Status epilepticus(SE), orstatus seizure,is a medical condition consisting of a singleseizurelasting more than 5 minutes, or 2 or more seizures within a 5-minute period without the person returning to normal between them.[3][1]Previous definitions used a 30-minute time limit.[2]The seizures can be of thetonic–clonic type,with a regular pattern of contraction and extension of the arms and legs, or of types that do not involve contractions, such asabsence seizuresorcomplex partial seizures.[1]Status epilepticus is a life-threatening medical emergency, particularly if treatment is delayed.[1]
| Status epilepticus | |
|---|---|
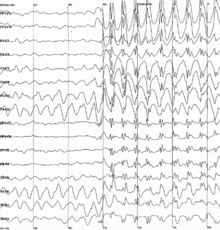 | |
| Generalized 3 Hzspike-and-wavedischarges on anelectroencephalogram | |
| Specialty | Emergency medicine,neurology |
| Symptoms | Regular pattern of contraction and extension of the arms and legs, movement of one part of the body, unresponsive[1] |
| Duration | >5 minutes[1] |
| Risk factors | Epilepsy,underlying problem with thebrain[2] |
| Diagnostic method | Blood sugar,imaging of the head, blood tests,electroencephalogram[1] |
| Differential diagnosis | Psychogenic nonepileptic seizures,movement disorders,meningitis,delirium[1] |
| Treatment | Benzodiazepines,fosphenytoin,phenytoin,[1]paraldehyde(rarely used) |
| Prognosis | ~20% thirty-day risk of death[1] |
| Frequency | 40 per 100,000 people per year[2] |
Status epilepticus may occur in those with a history ofepilepsyas well as those with an underlying problem of thebrain.[2]These underlying brain problems may include trauma, infections, orstrokes,among others.[2][4]Diagnosis often involves checking theblood sugar,imaging of the head, a number of blood tests, and anelectroencephalogram.[1]Psychogenic nonepileptic seizuresmay present similarly to status epilepticus.[1]Other conditions that may also appear to be status epilepticus includelow blood sugar,movement disorders,meningitis,anddelirium,among others.[1]Status epilepticus can also appear whentuberculous meningitisbecomes very severe.
Benzodiazepinesare the preferred initial treatment, after which typicallyphenytoinis given.[1]Possible benzodiazepines include intravenouslorazepamas well as intramuscular injections ofmidazolam.[5]A number of other medications may be used if these are not effective, such asphenobarbital,propofol,orketamine.[1]After initial treatment with benzodiazepines, typical antiseizure drugs should be given, includingvalproic acid(valproate),fosphenytoin,levetiracetam,or a similar substance(s).[6]While empirically based treatments exist, few head-to-head clinical trials exist, so the best approach remains undetermined.[6]This said, "consensus-based" best practices are offered by the Neurocritical Care Society.[6]Intubationmay be required to help maintain the person'sairway.[1]Between 10% and 30% of people who have status epilepticus die within 30 days.[1]The underlying cause, the person's age, and the length of the seizure are important factors in the outcome.[2]Status epilepticus occurs in up to 40 per 100,000 people per year.[2]Those with status epilepticus make up about 1% of people who visit the emergency department.[1]
Signs and symptoms
editStatus epilepticus can be divided into two categories: convulsive and nonconvulsive (NCSE).[1]
Convulsive
editConvulsive status epilepticus presents an urgentneurological condition,which is characterized by an elongated and uncontrollable onsets of seizures in which a regular pattern of contraction and extension of the arms and legs will be observed from the patient.[1][7]The symptoms can be managed by initially introducing a seizure suppressing medication as the first stage of the treatment, which optimally works only for that stage because any delay will reduce the efficacy of those medications. Convulsive status epilepticus commonly affects the elderly and young children, with a mortality rate of up to 20–30% of elderly patients and 0–3% of young children. Patients who survive initial onset are often left with cognitive and neurological defects.[7]
Epilepsia partialis continuais a variant involving hour-, day-, or even week-long jerking. It is a consequence ofvascular disease,tumors,orencephalitis,and is drug-resistant.[citation needed]
Generalizedmyoclonusis commonly seen incomatosepeople followingcardiopulmonary resuscitation(CPR) and is seen by some as an indication of catastrophic damage to theneocortex;myoclonus status in this situation can usually (but not always) be considered anagonalphenomenon.[8]
Refractory status epilepticus is defined as status epilepticus that continues despite treatment with benzodiazepines and oneantiepileptic drug.[9]
Super-refractory status epilepticus is defined as status epilepticus that continues or recurs 24 hours or more after the onset of anaesthetic therapy, including those cases where status epilepticus recurs on the reduction or withdrawal of anesthesia.[10]
Nonconvulsive
editNonconvulsive status epilepticus is a relatively long duration change in a person'slevel of consciousnesswithout large-scale bending and extension of the limbs due to seizure activity.[11]It is of two main types with either prolongedcomplex partial seizuresorabsence seizures.[11]Up to a quarter of cases of SE are nonconvulsive.[11]
In the case ofcomplex partial status epilepticus,the seizure is confined to a small area of the brain, normally thetemporal lobe.Absence status epilepticus is marked by a generalized seizure affecting the whole brain. Anelectroencephalogram(EEG) is needed to differentiate between the two conditions.
The cases of nonconvulsive status epilepticus are characterized by a long-lastingstupor,staring, and unresponsiveness. Recent studies indicated 50% of cases involve patients that are semi-conscious in a way that they can respond but are confused spontaneously. Only 6% have shown a decelerated thought process. About 44% of cases of nonconvulsive status epilepticus are marked by a prolonged or fragmentarycoma.[12]
Causes
editThis sectionneeds additional citations forverification.(April 2020) |
Only 25% of people who experience seizures or status epilepticus have epilepsy.[13]The following is a list of possible causes:
- Stroke[13]
- Hemorrhage[13]
- Intoxicants[13]or adverse reactions to drugs
- Insufficient dosageor sudden withdrawal of a medication (especiallyanticonvulsants)
- Insufficient dosage or sudden withdrawal of benzodiazepine(s) medication (akin to alcohol withdrawal); itself a class of antiseizure/anticonvulsant medications
- Consumption of alcoholic beverages while on an anticonvulsant, oralcohol withdrawal
- Dieting or fasting while on an anticonvulsant
- Starting on a new medication that reduces the effectiveness of the anticonvulsant or changes drug metabolism, decreasing itshalf-life,leading to decreased blood concentrations
- Developing a resistanceto an anticonvulsant already being used
- Gastroenteritiswhile on an anticonvulsant, where lower levels of anticonvulsant may exist in the bloodstream due to vomiting of gastric contents or reduced absorption due to mucosal edema
- Developing a new, unrelated condition in which seizures are coincidentally also a symptom, but are not controlled by an anticonvulsant already used
- Metabolic disturbances—such as affected kidney and liver[13]
- Sleep deprivationof more than a short duration is often the cause of a (usually, but not always, temporary) loss of seizure control
- Dehydration– moderate- to severe, especially when combined with any single factor above
Diagnosis
editDiagnostic criteria vary, though most practitioners diagnose as status epilepticus for: one continuous, unremitting seizure lasting longer than five minutes,[14]or recurrent seizures without regaining consciousness between seizures for greater than five minutes.[1]Previous definitions used a 30-minute time limit.[2]
Nonconvulsive status epilepticus is believed to be under-diagnosed.[15]
New-onset refractory status epilepticus (NORSE) is defined as status epilepticus that does not respond to an anticonvulsant and lacks an obvious cause after two days of investigation.[16][17]
Treatments
editBenzodiazepinesare the preferred initial treatment after which typicallyphenytoinorfosphenytoinis given.[1][6]First aid guidelines for seizures state that, as a rule, an ambulance should be called for seizures lasting longer than five minutes (or sooner if this is the person's first seizure episode and no precipitating factors are known, or if said SE happens to a person with epilepsy whose seizures were previously absent or well-controlled for a considerable time).[18]
Benzodiazepines
editWhen given intravenously,lorazepamappears to be superior todiazepamfor stopping seizure activity.[5][19]Intramuscularmidazolamappears to be a reasonable alternative especially in those who are not in hospital.[5]
The benzodiazepine of choice in North America for initial treatment is lorazepam, due to its relatively long duration of action (2–8 hours) when injected, and particularly due to its rapid onset of action, which is thought to be due to its high affinity forGABA receptorsand lowlipidsolubility.This causes the drug to remain in thevascular compartment.If lorazepam is not available, or intravenous access is not possible, then diazepam should be given.[20]Alternatively, medication, such asglucagon,should be given through the bone (intraosseously).[6]
In several countries outside North America, such as theNetherlands,[21]intravenousclonazepamis regarded as the drug of first choice.[21]Cited advantages of clonazepam include a longer duration of action than diazepam and a lower propensity for the development of acute tolerance than lorazepam.[22]The use of clonazepam for this indication is not recognized in North America, perhaps because it is not available as an intravenous formulation there.[22]
Particularly in children, another popular treatment choice is midazolam, given into theside of the mouthor thenose.[23]Sometimes, the failure of lorazepam alone is considered to be enough to classify a case of SE as refractory–that is, resistant to treatment.
Phenytoin and fosphenytoin
editPhenytoinwas once another first-line therapy,[24]although theprodrugfosphenytoincan be administered three times as fast and with far fewer injection site reactions. If these or any otherhydantoin derivativesare used, then cardiac monitoring is necessary if they are administered intravenously. Because the hydantoins take 15–30 minutes to work, a benzodiazepine or barbiturate is often coadministered. Because of diazepam's short duration of action, they were often administered together anyway.[25]At present, these remain recommended second-line, follow-up treatments in the acute setting per guidelines by groups like Neurocritical Care Society (United States).[6]
Barbiturates
editBefore the benzodiazepines were invented, barbiturates were used for purposes similar to benzodiazepines in general. Some are still used today in SE[clarification needed],for instance, if benzodiazepines or the hydantoins are not an option. These are used to induce abarbituriccoma. The barbiturate most commonly used for this isphenobarbital.Thiopentalorpentobarbitalmay also be used for that purpose if the seizures have to be stopped immediately or if the person has already been compromised by the underlying illness or toxic/metabolic-induced seizures;[6]however, in those situations, thiopental is the agent of choice.[26]That said, even when benzodiazepines are available, certain algorithms–including in the United States–indicate the use of phenobarbital as a second- or third-line treatment in SE. Such use isadjunctive.At least one U.S. study showed phenobarbital, when used alone, controlled about 60% of seizures, hence its preference as an add-on therapy.[6]
Carbamazepine and valproate
editValproateis available to be given intravenously, and may be used for status epilepticus.Carbamazepineis not available in an intravenous formulation, and does not play a role in status epilepticus.[24]It was found that all of valproate, phenobarbital, fosphenytoin (phenytoin), midazolam or levetiracetam are considered to the second line drugs after benzodiazepine is used as the first line treatment. It was found that especially valproate in contrast to antiepileptic drugs is more effective to the treatment of nonconvulsive status epilepticus and more commonly used for it.[27]
Others
editIf this proves ineffective or if barbiturates cannot be used for some reason, then ageneral anestheticsuch aspropofol[28]may be tried; sometimes it is used second after the failure of lorazepam.[29]This would entail putting the person onartificial ventilation.Propofol has been shown to be effective in suppressing the jerks seen inmyoclonusstatus epilepticus.[30]
Ketamine,anNMDA antagonistdrug, can be used as a last resort for drug-resistant status epilepticus.[31]
Lidocainehas been used in cases that do not improve with other more typical medications.[32]One concern is that seizures often begin again 30 minutes after it is stopped.[32]Additionally, it is not recommended in those with heart or liver problems.[32]
Prognosis
editWhile sources vary, about 16 to 20% of first-time SE patients die;[6]with other sources indicating between 10 and 30% of such patients die within 30 days.[1]Further, 10-50% of first-time SE patients experience lifelong disabilities.[6]In the 30% mortality figure, the great majority of these people have an underlying brain condition causing their status seizure such asbrain tumor,brain infection, brain trauma, orstroke.People with diagnosed epilepsy who have a status seizure also have an increased risk of death if their condition is not stabilized quickly, their medication and sleep regimen adapted and adhered to, and stress and other stimulant (seizure trigger) levels controlled. However, with optimal neurological care, adherence to the medication regimen, and a goodprognosis(no other underlying uncontrolled brain or other organic disease), the person—even people who have been diagnosed with epilepsy—in otherwise good health can survive with minimal or no brain damage, and can decrease risk of death and even avoid future seizures.[13]
Prognosis of refractory status epilepticus
A different prognosis method was developed for refractory status epilepticus (RSE). Prognosis studies have shown that there is no clear structure of the symptoms; since they range fromgastrointestinalto flu-like symptoms, which are considered to be mild and only represent 10%, while the remaining majority of 90% of the clinical cases were unknown.[clarification needed]It was found that it takes a period of 1 to 14 days for the patient to reach theprodromal stagein which the episode is yet to come for the first time. It was found that the frequency of those initial seizures starts from a short and inconsistent seizures that lasts for a few hours and may extend to few days. It can simply strike to hundreds of seizures per day, which is the stage that needed an urgent medical intervene in which the patient expected to be in theintensive care unit(ICU) as soon as possible. Typically focal seizures are the most common among those cases.[33]
Epidemiology
editIn theUnited States,about 40 cases of SE occur annually per 100,000 people.[2]This includes about 10–20% of all first seizures.[34]
Prevalence
It was found that status epilepticus is more prevalent among African Americans than Caucasian Americans by threefold in North London, and that Asian children have recorded a relatively higher susceptibility of developing the more severe form offebrile seizures.These ethnic distribution rates indicate the genetic contribution to the susceptibility of status epilepticus. Also, studies have shown that status epilepticus is more common in males.[34]
Aetiology
Many studies have found out that age is the most related factor to the etiology of status epilepticus, since 52% of febrile seizures was found in children, while for adultsacute cerebralvascularcases was more common, side by side withhypoxiaand other metabolic causes.[34]
Research
editAllopregnanolonewas being studied as a treatment for super-resistant status epilepticus,[35]but was found to have no benefit over placebo.[36][37]
See also
editReferences
edit- ^abcdefghijklmnopqrstuvAl-Mufti, F; Claassen, J (Oct 2014). "Neurocritical Care: Status Epilepticus Review".Critical Care Clinics.30(4): 751–764.doi:10.1016/j.ccc.2014.06.006.PMID25257739.
- ^abcdefghiTrinka, E; Höfler, J; Zerbs, A (September 2012). "Causes of status epilepticus".Epilepsia.53(Suppl 4): 127–38.doi:10.1111/j.1528-1167.2012.03622.x.PMID22946730.S2CID5294771.
- ^Drislane, Frank (19 March 2020). Garcia, Paul; Edlow, Jonathan (eds.). "Convulsive status epilepticus in adults: Classification, clinical features, and diagnosis".UpToDate.34.2217. Wolters Kluwer.
- ^Trinka, E., Cock, H., Hesdorffer, D., Rossetti, A. O., Scheffer, I. E., Shinnar, S., Shorvon, S., & Lowenstein, D. H. (2015). A definition and classification of status epilepticus--Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia, 56(10), 1515–1523.doi:10.1111/epi.13121
- ^abcPrasad, M; Krishnan, PR; Sequeira, R; Al-Roomi, K (Sep 10, 2014)."Anticonvulsant therapy for status epilepticus".The Cochrane Database of Systematic Reviews.2014(9): CD003723.doi:10.1002/14651858.CD003723.pub3.PMC7154380.PMID25207925.
- ^abcdefghijDrislane, Frank (15 June 2021). Garcia, Paul; Edlow, Jonathan (eds.). "Convulsive status epilepticus in adults: Treatment and prognosis: Initial Treatment".UpToDate.52.96933. Wolters Kluwer.
- ^abSánchez Fernández, I., Goodkin, H. P., & Scott, R. C. (2019). Pathophysiology of convulsive status epilepticus. Seizure, 68, 16–21.doi:10.1016/j.seizure.2018.08.002
- ^Wijdicks, Eelco F. M.; Parisi, J. E.; Sharbrough, F. W. (February 1994). "Prognostic value of myoclonus status in comatose survivors of cardiac arrest".Annals of Neurology.35(2): 239–43.doi:10.1002/ana.410350219.PMID8109907.S2CID42680232.
- ^Rossetti, AO; Lowenstein, DH (October 2011)."Management of refractory status epilepticus in adults: still more questions than answers".The Lancet. Neurology.10(10): 922–30.doi:10.1016/s1474-4422(11)70187-9.PMC3202016.PMID21939901.
- ^Shorvon Simon, Ferlisi Monica (2011)."A Critical Review of Available Therapies and a Clinical Treatment Protocol".Brain.134(10): 2802–2818.doi:10.1093/brain/awr215.PMID21914716.
- ^abcChang, AK; Shinnar, S (Feb 2011). "Nonconvulsive status epilepticus".Emergency Medicine Clinics of North America.29(1): 65–72.doi:10.1016/j.emc.2010.08.006.PMID21109103.
- ^(Woodford, H. J., George, J., & Jackson, M. (2015). Non-convulsive status epilepticus: a practical approach to diagnosis in confused older people. Postgraduate medical journal, 91(1081), 655–661.doi:10.1136/postgradmedj-2015-133537
- ^abcdefStasiukyniene, V.; Pilvinis, V.; Reingardiene, D.; Janauskaite, L. (2009)."[Epileptic seizures in critically ill patients]".Medicina.45(6): 501–7.doi:10.3390/medicina45060066.PMID19605972.
- ^Nair, PP; Kalita, J.; Misra, U. K. (Jul–Sep 2011)."Status epilepticus: why, what, and how".Journal of Postgraduate Medicine.57(3): 242–52.doi:10.4103/0022-3859.81807.PMID21941070.
- ^Rubin, Diana; Stephan, Ruegg; Stephan, Marsch; Christian, Schindler; Leticia, Grize; Raoul, Sutter (August 24, 2011). "High prevalence of nonconvulsive and subtle status epilepticus in an ICU of a tertiary care center: A three-year observational cohort study".Epilepsy Research.96(1): 140–150.doi:10.1016/j.eplepsyres.2011.05.018.PMID21676592.S2CID25684463.
- ^"NORSE (New Onset Refractory Status Epilepticus) and FIRES (Febrile Infection-Related Epilepsy Syndrome)".National Organization for Rare Disorders.Retrieved2021-12-07.
- ^"New-Onset Refractory Status Epilepticus (NORSE)".Epilepsy Foundation.Retrieved2021-12-07.
- ^Migdady, I., Rosenthal, E. S., & Cock, H. R. (2022). Management of status epilepticus: a narrative review. Anaesthesia, 77 Suppl 1, 78–91.https://www.researchgate.net/publication/357706108_Management_of_status_epilepticus_a_narrative_review
- ^Zhao, ZY; Wang, HY; Wen, B; Yang, ZB; Feng, K; Fan, JC (28 March 2016). "A Comparison of Midazolam, Lorazepam, and Diazepam for the Treatment of Status Epilepticus in Children: A Network Meta-analysis".Journal of Child Neurology.31(9): 1093–107.doi:10.1177/0883073816638757.PMID27021145.S2CID7677504.
- ^Pang, Trudy; Lawrence J. Hirsch (July 2005). "Treatment of Convulsive and Nonconvulsive Status Epilepticus".Current Treatment Options in Neurology.7(4): 247–259.doi:10.1007/s11940-005-0035-x.PMID15967088.S2CID31286223.
- ^ab"22.8 Convulsive status epilepticus"(PDF).Acute Boekje(in Dutch) (4th ed.). Van Zuiden Communications B.V. 2009. p. 276.ISBN978-90-8523-197-4.[permanent dead link]
- ^abLawn, Nicholas D; Wijdicks, Eelco FM (2002). "Status epilepticus: A critical review of management options".Neurol J Southeast Asia.7:47–59.
- ^Walker, D. M.; Teach, S. J. (June 2006). "Update on the acute management of status epilepticus in children".Curr Opin Pediatr.18(3): 239–44.doi:10.1097/01.mop.0000193306.55635.24.PMID16721142.S2CID42391321.
- ^abBeran, RG. (April 2008). "An alternative perspective on the management of status epilepticus".Epilepsy Behav.12(3): 349–53.doi:10.1016/j.yebeh.2007.12.013.hdl:10072/22410.PMID18262847.S2CID42219786.
- ^Crawshaw, A. A., & Cock, H. R. (2020). Medical management of status epilepticus: Emergency room to intensive care unit. Seizure, 75, 145–152.doi:10.1016/j.seizure.2019.10.006
- ^Lee S. K. (2020). Diagnosis and Treatment of Status Epilepticus. Journal of epilepsy research, 10(2), 45–54.doi:10.14581/jer.20008
- ^Lee S. K. (2020). Diagnosis and Treatment of Status Epilepticus. Journal of epilepsy research, 10(2), 45–54.doi:10.14581/jer.20008
- ^Pourrat, X; J.M. Serekian, D. Antier, J. Grassin (June 9, 2001). "Generalized tonic-clonic status epilepticus: therapeutic strategy".Presse Médicale.30(20): 1031–6.PMID11433696.
{{cite journal}}:CS1 maint: multiple names: authors list (link)(French). - ^Marik, Paul E.; Joseph Varon (2004). "The management of status epilepticus".Chest.126(2): 582–91.doi:10.1378/chest.126.2.582.PMID15302747.S2CID29378123.
- ^Wijdicks, Eelco F. M. (July 2002)."Propofol in myoclonus status epilepticus in comatose patients following cardiac resuscitation".Journal of Neurology, Neurosurgery, and Psychiatry.73(1): 94–5.doi:10.1136/jnnp.73.1.94.PMC1757284.PMID12082068.
- ^Gomes, D; Pimentel, J; Bentes, C; Aguiar de Sousa, D; Antunes, AP; Alvarez, A; Silva, ZC (31 October 2018)."Consensus Protocol for the Treatment of Super-Refractory Status Epilepticus".Acta Médica Portuguesa.31(10): 598–605.doi:10.20344/amp.9679.PMID30387431.
- ^abcSchmutzhard, E; Pfausler, B (Oct 2011)."Complications of the management of status epilepticus in the intensive care unit".Epilepsia.52(Suppl 8): 39–41.doi:10.1111/j.1528-1167.2011.03233.x.PMID21967359.S2CID205692349.
- ^Sculier, C., & Gaspard, N. (2019). New onset ref,ractory status epilepticus (NORSE). Seizure, 68, 72–78.doi:10.1016/j.seizure.2018.09.018
- ^abcShorvon, S., & Sen, A. (2020). What is status epilepticus and what do we know about its epidemiology?. Seizure, 75, 131–136.doi:10.1016/j.seizure.2019.10.003
- ^"A Study Using SAGE-547 for Super Resistant Status Epilepticus".Mayo Clinic.Archivedfrom the original on 2017-03-08.Retrieved2017-03-07.
- ^"Sage Therapeutics Reports Top-Line Results from Phase 3 STATUS Trial of Brexanolone in Super-Refractory Status Epilepticus".Sage Therapeutics, Inc.12 September 2017.Retrieved16 September2024.
- ^"Brexanolone - Sage Therapeutics".AdisInsight.
External links
edit- Evidence-Based Guideline: Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society
- Thomas, SanjeevV; Cherian, Ajith (2009)."Status epilepticus".Annals of Indian Academy of Neurology.12(3): 140–53.doi:10.4103/0972-2327.56312.PMC2824929.PMID20174493.