Care.15(1):14–18.doi:10.4103/0973-1075.53506.PMC2886208.PMID20606850.
- ^Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, Cherny N, Dale O, De Conno F, Fallon M, Hanna M, Haugen DF, Juhl G, King S, Klepstad P, Laugsand EA, Maltoni M, Mercadante S, Nabal M, Pigni A, Radbruch L, Reid C, Sjogren P, Stone PC, Tassinari D, Zeppetella G (February 2012)."Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC"(PDF).The Lancet. Oncology.13(2): e58–68.doi:10.1016/S1470-2045(12)70040-2.PMID22300860.Archived fromthe original(PDF)on 19 October 2014.Retrieved7 March2022.
- ^Beecher HK (1959).Measurement of subjective responses.New York: Oxford University Press.cited inMelzack R, Wall PD (1996).The challenge of pain(2nd ed.). London: Penguin. p. 7.ISBN978-0140256703.
- ^"International Association for the Study of Pain: Pain Definitions".Archived fromthe originalon 13 January 2015.Retrieved12 January2015.
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage
Alt URL[permanent dead link]Derived fromBonica JJ (June 1979). "The need of a taxonomy".Pain.6(3):247–248.doi:10.1016/0304-3959(79)90046-0.PMID460931.S2CID53161389. - ^ab"International Association for the Study of Pain | Pain Definitions"..Retrieved 12 October 2010.
- ^Grahek N (2007).Feeling pain and being in pain(2nd ed.). Cambridge, Mass.: MIT Press.ISBN978-0262517324.Archived fromthe originalon 27 September 2008.
- ^Brand PW, Yancey P (1997).The gift of pain: why we hurt & what we can do about it.Grand Rapids, Mich: Zondervan Publ.ISBN978-0310221449.
- ^Lipsky BA, Berendt AR, Deery HG, Embil JM, Joseph WS, Karchmer AW, LeFrock JL, Lew DP, Mader JT, Norden C, Tan JS (October 2004)."Diagnosis and treatment of diabetic foot infections".Clinical Infectious Diseases.39(7):885–910.doi:10.1086/424846.PMID15472838.
- ^Raina*, Triveni; Dash, Bhagya Ranjan."AN INTRODUCTORY APPROACH TO PAIN MANAGEMENT THROUGH AYURVEDA WITH BRIEF HOLISTIC REVIEW".
{{cite journal}}:Cite journal requires|journal=(help) - ^abAxelrod FB, Hilz MJ (December 2003). "Inherited autonomic neuropathies".Seminars in Neurology.23(4):381–390.doi:10.1055/s-2004-817722.PMID15088259.S2CID260317729.
- ^Raouf R, Quick K, Wood JN (November 2010)."Pain as a channelopathy".The Journal of Clinical Investigation.120(11):3745–3752.doi:10.1172/JCI43158.PMC2965577.PMID21041956.
- ^Hart RP, Wade JB, Martelli MF (April 2003). "Cognitive impairment in patients with chronic pain: the significance of stress".Current Pain and Headache Reports.7(2):116–126.doi:10.1007/s11916-003-0021-5.PMID12628053.S2CID14104974.
- ^Bruehl S, Burns JW, Chung OY, Chont M (March 2009)."Pain-related effects of trait anger expression: neural substrates and the role of endogenous opioid mechanisms".Neuroscience and Biobehavioral Reviews.33(3):475–491.doi:10.1016/j.neubiorev.2008.12.003.PMC2756489.PMID19146872.
- ^Merskey H (2000)."The History of Psychoanalytic Ideas Concerning Pain".In Weisberg JN, Gatchel RJ (eds.).Personality Characteristics of Patients With Pain.American Psychological Association (APA).ISBN978-1557986467.
- ^Bresin K, Kling L, Verona E (2018)."The effect of acute physical pain on subsequent negative emotional affect: A meta-analysis".Personality Disorders: Theory, Research, and Treatment.9(3):273–283.doi:10.1037/per0000248.PMC5624817.PMID28368146.
- ^abLinton. Models of Pain Perception. Elsevier Health, 2005. Print.
- ^abDallenbach KM (July 1939). "Pain: History and present status".American Journal of Psychology.52(3):331–347.doi:10.2307/1416740.JSTOR1416740.
- ^abMelzack R, Katz J (2004). "The Gate Control Theory: Reaching for the Brain". In Craig KD, Hadjistavropoulos T (eds.).Pain: psychological perspectives.Mahwah, N.J: Lawrence Erlbaum Associates, Publishers.ISBN978-0415650618.
- ^abBonica JJ (1990). "History of pain concepts and therapies".The management of pain.Vol. 1 (2 ed.). London: Lea & Febiger. p. 7.ISBN978-0812111224.
- ^Finger S (2001).Origins of neuroscience: a history of explorations into brain function.US: Oxford University Press. p. 149.ISBN978-0195146943.
- ^Woolf CJ, Ma Q (August 2007)."Nociceptors – noxious stimulus detectors".Neuron.55(3):353–364.doi:10.1016/j.neuron.2007.07.016.PMID17678850.S2CID13576368.
- ^abMarchand S (2010). "Applied pain neurophysiology". In Beaulieu P, Lussier D, Porreca F, Dickenson A (eds.).Pharmacology of pain.Seattle: International Association for the Study of Pain Press. pp.3–26.ISBN978-0931092787.
- ^Skevington S (1995).Psychology of pain.New York: Wiley. p.9.ISBN978-0471957737.
- ^Skevington SM (1995).Psychology of pain.Chichester, UK: Wiley. p.18.ISBN978-0471957737.
- ^Craig AD (2003). "Pain mechanisms: labeled lines versus convergence in central processing".Annual Review of Neuroscience.26:1–30.doi:10.1146/annurev.neuro.26.041002.131022.PMID12651967.S2CID12387848.
- ^Romanelli P, Esposito V (July 2004). "The functional anatomy of neuropathic pain".Neurosurgery Clinics of North America.15(3):257–268.doi:10.1016/j.nec.2004.02.010.PMID15246335.
- ^Melzack R,Wall PD(November 1965)."Pain mechanisms: a new theory"(PDF).Science.150(3699):971–979.Bibcode:1965Sci...150..971M.doi:10.1126/science.150.3699.971.PMID5320816.Archived fromthe original(PDF)on 14 January 2012.Retrieved7 March2022.
- ^abMelzack, Ronald;Casey, Kenneth(1968). "Sensory, Motivational, and Central Control Determinants of Pain". In Kenshalo, Dan (ed.).The Skin Senses.Springfield, Illinois: Charles C Thomas.
- ^Lynn B (1984)."Cutaneous nociceptors".In Winlow W, Holden AV (eds.).The neurobiology of pain: Symposium of the Northern Neurobiology Group, held at Leeds on 18 April 1983.Manchester: Manchester University Press. p. 106.ISBN978-0719009969.Archivedfrom the original on 30 March 2021.Retrieved3 February2016.
- ^Bernston GG, Cacioppo JT (2007)."The neuroevolution of motivation".In Gardner WL, Shah JY (eds.).Handbook of Motivation Science.New York: The Guilford Press. p. 191.ISBN978-1593855680.Archivedfrom the original on 30 March 2021.Retrieved18 November2020.
- ^Dawkins R (2009).The Greatest Show on Earth.Free Press. pp.392–395.ISBN978-1416594789.
- ^Steinkopf L (June 2016)."An Evolutionary Perspective on Pain Communication".Evolutionary Psychology.14(2): 100.doi:10.1177/1474704916653964.
- ^Sarno JE (2006).The divided mind: the epidemic of mindbody disorders.New York: ReganBooks.ISBN978-0061174308.
- ^abFillingim RB, Loeser JD, Baron R, Edwards RR (September 2016)."Assessment of Chronic Pain: Domains, Methods, and Mechanisms".The Journal of Pain.17(9 Suppl): T10–20.doi:10.1016/j.jpain.2015.08.010.PMC5010652.PMID27586827.
- ^Amico D (2016).Health & physical assessment in nursing.Boston: Pearson. p. 173.ISBN978-0133876406.
- ^Taylor C (2015).Fundamentals of nursing: the art and science of person-centered nursing care.Philadelphia: Wolters Kluwer Health. p. 241.ISBN978-1451185614.
- ^Venes D (2013).Taber's cyclopedic medical dictionary.Philadelphia: F.A. Davis. p. 1716.ISBN978-0803629776.
- ^Prkachin KM, Solomon PE, Ross J (June 2007). "Underestimation of pain by health-care providers: towards a model of the process of inferring pain in others".The Canadian Journal of Nursing Research.39(2):88–106.PMID17679587.
- ^McCaffery M. (1968).Nursing practice theories related to cognition, bodily pain, and man-environment interactions.Los Angeles: UCLA Students Store.
More recently, McCaffery defined pain as "whatever the experiencing person says it is, existing whenever the experiencing person says it does."Pasero C, McCaffery M (1999).Pain: clinical manual.St. Louis: Mosby.ISBN978-0815156093. - ^Kelly AM (May 2001)."The minimum clinically significant difference in visual analogue scale pain score does not differ with severity of pain".Emergency Medicine Journal.18(3):205–207.doi:10.1136/emj.18.3.205.PMC1725574.PMID11354213.
- ^Hawker GA, Mian S, Kendzerska T, French M (November 2011). "Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP)".Arthritis Care & Research.63(S11): S240–252.doi:10.1002/acr.20543.PMID22588748.
- ^abcLewis SM, Bucher L, Heitkemper MM, Harding M (2017).Medical-surgical nursing: Assessment and management of clinical problems(10th ed.). St. Louis, Missouri: Elsevier. p. 126.ISBN978-0323328524.OCLC944472408.
- ^abcJarvis C (2007).Physical examination & health assessment.St. Louis, Mo: Elsevier Saunders. pp.180–192.ISBN978-1455728107.
- ^Encandela JA (March 1993). "Social science and the study of pain since Zborowski: a need for a new agenda".Social Science & Medicine.36(6):783–791.doi:10.1016/0277-9536(93)90039-7.PMID8480223.
- ^Zborowski M.People in Pain.1969, San Francisco, CA:Josey-Bass[ISBN missing][page needed]
- ^Encandela JA (1997). "Social Construction of pain and aging: Individual artfulness within interpretive structures".Symbolic Interaction.20(3):251–273.doi:10.1525/si.1997.20.3.251.
- ^Lawhorne L, Passerini J (1999).Chronic Pain Management in the Long Term Care Setting: Clinical Practice Guidelines.Baltimore, Maryland: American Medical Directors Association. pp.1–27.
- ^Epstein R (19 March 2018)."When Doctors Don't Listen to Women".The New York Times.Archivedfrom the original on 9 May 2019.Retrieved20 July2019.
- ^Fasslet J (15 October 2015)."How Doctors Take Women's Pain Less Seriously".The Atlantic.Archivedfrom the original on 17 July 2019.Retrieved20 July2019.
- ^"Stories of Misunderstanding Women's Pain".The Atlantic.15 March 2016.Archivedfrom the original on 15 April 2019.Retrieved20 July2019.
- ^Panju AA, Hemmelgarn BR, Guyatt GH, Simel DL (October 1998). "The rational clinical examination. Is this patient having a myocardial infarction?".JAMA.280(14):1256–1263.doi:10.1001/jama.280.14.1256.PMID9786377.
- ^Slater EE, DeSanctis RW (May 1976). "The clinical recognition of dissecting aortic aneurysm".The American Journal of Medicine.60(5):625–633.doi:10.1016/0002-9343(76)90496-4.PMID1020750.
- ^Brown JE, Chatterjee N, Younger J, Mackey S (September 2011)."Towards a physiology-based measure of pain: patterns of human brain activity distinguish painful from non-painful thermal stimulation".PLOS ONE.6(9): e24124.Bibcode:2011PLoSO...624124B.doi:10.1371/journal.pone.0024124.PMC3172232.PMID21931652.
- ^Paddock C (15 September 2011)."Tool That Measures Pain Objectively Under Way".Medical News Today.Archivedfrom the original on 25 September 2017.Retrieved25 September2017.
- ^"Feeling pain? The computer can tell".Reuters.13 September 2011.Archivedfrom the original on 17 June 2015.Retrieved25 September2017.
Editorial
- ^Urch CE, Suzuki R (26 September 2008). "Pathophysiology of somatic, visceral, and neuropathic cancer pain". In Sykes N, Bennett MI & Yuan C-S (ed.).Clinical pain management: Cancer pain(2d ed.). London: Hodder Arnold. pp.3–12.ISBN978-0340940075.
- ^Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW, Hansson P, Hughes R, Nurmikko T, Serra J (April 2008). "Neuropathic pain: redefinition and a grading system for clinical and research purposes".Neurology.70(18):1630–1635.doi:10.1212/01.wnl.0000282763.29778.59.hdl:11573/97043.PMID18003941.S2CID30172528.
- ^Paice JA (2003)."Mechanisms and management of neuropathic pain in cancer"(PDF).The Journal of Supportive Oncology.1(2):107–120.PMID15352654.Archived fromthe original(PDF)on 7 January 2010.Retrieved8 January2010.
- ^Campbell JN, Meyer RA (October 2006)."Mechanisms of neuropathic pain".Neuron.52(1):77–92.doi:10.1016/j.neuron.2006.09.021.PMC1810425.PMID17015228.
- ^ab"Psychogenic Pain".Cleveland Clinic.Archivedfrom the original on 14 July 2011.Retrieved25 September2017.
- ^Thienhaus O, Cole BE (2002). "The classification of pain". In Weiner RS (ed.).Pain management: A practical guide for clinicians.American Academy of Pain Management. p. 29.ISBN978-0849322624.
- Main CJ, Spanswick CC (2000).Pain management: an interdisciplinary approach.Churchill Livingstone.ISBN978-0443056833.
Pain management: an interdisciplinary approach.
- Main CJ, Spanswick CC (2000).Pain management: an interdisciplinary approach.Churchill Livingstone.ISBN978-0443056833.
- ^Brown AK, Christo PJ, Wu CL (December 2004). "Strategies for postoperative pain management".Best Practice & Research. Clinical Anaesthesiology.18(4):703–717.doi:10.1016/j.bpa.2004.05.004.PMID15460554.
- ^Cullen L, Greiner J, Titler MG (June 2001). "Pain management in the culture of critical care".Critical Care Nursing Clinics of North America.13(2):151–166.doi:10.1016/S0899-5885(18)30046-7.PMID11866399.
- ^Rupp T, Delaney KA (April 2004). "Inadequate analgesia in emergency medicine".Annals of Emergency Medicine.43(4):494–503.doi:10.1016/j.annemergmed.2003.11.019.PMID15039693.
- ^Smith GF, Toonen TR (April 2007). "Primary care of the patient with cancer".American Family Physician.75(8):1207–1214.PMID17477104.
- ^Jacobson PL, Mann JD (January 2003). "Evolving role of the neurologist in the diagnosis and treatment of chronic noncancer pain".Mayo Clinic Proceedings.78(1):80–84.doi:10.4065/78.1.80.PMID12528880.
- ^Deandrea S, Montanari M, Moja L, Apolone G (December 2008)."Prevalence of undertreatment in cancer pain. A review of published literature".Annals of Oncology.19(12):1985–1991.doi:10.1093/annonc/mdn419.PMC2733110.PMID18632721.
- ^Perron V, Schonwetter RS (2001)."Assessment and management of pain in palliative care patients".Cancer Control.8(1):15–24.doi:10.1177/107327480100800103.PMID11176032.
- ^Selbst SM, Fein JA (2006)."Sedation and analgesia".In Henretig FM, Fleisher GR, Ludwig S (eds.).Textbook of pediatric emergency medicine.Hagerstwon, MD: Lippincott Williams & Wilkins.ISBN978-1605471594.Archivedfrom the original on 11 June 2016.Retrieved3 February2016.
- ^Cleeland CS (June 1998). "Undertreatment of cancer pain in elderly patients".JAMA.279(23):1914–1915.doi:10.1001/jama.279.23.1914.PMID9634265.
- ^Bonham VL (2001)."Race, ethnicity, and pain treatment: striving to understand the causes and solutions to the disparities in pain treatment"(PDF).The Journal of Law, Medicine & Ethics.29(1):52–68.doi:10.1111/j.1748-720X.2001.tb00039.x.PMID11521272.S2CID18257031.Archived fromthe original(PDF)on 19 July 2011.Retrieved7 March2022.
- ^Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Kalauokalani DA, Kaloukalani DA, Lasch KE, Myers C, Tait RC, Todd KH, Vallerand AH (September 2003)."The unequal burden of pain: confronting racial and ethnic disparities in pain"(PDF).Pain Medicine.4(3):277–294.doi:10.1046/j.1526-4637.2003.03034.x.hdl:2027.42/73822.PMID12974827.Archivedfrom the original on 30 March 2021.Retrieved2 September2019.
- ^Hoffmann DE, Tarzian AJ (2001)."The girl who cried pain: a bias against women in the treatment of pain".The Journal of Law, Medicine & Ethics.29(1):13–27.doi:10.1111/j.1748-720X.2001.tb00037.x.PMID11521267.S2CID219952180.Archivedfrom the original on 1 November 2019.Retrieved11 July2019.
- ^Delegates to the International Pain Summit of the International Association for the Study of Pain (2010)."Declaration of Montreal".Archived fromthe originalon 13 May 2011.Retrieved7 March2022.
- ^Horlocker TT, Cousins MJ, Bridenbaugh PO, Carr DL (2008).Cousins and Bridenbaugh's Neural Blockade in Clinical Anesthesia and Pain Medicine.Hagerstwon, MD: Lippincott Williams & Wilkins.ISBN978-0781773881.
- ^"Physical Medicine and Rehabilitation".Archived fromthe originalon 16 May 2008.Retrieved7 March2022.
- ^Human Rights Watch(2011)."Tens of Millions Face Death in Agony".Archivedfrom the original on 1 September 2013.Retrieved26 August2013.
- ^Mallinson TE (2017)."A review of ketorolac as a prehospital analgesic".Journal of Paramedic Practice.9(12):522–526.doi:10.12968/jpar.2017.9.12.522.Archivedfrom the original on 5 June 2018.Retrieved2 June2018.
- ^Derry CJ, Derry S, Moore RA (December 2014)."Caffeine as an analgesic adjuvant for acute pain in adults".The Cochrane Database of Systematic Reviews.12(12): CD009281.doi:10.1002/14651858.CD009281.pub3.PMC6485702.PMID25502052.
- ^Derry S, Wiffen PJ, Moore RA (July 2015)."Single dose oral ibuprofen plus caffeine for acute postoperative pain in adults".The Cochrane Database of Systematic Reviews.2019(7): CD011509.doi:10.1002/14651858.CD011509.pub2.PMC6481458.PMID26171993.
- ^Karlow N, Schlaepfer CH, Stoll CR, Doering M, Carpenter CR, Colditz GA, et al. (October 2018)."A Systematic Review and Meta-analysis of Ketamine as an Alternative to Opioids for Acute Pain in the Emergency Department".Academic Emergency Medicine.25(10):1086–1097.doi:10.1111/acem.13502.PMID30019434.
- ^Higgins C, Smith BH, Matthews K (June 2019)."Evidence of opioid-induced hyperalgesia in clinical populations after chronic opioid exposure: a systematic review and meta-analysis".British Journal of Anaesthesia.122(6):e114 –e126.doi:10.1016/j.bja.2018.09.019.PMID30915985.
- ^Fishbain DA, Pulikal A (November 2019)."Does Opioid Tapering in Chronic Pain Patients Result in Improved Pain or Same Pain vs Increased Pain at Taper Completion? A Structured Evidence-Based Systematic Review".Pain Medicine.20(11):2179–2197.doi:10.1093/pm/pny231.PMID30597076.Archivedfrom the original on 18 January 2021.Retrieved19 February2021.
- ^Stevens B, Yamada J, Ohlsson A, Haliburton S, Shorkey A (July 2016)."Sucrose for analgesia in newborn infants undergoing painful procedures".The Cochrane Database of Systematic Reviews.7(2): CD001069.doi:10.1002/14651858.CD001069.pub5.PMC6457867.PMID27420164.
- ^Lasky RE, van Drongelen W (October 2010). "Is sucrose an effective analgesic for newborn babies?".Lancet.376(9748):1201–1203.doi:10.1016/S0140-6736(10)61358-X.PMID20817245.S2CID18724497.
- ^Harrison D, Stevens B, Bueno M, Yamada J, Adams-Webber T, Beyene J, Ohlsson A (June 2010)."Efficacy of sweet solutions for analgesia in infants between 1 and 12 months of age: a systematic review".Archives of Disease in Childhood.95(6):406–413.doi:10.1136/adc.2009.174227.PMID20463370.
- ^Wark DM (July 2008). "What we can do with hypnosis: a brief note".The American Journal of Clinical Hypnosis.51(1):29–36.doi:10.1080/00029157.2008.10401640.PMID18714889.S2CID12240662.
- ^Elkins G, Jensen MP, Patterson DR (July 2007)."Hypnotherapy for the management of chronic pain".The International Journal of Clinical and Experimental Hypnosis.55(3):275–287.doi:10.1080/00207140701338621.PMC2752362.PMID17558718.
- ^Madsen MV, Gøtzsche PC, Hróbjartsson A (January 2009)."Acupuncture treatment for pain: systematic review of randomised clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups".BMJ.338:a3115.doi:10.1136/bmj.a3115.PMC2769056.PMID19174438.
- ^Chiu HY, Hsieh YJ, Tsai PS (March 2017)."Systematic review and meta-analysis of acupuncture to reduce cancer-related pain".European Journal of Cancer Care.26(2): e12457.doi:10.1111/ecc.12457.PMID26853524.S2CID20096639.
- ^Chang SC, Hsu CH, Hsu CK, Yang SS, Chang SJ (February 2017). "The efficacy of acupuncture in managing patients with chronic prostatitis/chronic pelvic pain syndrome: A systemic review and meta-analysis".Neurourology and Urodynamics.36(2):474–481.doi:10.1002/nau.22958.PMID26741647.S2CID46827576.
- ^Ji M, Wang X, Chen M, Shen Y, Zhang X, Yang J (2015)."The Efficacy of Acupuncture for the Treatment of Sciatica: A Systematic Review and Meta-Analysis".Evidence-Based Complementary and Alternative Medicine.2015:192808.doi:10.1155/2015/192808.PMC4575738.PMID26425130.
- ^Gagnier JJ, Oltean H, van Tulder MW, Berman BM, Bombardier C, Robbins CB (January 2016). "Herbal Medicine for Low Back Pain: A Cochrane Review".Spine.41(2):116–133.doi:10.1097/BRS.0000000000001310.PMID26630428.
- ^abRubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW (September 2012)."Spinal manipulative therapy for acute low-back pain".The Cochrane Database of Systematic Reviews.2012(9): CD008880.doi:10.1002/14651858.CD008880.pub2.PMC6885055.PMID22972127.
- ^Straube S, Andrew Moore R, Derry S, McQuay HJ (January 2009). "Vitamin D and chronic pain".Pain.141(1–2):10–13.doi:10.1016/j.pain.2008.11.010.PMID19084336.S2CID17244398.
- ^"IASP Position Statement on the Use of Cannabinoids to Treat Pain".iasp-pain.Retrieved10 May2024.
- ^Cordell WH, Keene KK, Giles BK, Jones JB, Jones JH, Brizendine EJ (May 2002). "The high prevalence of pain in emergency medical care".The American Journal of Emergency Medicine.20(3):165–169.doi:10.1053/ajem.2002.32643.PMID11992334.
- ^Hasselström J, Liu-Palmgren J, Rasjö-Wrååk G (2002). "Prevalence of pain in general practice".European Journal of Pain.6(5):375–385.doi:10.1016/S1090-3801(02)00025-3.PMID12160512.S2CID798849.
- ^Abu-Saad Huijer H (2010). "Chronic pain: a review".Le Journal Medical Libanais. The Lebanese Medical Journal.58(1):21–27.PMID20358856.
- ^Smith AK, Cenzer IS, Knight SJ, Puntillo KA, Widera E, Williams BA, Boscardin WJ, Covinsky KE (November 2010)."The epidemiology of pain during the last 2 years of life".Annals of Internal Medicine.153(9):563–569.doi:10.7326/0003-4819-153-9-201011020-00005.PMC3150170.PMID21041575.
- ^Perquin CW, Hazebroek-Kampschreur AA, Hunfeld JA, Bohnen AM, van Suijlekom-Smit LW, Passchier J, van der Wouden JC (July 2000). "Pain in children and adolescents: a common experience".Pain.87(1):51–58.doi:10.1016/S0304-3959(00)00269-4.PMID10863045.S2CID9813003.
- ^Foucault M (2007).Security, Territory, Population: Lectures at the College de France, 1977–78.Palgrave Macmillan. p. 1.
- ^abcEinolf C (2007)."The Fall and Rise of Torture: A Comparative and Historical Analysis".Social Theory.25(2):101–121.doi:10.1111/j.1467-9558.2007.00300.x.JSTOR20453071.S2CID53345959.
- ^Morinis A (1985)."The ritual experience: pain and the transformation of consciousness in ordeals of initiation".Ethos.13(2):150–174.doi:10.1525/eth.1985.13.2.02a00040.JSTOR639985.
- ^Atkinson M, Young K (2001). "Flesh journeys: neo primitives and the contemporary rediscovery of radical body modification".Deviant Behavior.22(2):117–146.doi:10.1080/016396201750065018.S2CID146525156.
- ^Loland S, Skirstad B, Waddington I, eds. (2006).Pain and injury in sport: Social and ethical analysis.London and New York: Routledge. pp.17–20.ISBN978-0415357043.
- ^Narayan MC (April 2010)."Culture's effects on pain assessment and management".The American Journal of Nursing.110(4):38–47.doi:10.1097/01.NAJ.0000370157.33223.6d.PMID20335689.
- ^Working party of the Nuffield Council on Bioethics (2005)."The ethics of research involving animals. London: Nuffield Council on Bioethics."ISBN978-1904384106.Archived from the original on 25 June 2008. Retrieved 12 January 2010.
- ^Rollin BE (June 2007)."Animal research: a moral science. Talking Point on the use of animals in scientific research".EMBO Reports.8(6):521–525.doi:10.1038/sj.embor.7400996.PMC2002540.PMID17545990.
- ^Rollin B (1989).The Unheeded Cry: Animal Consciousness, Animal Pain, and Science.New York: Oxford University Press. pp.117–118.cited inCarbone L (2004).What animals want: expertise and advocacy in laboratory animal welfare policy.US: Oxford University Press. p. 150.
- ^Griffin DR, Speck GB (January 2004). "New evidence of animal consciousness".Animal Cognition.7(1):5–18.doi:10.1007/s10071-003-0203-x.PMID14658059.S2CID8650837.
- ^abSherwin CM (February 2001)."Can invertebrates suffer? Or, how robust is argument-by-analogy?".Animal Welfare.10(1):103–118.doi:10.1017/S0962728600023551.S2CID54126137.Archivedfrom the original on 7 March 2022.Retrieved22 December2021.
- ^Lockwood JA (1987). "The Moral Standing of Insects and the Ethics of Extinction".The Florida Entomologist.70(1):70–89.doi:10.2307/3495093.JSTOR3495093.
- ^DeGrazia D, Rowan A (September 1991). "Pain, suffering, and anxiety in animals and humans".Theoretical Medicine.12(3):193–211.doi:10.1007/BF00489606.PMID1754965.S2CID34920699.
- ^"Do Invertebrates Feel Pain?".The Senate Standing Committee on Legal and Constitutional Affairs.TheParliament of Canada.Archived fromthe originalon 6 January 2010.Retrieved11 June2008.
- ^Smith JA (1991)."A Question of Pain in Invertebrates".Institute for Laboratory Animal Research Journal.33:1–2.Archivedfrom the original on 8 October 2011.
- ^Abbott FV, Franklin KB, Westbrook FR (January 1995). "The formalin test: scoring properties of the first and second phases of the pain response in rats".Pain.60(1):91–102.doi:10.1016/0304-3959(94)00095-V.PMID7715946.S2CID35448280.
- ^Jones JM, Foster W, Twomey CR, Burdge J, Ahmed OM, Pereira TD, et al. (August 2020)."A machine-vision approach for automated pain measurement at millisecond timescales".eLife.9:e57258.doi:10.7554/eLife.57258.PMC7434442.PMID32758355.
- ^abcPetruzzello, Melissa (2016)."Do Plants Feel Pain?".Encyclopedia Britannica.Retrieved8 January2023.
Given that plants do not have pain receptors, nerves, or a brain, they do not feel pain as we members of the animal kingdom understand it. Uprooting a carrot or trimming a hedge is not a form of botanical torture, and you can bite into that apple without worry.
- ^Draguhn, Andreas; Mallatt, Jon M.; Robinson, David G. (2021)."Anesthetics and plants: no pain, no brain, and therefore no consciousness".Protoplasma.258(2). Springer:239–248.doi:10.1007/s00709-020-01550-9.PMC7907021.PMID32880005.32880005.
Further reading
edit- Casey K (2019).Chasing Pain: The Search for a Neurobiological Mechanism.New York: Oxford University Press.ISBN978-0190880231.
- Parshall, Allison,"Pain Language: The sound of 'ow' transcends borders",Scientific American,vol. 332, no. 2 (February 2025), pp. 16–18.