Monocytesare a type of leukocyte orwhite blood cell.They are the largest type of leukocyte in blood and candifferentiateintomacrophagesand monocyte-deriveddendritic cells.As a part of thevertebrateinnate immune systemmonocytes also influenceadaptive immune responsesand exert tissue repair functions. There are at least three subclasses of monocytes inhumanbloodbased on their phenotypic receptors.
| Monocyte | |
|---|---|
 3D rendering of a monocyte | |
 | |
| Details | |
| System | Immune system |
| Identifiers | |
| MeSH | D009000 |
| TH | H2.00.04.1.02010 |
| FMA | 62864 |
| Anatomical terms of microanatomy | |
Structure
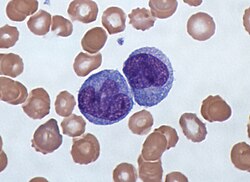
editMonocytes areamoeboidin appearance, and have nongranulatedcytoplasm.[1]Thus they are classified asagranulocytes,although they might occasionally display someazurophil granulesand/orvacuoles.With a diameter of 15–22μm,monocytes are the largest cell type inperipheral blood.[2][3]Monocytes are mononuclear cells and the ellipsoidal nucleus is often lobulated/indented, causing a bean-shaped or kidney-shaped appearance.[4]Monocytes compose 2% to 10% of all leukocytes in the human body.
Development
editMonocytes are produced by thebone marrowfrom precursors calledmonoblasts,bipotent cells that differentiated fromhematopoietic stem cells.[5]Monocytes circulate in the bloodstream for about one to three days and then typically migrate into tissues throughout the body where they differentiate intomacrophagesanddendritic cells.
Subpopulations
editIn humans
editThe first clear description of monocyte subsets by flow cytometry dates back to the late 1980s, when a population ofCD16-positive monocytes was described.[6][7]Today, three types of monocytes are recognized in human blood:[8]
- The classical monocyte is characterized by high level expression of theCD14cell surface receptor (CD14++CD16−monocyte)
- The non-classical monocyte shows low level expression ofCD14and additional co-expression of theCD16receptor (CD14+CD16++monocyte).[9]
- The intermediate monocyte expresses high levels ofCD14and low levels ofCD16(CD14++CD16+monocytes).
While in humans the level of CD14 expression can be used to differentiate non-classical and intermediate monocytes, the slan (6-Sulfo LacNAc) cell surface marker was shown to give an unequivocal separation of the two cell types.[10][11]
Ghattas et al. state that the "intermediate" monocyte population is likely to be a unique subpopulation of monocytes, as opposed to a developmental step, due to their comparatively high expression of surface receptors involved in reparative processes (includingvascular endothelial growth factorreceptors type 1 and 2,CXCR4,andTie-2) as well as evidence that the "intermediate" subset is specifically enriched in the bone marrow.[12]
In mice
editIn mice, monocytes can be divided in two subpopulations. Inflammatory monocytes (CX3CR1low,CCR2pos,Ly6Chigh,PD-L1neg), which are equivalent to human classical CD14++CD16−monocytes and resident monocytes (CX3CR1high,CCR2neg,Ly6Clow,PD-L1pos), which are equivalent to human non-classical CD14+CD16+monocytes. Resident monocytes have the ability to patrol along the endothelium wall in the steady state and under inflammatory conditions.[13][14][15][16]
Function
editMonocytes are mechanically active cells[17]and migrate from blood to an inflammatory site to perform their functions. As explained before, they can differentiate into macrophages and dendritic cells, but the different monocyte subpopulations can also exert specific functions on their own. In general, monocytes and their macrophage and dendritic cell progeny serve three main functions in the immune system. These arephagocytosis,antigen presentation, andcytokineproduction.Phagocytosisis the process of uptake of microbes and particles followed by digestion and destruction of this material. Monocytes can perform phagocytosis using intermediary (opsonising) proteins such asantibodiesorcomplementthat coat the pathogen, as well as by binding to the microbe directly viapattern recognition receptorsthat recognize pathogens. Monocytes are also capable of killing infected host cells viaantibody-dependent cell-mediated cytotoxicity.Vacuolizationmay be present in a cell that has recently phagocytized foreign matter.
Differentiation into other effector cells
editMonocytes can migrate into tissues and replenish residentmacrophagepopulations. Macrophages have a high antimicrobial and phagocytic activity and thereby protect tissues from foreign substances. They are cells that possess a large smooth nucleus, a large area of cytoplasm, and many internalvesiclesfor processing foreign material. Although they can be derived from monocytes, a large proportion is already formed prenatally in theyolk sacand foetal liver.[18]
In vitro,monocytes can differentiate intodendritic cellsby adding the cytokinesgranulocyte macrophage colony-stimulating factor(GM-CSF) andinterleukin 4.[19]Such monocyte-derived cells do, however, retain the signature of monocytes in theirtranscriptomeand they cluster with monocytes and not with bona fide dendritic cells.[20]
Specific functions of monocyte subpopulations
editAside from their differentiation capacity, monocytes can also directly regulate immune responses. As explained before, they are able to perform phagocytosis. Cells of the classical subpopulation are the most efficient phagocytes and can additionally secrete inflammation-stimulating factors. The intermediate subpopulation is important forantigen presentationandT lymphocytestimulation.[21]Briefly, antigen presentation describes a process during which microbial fragments that are present in the monocytes after phagocytosis are incorporated into MHC molecules. They are then trafficked to the cell surface of the monocytes (or macrophages or dendritic cells) and presented as antigens to activate T lymphocytes, which then mount a specific immune response against the antigen. Non-classical monocytes produce high amounts of pro-inflammatorycytokinesliketumor necrosis factorandinterleukin-12after stimulation with microbial products. Furthermore, a monocyte patrolling behavior has been demonstrated in humans both for the classical and the non-classical monocytes, meaning that they slowly move along theendotheliumto examine it for pathogens.[22]Said et al. showed that activated monocytes express high levels ofPD-1which might explain the higher expression of PD-1 in CD14+CD16++monocytes as compared to CD14++CD16−monocytes. Triggering monocytes-expressed PD-1 by itsligandPD-L1 induces IL-10 production, which activatesCD4Th2 cellsand inhibitsCD4Th1 cellfunction.[23] Many factors produced by other cells can regulate thechemotaxisand other functions of monocytes. These factors include most particularlychemokinessuch asmonocyte chemotactic protein-1(CCL2) andmonocyte chemotactic protein-3 (CCL7);certainarachidonic acidmetabolites such asleukotriene B4and members of the5-hydroxyicosatetraenoic acid and 5-oxo-eicosatetraenoic acidfamily of OXE1 receptor agonists (e.g.,5-HETEand 5-oxo-ETE); andN-Formylmethionine leucyl-phenylalanineand other N-formylatedoligopeptideswhich are made by bacteria and activate theformyl peptide receptor 1.[24] Other microbial products can directly activate monocytes and this leads to production of pro-inflammatory and, with some delay, of anti-inflammatorycytokines.Typical cytokines produced by monocytes areTNF,IL-1,andIL-12.
Clinical significance
editAmonocyte countis part of acomplete blood countand is expressed either as a percentage of monocytes among all white blood cells or as absolute numbers. Both may be useful, but these cells became valid diagnostic tools only when monocyte subsets are determined. Monocytic cells may contribute to the severity and disease progression in COVID-19 patients.[25]
Monocytosis
editMonocytosisis the state of excess monocytes in the peripheral blood. It may be indicative of various disease states. Examples of processes that can increase a monocyte count include:
- chronic inflammation
- diabetes[26]
- stressresponse[27]
- Cushing's syndrome(hyperadrenocorticism)
- immune-mediated disease
- granulomatousdisease
- atherosclerosis[28]
- necrosis
- red blood cellregeneration
- viral fever
- sarcoidosis
- chronic myelomonocytic leukemia(CMML)
- Resolution offasting[29]
A high count of CD14+CD16++monocytes is found in severe infection (sepsis).[30]
In the field of atherosclerosis, high numbers of the CD14++CD16+intermediate monocytes were shown to be predictive of cardiovascular events in populations at risk.[31][32]
CMML is characterized by a persistent monocyte count of > 1000/microL of blood. Analysis of monocyte subsets has demonstrated predominance of classical monocytes and absence of CD14lowCD16+ monocytes.[33][34]The absence of non-classical monocytes can assist in diagnosis of the disease and the use of slan as a marker can improve specificity.[35]
Monocytopenia
editMonocytopeniais a form ofleukopeniaassociated with a deficiency of monocytes. A very low count of these cells is found after therapy with immuno-suppressiveglucocorticoids.[36]
Also, non-classical slan+ monocytes are strongly reduced in patients withhereditary diffuse leukoencephalopathy with spheroids,a neurologic disease associated with mutations in the macrophage colony-stimulating factor receptor gene.[10]
Blood content
editSee also
editFurther reading
edit- Jakubzick, C. V., Randolph, G. J., & Henson, P. M. (2017).Monocyte differentiation and antigen-presenting functions.In:Nature Reviews Immunology.doi:10.1038/nri.2017.28
References
edit- ^Nichols, Barbara A.; Bainton, Dorothy Ford; Farquhar, Marilyn G. (1 August 1971)."Differentiation of monocytes".Journal of Cell Biology.50(2): 498–515.doi:10.1083/jcb.50.2.498.PMC2108281.PMID4107019.
- ^Palmer, L.; Briggs, C.; McFadden, S.; Zini, G.; Burthem, J.; Rozenberg, G.; Proytcheva, M.; Machin, S. J. (2015). "ICSH recommendations for the standardization of nomenclature and grading of peripheral blood cell morphological features".International Journal of Laboratory Hematology.37(3): 287–303.doi:10.1111/ijlh.12327.ISSN1751-5521.PMID25728865.
- ^Steve, Paxton; Michelle, Peckham; Adele, Knibbs (28 April 2018)."The Leeds Histology Guide".leeds.ac.uk.Archivedfrom the original on 11 October 2017.Retrieved28 April2018.
- ^Zini, Gina (2021). "How I investigate difficult cells at the optical microscope".International Journal of Laboratory Hematology.43(3): 346–353.doi:10.1111/ijlh.13437.ISSN1751-5521.PMID33342036.
- ^Monga I, Kaur K, Dhanda S (March 2022). "Revisiting hematopoiesis: applications of the bulk and single-cell transcriptomics dissecting transcriptional heterogeneity in hematopoietic stem cells".Briefings in Functional Genomics.21(3): 159–176.doi:10.1093/bfgp/elac002.PMID35265979.
- ^Ziegler-Heitbrock, H W Loems; Passlick, Bernward; Flieger, Dimitri (December 1988). "The Monoclonal Antimonocyte Antibody My4 Stains B Lymphocytes and Two Distinct Monocyte Subsets in Human Peripheral Blood".Hybridoma.7(6): 521–527.doi:10.1089/hyb.1988.7.521.PMID2466760.
- ^Passlick, Bernward; Flieger, Dimitri; Ziegler-Heitbrock, H W Loems (November 1989)."Characterization of a human monocyte subpopulation coexpressing CD14 and CD16 antigens".Blood.74(7): 2527–2534.doi:10.1182/blood.V74.7.2527.2527.PMID2478233.
- ^Ziegler-Heitbrock, Loems; Ancuta, Petronela; Crowe, Suzanne; Dalod, Marc; Grau, Veronika; Hart, Derek N.; Leenen, Pieter J. M.; Liu, Yong-Jun; MacPherson, Gordon; Randolph, Gwendalyn J.; Scherberich, Juergen; Schmitz, Juergen; Shortman, Ken; Sozzani, Silvano; Strobl, Herbert; Zembala, Marek; Austyn, Jonathan M.; Lutz, Manfred B. (21 October 2010). "Nomenclature of monocytes and dendritic cells in blood".Blood.116(16): e74–e80.doi:10.1182/blood-2010-02-258558.hdl:11379/41075.PMID20628149.S2CID1570404.
- ^Ziegler-Heitbrock, Loems (March 2007)."The CD14+ CD16+ blood monocytes: their role in infection and inflammation".Journal of Leukocyte Biology.81(3): 584–592.doi:10.1189/jlb.0806510.PMID17135573.S2CID31534841.
- ^abHofer, Thomas P.; Zawada, Adam M.; Frankenberger, Marion; Skokann, Kerstin; Satzl, Anna A.; Gesierich, Wolfgang; Schuberth, Madeleine; Levin, Johannes; Danek, Adrian; Rotter, Björn; Heine, Gunnar H.; Ziegler-Heitbrock, Loems (10 December 2015)."slan-defined subsets of CD16-positive monocytes: impact of granulomatous inflammation and M-CSF receptor mutation".Blood.126(24): 2601–2610.doi:10.1182/blood-2015-06-651331.PMID26443621.
- ^Hofer, Thomas P.; van de Loosdrecht, Arjan A.; Stahl-Hennig, Christiane; Cassatella, Marco A.; Ziegler-Heitbrock, Loems (13 September 2019)."6-Sulfo LacNAc (Slan) as a Marker for Non-classical Monocytes".Frontiers in Immunology.10:2052.doi:10.3389/fimmu.2019.02052.PMC6753898.PMID31572354.
- ^Ghattas, Angie; Griffiths, Helen R.; Devitt, Andrew; Lip, Gregory Y.H.; Shantsila, Eduard (October 2013)."Monocytes in Coronary Artery Disease and Atherosclerosis".Journal of the American College of Cardiology.62(17): 1541–1551.doi:10.1016/j.jacc.2013.07.043.PMID23973684.
- ^Carlin, Leo M.; Stamatiades, Efstathios G.; Auffray, Cedric; Hanna, Richard N.; Glover, Leanne; Vizcay-Barrena, Gema; Hedrick, Catherine C.; Cook, H. Terence; Diebold, Sandra; Geissmann, Frederic (April 2013)."Nr4a1-Dependent Ly6Clow Monocytes Monitor Endothelial Cells and Orchestrate Their Disposal".Cell.153(2): 362–375.doi:10.1016/j.cell.2013.03.010.PMC3898614.PMID23582326.
- ^Auffray, Cedric; Fogg, Darin; Garfa, Meriem; Elain, Gaelle; Join-Lambert, Olivier; Kayal, Samer; Sarnacki, Sabine; Cumano, Ana; Lauvau, Gregoire; Geissmann, Frederic (3 August 2007). "Monitoring of Blood Vessels and Tissues by a Population of Monocytes with Patrolling Behavior".Science.317(5838): 666–670.Bibcode:2007Sci...317..666A.doi:10.1126/science.1142883.PMID17673663.S2CID46067303.
- ^Imhof, Beat A.; Jemelin, Stephane; Ballet, Romain; Vesin, Christian; Schapira, Marc; Karaca, Melis; Emre, Yalin (16 August 2016)."CCN1/CYR61-mediated meticulous patrolling by Ly6C low monocytes fuels vascular inflammation".Proceedings of the National Academy of Sciences.113(33): E4847–E4856.Bibcode:2016PNAS..113E4847I.doi:10.1073/pnas.1607710113.PMC4995973.PMID27482114.
- ^Bianchini, Mariaelvy; Duchêne, Johan; Santovito, Donato; Schloss, Maximilian J.; Evrard, Maximilien; Winkels, Holger; Aslani, Maria; Mohanta, Sarajo K.; Horckmans, Michael; Blanchet, Xavier; Lacy, Michael; von Hundelshausen, Philipp; Atzler, Dorothee; Habenicht, Andreas; Gerdes, Norbert; Pelisek, Jaroslav; Ng, Lai Guan; Steffens, Sabine; Weber, Christian; Megens, Remco T. A. (21 June 2019)."PD-L1 expression on nonclassical monocytes reveals their origin and immunoregulatory function".Science Immunology.4(36): eaar3054.doi:10.1126/sciimmunol.aar3054.PMID31227596.S2CID195259881.
- ^Evers, Tom M.J.; Sheikhhassani, Vahid; Haks, Mariëlle C.; Storm, Cornelis; Ottenhoff, Tom H.M.; Mashaghi, Alireza (2022)."Single-cell analysis reveals chemokine-mediated differential regulation of monocyte mechanics".iScience.25(1): 103555.Bibcode:2022iSci...25j3555E.doi:10.1016/j.isci.2021.103555.PMC8693412.PMID34988399.
- ^Murphy, Kenneth; Weaver, Casey (2018). "Grundbegriffe der Immunologie".Janeway Immunologie(in German). Berlin, Heidelberg: Springer Berlin Heidelberg. pp. 3–46.doi:10.1007/978-3-662-56004-4_1.ISBN978-3-662-56003-7.PMC7844863.
- ^Sallusto, F; Cella, M; Danieli, C; Lanzavecchia, A (1 August 1995)."Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and bacterial products".Journal of Experimental Medicine.182(2): 389–400.doi:10.1084/jem.182.2.389.PMC2192110.PMID7629501.
- ^Robbins, Scott H; Walzer, Thierry; Dembélé, Doulaye; Thibault, Christelle; Defays, Axel; Bessou, Gilles; Xu, Huichun; Vivier, Eric; Sellars, MacLean; Pierre, Philippe; Sharp, Franck R; Chan, Susan; Kastner, Philippe; Dalod, Marc (2008)."Novel insights into the relationships between dendritic cell subsets in human and mouse revealed by genome-wide expression profiling".Genome Biology.9(1): R17.doi:10.1186/gb-2008-9-1-r17.PMC2395256.PMID18218067.
- ^Wong, Kok Loon; Tai, June Jing-Yi; Wong, Wing-Cheong; Han, Hao; Sem, Xiaohui; Yeap, Wei-Hseun; Kourilsky, Philippe; Wong, Siew-Cheng (2011-08-04). "Gene expression profiling reveals the defining features of the classical, intermediate, and nonclassical human monocyte subsets".Blood.118(5): e16–e31.doi:10.1182/blood-2010-12-326355.ISSN0006-4971.PMID21653326.
- ^Collison, Joanna L.; Carlin, Leo M.; Eichmann, Martin; Geissmann, Frederic; Peakman, Mark (1 August 2015)."Heterogeneity in the Locomotory Behavior of Human Monocyte Subsets over Human Vascular Endothelium In Vitro".The Journal of Immunology.195(3): 1162–1170.doi:10.4049/jimmunol.1401806.PMID26085686.
- ^Said, Elias A; Dupuy, Franck P; Trautmann, Lydie; Zhang, Yuwei; Shi, Yu; El-Far, Mohamed; Hill, Brenna J; Noto, Alessandra; Ancuta, Petronela; Peretz, Yoav; Fonseca, Simone G; Van Grevenynghe, Julien; Boulassel, Mohamed R; Bruneau, Julie; Shoukry, Naglaa H; Routy, Jean-Pierre; Douek, Daniel C; Haddad, Elias K; Sekaly, Rafick-Pierre (April 2010)."Programmed death-1–induced interleukin-10 production by monocytes impairs CD4+ T cell activation during HIV infection".Nature Medicine.16(4): 452–459.doi:10.1038/nm.2106.PMC4229134.PMID20208540.
- ^Sozzani, S.; Zhou, D.; Locati, M.; Bernasconi, S.; Luini, W.; Mantovani, A.; O'Flaherty, J. T. (15 November 1996)."Stimulating properties of 5-oxo-eicosanoids for human monocytes: synergism with monocyte chemotactic protein-1 and -3".The Journal of Immunology.157(10): 4664–4671.doi:10.4049/jimmunol.157.10.4664.PMID8906847.S2CID23499393.
- ^Gómez-Rial, Jose; Rivero-Calle, Irene; Salas, Antonio; Martinón-Torres, Federico (22 July 2020)."Role of Monocytes/Macrophages in Covid-19 Pathogenesis: Implications for Therapy".Infection and Drug Resistance.13:2485–2493.doi:10.2147/IDR.S258639.PMC7383015.PMID32801787.
- ^Hoyer, FF; Zhang, X; Coppin, E; Vasamsetti, SB; Modugu, G; Schloss, MJ; Rohde, D; McAlpine, CS; Iwamoto, Y; Libby, P; Naxerova, K; Swirski, F; Dutta, P; Nahrendorf, P (April 2020)."Bone Marrow Endothelial Cells Regulate Myelopoiesis in Diabetes".Circulation.142(3): 244–258.doi:10.1161/CIRCULATIONAHA.120.046038.PMC7375017.PMID32316750.
- ^Heidt, Timo; Sager, Hendrik B; Courties, Gabriel; Dutta, Partha; Iwamoto, Yoshiko; Zaltsman, Alex; von zur Muhlen, Constantin; Bode, Christoph; Fricchione, Gregory L; Denninger, John; Lin, Charles P; Vinegoni, Claudio; Libby, Peter; Swirski, Filip K; Weissleder, Ralph; Nahrendorf, Matthias (July 2014)."Chronic variable stress activates hematopoietic stem cells".Nature Medicine.20(7): 754–758.doi:10.1038/nm.3589.PMC4087061.PMID24952646.
- ^Swirski, Filip K.; Libby, Peter; Aikawa, Elena; Alcaide, Pilar; Luscinskas, F. William; Weissleder, Ralph; Pittet, Mikael J. (2 January 2007)."Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata".Journal of Clinical Investigation.117(1): 195–205.doi:10.1172/JCI29950.PMC1716211.PMID17200719.
- ^O’Brien, Conan J.O.; Domingos, Ana I. (2023). "Old and" hangry "monocytes turn from friend to foe under assault".Immunity.56(4): 747–749.doi:10.1016/j.immuni.2023.03.013.PMID37044065.
- ^Fingerle, G; Pforte, A; Passlick, B; Blumenstein, M; Strobel, M; Ziegler- Heitbrock, Hw (15 November 1993)."The novel subset of CD14+/CD16+ blood monocytes is expanded in sepsis patients".Blood.82(10): 3170–3176.doi:10.1182/blood.v82.10.3170.3170.PMID7693040.
- ^Heine, G.H.; Ulrich, C.; Seibert, E.; Seiler, S.; Marell, J.; Reichart, B.; Krause, M.; Schlitt, A.; Köhler, H.; Girndt, M. (March 2008)."CD14++CD16+ monocytes but not total monocyte numbers predict cardiovascular events in dialysis patients".Kidney International.73(5): 622–629.doi:10.1038/sj.ki.5002744.PMID18160960.
- ^Rogacev, Kyrill S.; Cremers, Bodo; Zawada, Adam M.; Seiler, Sarah; Binder, Nadine; Ege, Philipp; Große-Dunker, Gunnar; Heisel, Isabel; Hornof, Florian; Jeken, Jana; Rebling, Niko M.; Ulrich, Christof; Scheller, Bruno; Böhm, Michael; Fliser, Danilo; Heine, Gunnar H. (October 2012)."CD14++CD16+ Monocytes Independently Predict Cardiovascular Events".Journal of the American College of Cardiology.60(16): 1512–1520.doi:10.1016/j.jacc.2012.07.019.PMID22999728.
- ^Vuckovic, S.; Fearnley, D. B.; Gunningham, S.; Spearing, R. L.; Patton, W. N.; Hart, D. N. J. (June 1999)."Dendritic cells in chronic myelomonocytic leukaemia: Dendritic Cells in CMML".British Journal of Haematology.105(4): 974–985.doi:10.1046/j.1365-2141.1999.01431.x.PMID10554809.S2CID22571555.
- ^Selimoglu-Buet, Dorothée; Wagner-Ballon, Orianne; Saada, Véronique; Bardet, Valérie; Itzykson, Raphaël; Bencheikh, Laura; Morabito, Margot; Met, Elisabeth; Debord, Camille; Benayoun, Emmanuel; Nloga, Anne-Marie; Fenaux, Pierre; Braun, Thorsten; Willekens, Christophe; Quesnel, Bruno; Adès, Lionel; Fontenay, Michaela; Rameau, Philippe; Droin, Nathalie; Koscielny, Serge; Solary, Eric (4 June 2015)."Characteristic repartition of monocyte subsets as a diagnostic signature of chronic myelomonocytic leukemia".Blood.125(23): 3618–3626.doi:10.1182/blood-2015-01-620781.PMC4497970.PMID25852055.
- ^Tarfi, Sihem; Badaoui, Bouchra; Freynet, Nicolas; Morabito, Margot; Lafosse, Jeffie; Toma, Andréa; Etienne, Gabriel; Micol, Jean-Baptiste; Sloma, Ivan; Fenaux, Pierre; Solary, Eric; Selimoglu-Buet, Dorothée; Wagner-Ballon, Orianne (April 2020)."Disappearance of slan-positive non-classical monocytes for diagnosis of chronic myelomonocytic leukemia with an associated inflammatory state".Haematologica.105(4): e147–e152.doi:10.3324/haematol.2019.219782.PMID31413091.S2CID199663779.
- ^Fingerle-Rowson, G; Angstwurm, M; Andreesen, R; Ziegler-Heitbrock, HW (June 1998)."Selective depletion of CD14 + CD16 + monocytes by glucocorticoid therapy: Depletion of CD14+ CD16+ monocytes by glucocorticoids".Clinical & Experimental Immunology.112(3): 501–506.doi:10.1046/j.1365-2249.1998.00617.x.PMC1904988.PMID9649222.
External links
edit- Histology image: 01702ooa– Histology Learning System at Boston University
- Human Monocytes — Prof. Dr. Ziegler-Heitbrock
- Circulation of Body Fluids