Atenololis abeta blockermedication primarily used to treathigh blood pressureandheart-associated chest pain.[7]Although used to treat high blood pressure, it does not seem to improvemortalityin those with the condition.[8][9]Other uses include the prevention ofmigrainesand treatment of certainirregular heart beats.[7][10]It is takenorally(by mouth) or byintravenous injection(injection into a vein).[7][10]It can also be used with otherblood pressure medications.[10]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Tenormin, others |
| Other names | ICI-66082; ICI66082 |
| AHFS/Drugs | Monograph |
| MedlinePlus | a684031 |
| License data | |
| Pregnancy category |
|
| Routes of administration | Oral,intravenous |
| Drug class | Selectiveβ1receptorantagonist |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokineticdata | |
| Bioavailability | 50–60%[2][3] |
| Protein binding | 6–16%[4] |
| Metabolism | Minimal (~5%)[4][5][6] |
| Metabolites | • Hydroxyatenolol[3] • Atenolol glucuronide[3] |
| Onset of action | IV:<5 minutes[4] Oral:<1 hour[4] |
| Eliminationhalf-life | 6–7 hours[4] |
| Duration of action | >24 hours[4] |
| Excretion | Oral:urine(40–50%),feces(50%)[3][4] IV:urine (85–100%), feces (10%)[3][4] |
| Identifiers | |
| |
| CAS Number | |
| PubChemCID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard(EPA) | |
| ECHA InfoCard | 100.044.941 |
| Chemical and physical data | |
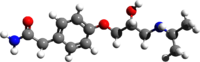
| Formula | C14H22N2O3 |
| Molar mass | 266.341g·mol−1 |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Commonside effectsincludefeeling tired,heart failure,dizziness,depression,andshortness of breath.[7]Other serious side effects includebronchial spasm.[7]Use is not recommended duringpregnancy[7]and alternative drugs are preferred whenbreastfeeding.[11]It works by blockingβ1-adrenergic receptorsin theheart,thus decreasingheart rate,force of heart beats,andblood pressure.[7]
Atenolol was patented in 1969 and approved for medical use in 1975.[12]It is on theWorld Health Organization's List of Essential Medicines.[13]It is available as ageneric medication.[7]In 2022, it was the 63rd most commonly prescribed medication in the United States, with more than 10million prescriptions.[14][15]
Medical uses
editAtenolol is used for a number of conditions includinghyperthyroidism,[16]hypertension,angina,long QT syndrome,acute myocardial infarction,supraventricular tachycardia,ventricular tachycardia,essential tremor (ET),and the symptoms ofalcohol withdrawal.[17]
The role for β-blockers in general in hypertension was downgraded in June 2006 in the United Kingdom, and later in the United States, as they are less appropriate than other agents such asACE inhibitors,calcium channel blockers,thiazidediuretics andangiotensin receptor blockers,particularly in the elderly.[18][19][20]
Available forms
editAtenolol is available in the form of 25, 50, and 100mgoraltablets.[21][4]It is also available in the form of oral tablets containing acombinationof 50 or 100mg atenolol and 50mgchlortalidone.[21]Atenolol was previously available in a 0.5mg/mL solution forinjectionas well, but this formulation was discontinued.[21]
Side effects
editHypertension treated with a β-blocker such as atenolol, alone or in conjunction with a thiazide diuretic, is associated with a higher incidence of new onset type 2 diabetes mellitus compared to those treated with an ACE inhibitor or angiotensin receptor blocker.[22][23]
β-blockers, of which atenolol is mainly studied, provides weaker protection againststrokeand mortality in patients over 60 years old compared to other antihypertensive medications.[24][25][26][18]Diureticsmay be associated with better cardiovascular and cerebrovascular outcomes than β-blockers in the elderly.[27]
Rarely, atenolol has been associated with induction of acutedelirium.[28][2][29]
Overdose
editSymptoms ofoverdoseare due to excessive pharmacodynamic actions on β1and also β2-receptors. These includebradycardia(slow heartbeat), severehypotensionwithshock,acuteheart failure,hypoglycemiaand bronchospastic reactions. Treatment is largely symptomatic. Hospitalization and intensive monitoring is indicated.Activated charcoalis useful to absorb the drug.Atropinewill counteract bradycardia,glucagonhelps with hypoglycemia,dobutaminecan be given against hypotension and the inhalation of a β2-mimetic such ashexoprenalinorsalbutamolwill terminate bronchospasms. Blood or plasma atenolol concentrations may be measured to confirm a diagnosis of poisoning in hospitalized patients or to assist in a medicolegal death investigation. Plasma levels are usually less than 3 mg/L during therapeutic administration, but can range from 3–30 mg/L in overdose victims.[30][31]
Interactions
editInteractionswith atenolol includecatecholamine-depleting drugslikereserpine,calcium channel blockers,disopyramide,amiodarone,clonidine,prostaglandin synthase inhibitorslikeindomethacin,anddigitalis glycosides.[32]Most of these interactions involve either additive cardiovascular effects or reduction of atenolol's effects.[32]
Atenolol is mainlyeliminatedrenallywithout beingmetabolizedby theliveror bycytochrome P450enzymes.[32][5][33]As a result, it has little or no potential for cytochrome P450-related drug interactions, for instance withinhibitorsandinducersof these enzymes.[5][33]Accordingly, the broad/non-selectivecytochrome P450 inhibitorcimetidinehad no effect on atenolol levels, whereas cimetidine has been found to significantly increasemetoprololandpropranolollevels.[5]
Beta blockers like atenolol can reduce or block thecardiovasculareffects ofsympathomimeticsandamphetamines,such ashypertensionandtachycardia.[34][35][36][37][38][39][40]
Atenolol has been found to be safe in combination with thenon-selectivemonoamine oxidase inhibitor(MAOI)phenelzineand actually improvedorthostatic hypotensionandhypertensivereactions with phenelzine.[41][42][43]However, more research is still needed to assess whether addition of a beta blocker like atenolol to MAOI therapy is safe and effective for improving orthostatic hypotension with MAOIs.[41][43]
Pharmacology
editPharmacodynamics
editAtenolol is abeta blocker;that is, anantagonistof theβ-adrenergic receptors.[44][4]It is specifically aselectiveantagonist of theβ1-adrenergic receptorwith nointrinsic sympathomimetic activity(i.e.,partial agonistactivity) ormembrane-stabilizing activity.[44][4]However, the preferential action of atenolol is not absolute, and at high doses, it can also blockβ2-adrenergic receptors.[4]
Beta-blocking effects of atenolol include reduction inrestingandexerciseheart rateandcardiac output,reduction ofsystolicanddiastolic blood pressureat rest and with exercise, inhibition oftachycardiainduced byisoproterenol(a non-selective β-adrenergic receptoragonist), and reduction ofreflexorthostatic tachycardia.[4]
The beta-blocking effects of atenolol, as measured by reduction of exercise-related tachycardia, are apparent within 1hour and are maximal within 2 to 4hours following a single oral dose.[4]The general effects of atenolol, including beta-blocking andantihypertensiveeffects, last for at least 24hours followingoraldoses of 50 or 100mg.[4]With intravenous administration, maximal reduction in exercise-related tachycardia occurs within 5minutes and following a single 10mg dose has dissipated within 12hours.[4]Theduration of actionof atenolol is dose-related and is correlated with circulating levels of atenolol.[4]
Pharmacokinetics
editAbsorption
editTheoralbioavailabilityof atenolol is approximately 50 to 60%.[2][3]Theabsorptionof atenolol with oral administration is rapid and consistent but is incomplete.[4]About 50% of an oral dose of atenolol is absorbed from theintestines,with the restexcretedinfeces.[4]Maximal concentrationsof atenolol occur 2 to 4hours following an oral dose, whereas peak concentrations occur within 5minutes withintravenous administration.[4]Thepharmacokineticprofile of atenolol results in it having relatively consistent plasma drug levels with about 4-fold variation between individuals.[4]
Distribution
editTheplasma protein bindingof atenolol is 6 to 16%.[4]
Atenolol is classified as a beta blocker with lowlipophilicityand hence lower potential for crossing theblood–brain barrierand entering the brain.[44]This in turn may result in fewer effects in thecentral nervous systemas well as a lower risk ofneuropsychiatricside effects.[44]Only small amounts of atenolol are said to enter the brain.[2][3]The brain-to-blood ratio of atenolol was 0.2: 1 in one study, whereas the ratio for propranolol was 33: 1 in the same study.[3]
Metabolism
editAtenolol undergoes minimal or negligiblemetabolismby theliver.[4][5]It has been estimated that about 5% of atenolol is metabolized.[6]This is in contrast to other beta blockers likepropranololandmetoprolol,but is similar tonadolol.[4]In accordance with its lack of hepatic metabolism, the pharmacokinetics of atenolol are not altered inhepatic impairment,unlike the case of propranolol.[5]Twometabolitesof atenolol have been identified: hydroxyatenolol and atenolol glucuronide.[2]It has been said that it is unknown if these metabolites are active.[2]However, another source stated that hydroxyatenolol has one-tenth the beta-blocking activity of atenolol.[3]
Elimination
editInstead of by hepatic metabolism, atenolol iseliminatedfrom the blood mainly viarenalexcretion.[4]Atenolol is excreted about 40 to 50% inurineand 50% infeceswith oral administration.[3][4]Conversely, it is excreted 85 to 100% in urine unchanged and 10% in feces with intravenous administration.[3][4]Only very small amounts of hydroxyatenolol and atenolol glucuronide are found in urine with atenolol.[3]
Theelimination half-lifeof atenolol is about 6 to 7hours.[4]The half-life of atenolol does not change with continuous administration.[4]With intravenous administration, atenolol levels rapidly decline (5- to 10-fold) during the first 7hours and thereafter decline at a rate similar to that with oral administration.[4]
The elimination of atenolol is slowed inrenal impairment,with the elimination rate being closely related to theglomerular filtration rate(GFR) and with significant accumulation occurring when thecreatinineclearancerate is under 35mL/min/1.73m2.[4]At a GFR of less than 10mL/min, the half-life of atenolol increases up to 36hours.[6]
Chemistry
editAtenolol is asubstituted phenethylaminederivative.[45]It is specificallyβ-phenylethylaminewith an α-ketosubstitutionand a 4- substitution on thephenyl ring.[45]
The experimentallog Pof atenolol is 0.16 and its predicted log P ranges from −0.03 to 0.57.[45][46][47]
Atenolol is closelystructurally relatedto metoprolol and certain other beta blockers. It is also structurally related to thecatecholamineneurotransmittersepinephrine(adrenaline) andnorepinephrine(noradrenaline).
Society and culture
editChanging medical practices
editAtenolol has been given as an example of how slow healthcare providers are to change their prescribing practices in the face ofmedical evidencethat indicates that a drug is not as effective as others in treating some conditions.[48]In 2012, 33.8 million prescriptions were written to American patients for this drug.[48]In 2014, it was in the top (most common) 1% of drugs prescribed to Medicare patients.[48]Although the number of prescriptions has been declining steadily since limited evidence articles contesting its efficacy was published, it has been estimated that it would take 20 years for doctors to stop prescribing it for hypertension.[48]Despite its diminished efficacy when compared to newerantihypertensive drugs,atenolol and otherbeta blockersare still a relevant clinical choice for treating some conditions, sincebeta blockersare a diverse group of medicines with different properties that still requires further research.[18]As consequence, reasons for the popularity of beta blockers cannot be fully attributed to a slow healthcare system –patient compliancefactor, such as treatment cost and duration, also affect adherence and popularity of therapy.[49]
References
edit- ^"FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)".nctr-crs.fda.gov.FDA.Retrieved22 October2023.
- ^abcdefWadworth AN, Murdoch D, Brogden RN (September 1991). "Atenolol. A reappraisal of its pharmacological properties and therapeutic use in cardiovascular disorders".Drugs.42(3):468–510.doi:10.2165/00003495-199142030-00007.PMID1720383.
- ^abcdefghijklHeel RC, Brogden RN, Speight TM, Avery GS (June 1979). "Atenolol: a review of its pharmacological properties and therapeutic efficacy in angina pectoris and hypertension".Drugs.17(6):425–460.doi:10.2165/00003495-197917060-00001.PMID38096.
- ^abcdefghijklmnopqrstuvwxyzaaabacadae"DailyMed - TENORMIN- atenolol tablet".DailyMed.30 June 2021.Archivedfrom the original on 27 January 2022.Retrieved20 November2023.
- ^abcdefBrodde OE, Kroemer HK (2003). "Drug-drug interactions of beta-adrenoceptor blockers".Arzneimittelforschung.53(12):814–822.doi:10.1055/s-0031-1299835.PMID14732961.
Atenolol is only minimally, if at all, metabolized and renally excreted in mostly unchanged form; thus an interaction with drugs that interfere with the hepatic metabolism is not to be expected. It is also very unlikely that the genetic polymorphisms of the CYP-family might affect the pharmacokinetics of atenolol. In fact it has been shown that plasma concentrations of nonmetabolized atenolol was not significantly different between "extensive" and "poor debrisoquine metabolizers" – in contrast to the plasma concentrations of metoprolol that were significantly increased in "poor metabolizers" (Dayer et al. 1985, Lewis et al. 1985). Furthermore, in healthy volunteers cimetidine (CAS 70059- 30-2) did not affect plasma concentrations of atenolol but significantly increased plasma concentrations of metoprolol or propranolol (Kirch et al. 1981).
- ^abcKirch W, Görg KG (1982). "Clinical pharmacokinetics of atenolol--a review".Eur J Drug Metab Pharmacokinet.7(2):81–91.doi:10.1007/BF03188723.PMID6749509.
- ^abcdefgh"Atenolol Monograph for Professionals".Drugs.AHFS.Archivedfrom the original on 18 April 2019.Retrieved23 December2018.
- ^Tomiyama H, Yamashina A (2014)."Beta-Blockers in the Management of Hypertension and/or Chronic Kidney Disease".International Journal of Hypertension.2014:919256.doi:10.1155/2014/919256.PMC3941231.PMID24672712.
- ^DiNicolantonio JJ, Fares H, Niazi AK, Chatterjee S, D'Ascenzo F, Cerrato E, et al. (2015)."β-Blockers in hypertension, diabetes, heart failure and acute myocardial infarction: a review of the literature".Open Heart.2(1): e000230.doi:10.1136/openhrt-2014-000230.PMC4371808.PMID25821584.
- ^abcBritish national formulary: BNF 76(76 ed.). Pharmaceutical Press. 2018. pp.151–153.ISBN9780857113382.
- ^"Atenolol use while Breastfeeding".Drugs.Archivedfrom the original on 23 December 2018.Retrieved23 December2018.
- ^Fischer J, Ganellin CR (2006).Analogue-based Drug Discovery.John Wiley & Sons. p. 461.ISBN9783527607495.
- ^World Health Organization(2021).World Health Organization model list of essential medicines: 22nd list (2021).Geneva: World Health Organization.hdl:10665/345533.WHO/MHP/HPS/EML/2021.02.
- ^"The Top 300 of 2022".ClinCalc.Archivedfrom the original on 30 August 2024.Retrieved30 August2024.
- ^"Atenolol Drug Usage Statistics, United States, 2013 - 2022".ClinCalc.Retrieved30 August2024.
- ^Rehman B, Sanchez DP, Shah S (2021)."Atenolol".StatPearls.Treasure Island (FL): StatPearls Publishing.PMID30969666.Archivedfrom the original on 10 October 2022.Retrieved5 September2021.
- ^"Atenolol".The American Society of Health-System Pharmacists.Archivedfrom the original on 18 April 2019.Retrieved8 May2018.
- ^abcWiysonge CS, Bradley HA, Volmink J, Mayosi BM, Opie LH (January 2017)."Beta-blockers for hypertension".The Cochrane Database of Systematic Reviews.1(1): CD002003.doi:10.1002/14651858.CD002003.pub5.PMC5369873.PMID28107561.
Further research should be of high quality and should explore whether there are differences between different subtypes of beta-blockers or whether beta-blockers have differential effects on younger and older people [...] Beta-blockers were not as good at preventing the number of deaths, strokes, and heart attacks as other classes of medicines such as diuretics, calcium-channel blockers, and renin-angiotensin system inhibitors. Most of these findings come from one type of beta-blocker called atenolol. However, beta-blockers are a diverse group of medicines with different properties, and we need more well-conducted research in this area. "(p. 2-3)
- ^Ladva S (28 June 2006)."NICE and BHS launch updated hypertension guideline".National Institute for Health and Clinical Excellence.Archived fromthe originalon 11 May 2008.Retrieved19 August2012.
- ^Cruickshank JM (August 2007). "Are we misunderstanding beta-blockers".International Journal of Cardiology.120(1):10–27.doi:10.1016/j.ijcard.2007.01.069.PMID17433471.
- ^abc"Drugs@FDA: FDA-Approved Drugs".accessdata.fda.gov.Retrieved8 July2024.
- ^Lindholm LH, Ibsen H, Borch-Johnsen K, Olsen MH, Wachtell K, Dahlöf B, et al. (September 2002). "Risk of new-onset diabetes in the Losartan Intervention For Endpoint reduction in hypertension study".Journal of Hypertension.20(9):1879–86.doi:10.1097/00004872-200209000-00035.PMID12195132.S2CID23613019.
- ^Elliott WJ, Meyer PM (January 2007). "Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis".Lancet.369(9557):201–7.doi:10.1016/s0140-6736(07)60108-1.PMID17240286.S2CID37044384.
- ^Lindholm LH, Carlberg B, Samuelsson O (October 2005). "Should β blockers remain first choice in the treatment of primary hypertension? A meta-analysis".The Lancet.366(9496):1545–1553.doi:10.1016/S0140-6736(05)67573-3.PMID16257341.S2CID34364430.
- ^Khan N, McAlister FA (June 2006)."Re-examining the efficacy of beta-blockers for the treatment of hypertension: a meta-analysis".CMAJ.174(12):1737–42.doi:10.1503/cmaj.060110.PMC1471831.PMID16754904.
- ^Kuyper LM, Khan NA (May 2014)."Atenolol vs nonatenolol β-blockers for the treatment of hypertension: a meta-analysis".The Canadian Journal of Cardiology.30(5 Suppl): S47-53.doi:10.1016/j.cjca.2014.01.006.PMID24750981.
- ^Messerli FH, Grossman E, Goldbourt U (June 1998). "Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review".JAMA.279(23):1903–7.doi:10.1001/jama.279.23.1903.PMID9634263.
- ^Keller S, Frishman WH (2003). "Neuropsychiatric effects of cardiovascular drug therapy".Cardiol Rev.11(2):73–93.doi:10.1097/01.CRD.0000053453.89776.2D.PMID12620132.
- ^Arber N (October 1988)."Delirium induced by atenolol".BMJ.297(6655): 1048.doi:10.1136/bmj.297.6655.1048-b.PMC1834788.PMID3142623.
- ^DeLima LG, Kharasch ED, Butler S (July 1995). "Successful pharmacologic treatment of massive atenolol overdose: sequential hemodynamics and plasma atenolol concentrations".Anesthesiology.83(1):204–7.doi:10.1097/00000542-199507000-00025.PMID7605000.
- ^Baselt R (2008).Disposition of Toxic Drugs and Chemicals in Man(8th ed.). Foster City, Calif.: Biomedical Publications. pp.116–117.
- ^abc"TENORMIN® (atenolol) Tablets Drug Label"(PDF).Food and Drug Administration. December 2023.Retrieved8 July2024.
- ^abScheen AJ (September 2011). "Cytochrome P450-mediated cardiovascular drug interactions".Expert Opin Drug Metab Toxicol.7(9):1065–1082.doi:10.1517/17425255.2011.586337.PMID21810031.
β-Blockers still represent widely prescribed drugs as they cover a wide spectrum of CV indications. Obviously, it is not trivial which β-blocker to choose as they differ both with regard to their PD and PK profiles [82]. It is well known when comparing the characteristics of atenolol, bisoprolol, metoprolol (each β-1 selective) and carvedilol (β-1 and β-2 nonselective). Among these β-blockers, atenolol is mainly eliminated by renal excretion; bisoprolol is in part excreted as parent compound via the renal route (50%); the other 50% are hepatically metabolized; whereas metoprolol and carvedilol are metabolized by CYP2D6. DDIs are mainly observed with those β-blockers that are metabolized via CYP enzymes. However, it should be emphasized that, in general, β-blockers are well-tolerated safe drugs with a large therapeutic index [83].
- ^Richards JR, Albertson TE, Derlet RW, Lange RA, Olson KR, Horowitz BZ (May 2015). "Treatment of toxicity from amphetamines, related derivatives, and analogues: a systematic clinical review".Drug Alcohol Depend.150:1–13.doi:10.1016/j.drugalcdep.2015.01.040.PMID25724076.
- ^Vetter VL, Elia J, Erickson C, Berger S, Blum N, Uzark K, et al. (May 2008). "Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder [corrected]: a scientific statement from the American Heart Association Council on Cardiovascular Disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing".Circulation.117(18):2407–2423.doi:10.1161/CIRCULATIONAHA.107.189473.PMID18427125.
Amphetamines (Adderall, Dexedrine): Electrophysiological Effects of Amphetamines: Amphetamines have been associated with tachyarrhythmias and sudden death.113–115 Many of the electrophysiological effects of amphetamines may be initiated by the release of norepinephrine stores from presynaptic vesicles and blocking of norepinephrine reuptake.116,117 In addition, amphetamines are potent blockers of dopamine uptake and strong central nervous system stimulants. Dopaminergic Effects of Amphetamines: In addition to the β-agonist effects of amphetamines, the dopamine receptors D1 and D2 contribute to the cardiovascular effects of methamphetamine by producing a pressor response accounting for the increase in blood pressure. The D1 receptor also is involved in mediating the positive tachycardic effects of methamphetamine.117
- ^Schindler CW, Zheng JW, Tella SR, Goldberg SR (August 1992)."Pharmacological mechanisms in the cardiovascular effects of methamphetamine in conscious squirrel monkeys".Pharmacol Biochem Behav.42(4):791–796.doi:10.1016/0091-3057(92)90031-a.PMID1325059.
- ^Hassan NA, Gunaid AA, El-Khally FM, Al-Noami MY, Murray-Lyon IM (April 2005). "Khat chewing and arterial blood pressure. A randomized controlled clinical trial of Alpha -1 and selective beta-1 adrenoceptor blockade".Saudi Med J.26(4):537–541.PMID15900355.
- ^O'Connell MB, Gross CR (1990). "The effect of single-dose phenylpropanolamine on blood pressure in patients with hypertension controlled by beta blockers".Pharmacotherapy.10(2):85–91.doi:10.1002/j.1875-9114.1990.tb02554.x.PMID2349137.
- ^O'Connell MB, Gross CR (1991). "The effect of multiple doses of phenylpropanolamine on the blood pressure of patients whose hypertension was controlled with beta blockers".Pharmacotherapy.11(5):376–81.doi:10.1002/j.1875-9114.1991.tb02648.x.PMID1684039.
- ^abGadde KM, Krishnan KR (1998)."Management of Side Effects of Monoamine Oxidase Inhibitors".In Balon R (ed.).Practical Management of the Side Effects of Psychotropic Drugs.Medical Psychiatry Series. CRC Press. pp. 67–83 (71).ISBN978-0-8247-4630-8.Retrieved8 July2024.
Interestingly, in one study, orthostatic hypotension was eliminated in a group of 61 patients treated for migraine headaches with phenelzine, when a beta-blocker, atenolol, was added (15). The authors have reported that hypertensive reactions were also less frequent when the two drugs were combined. We need further experience with this combination to determine whether addition of a beta-blocker is a safe and an effective strategy for alleviation of postural hypotension in depressed patients receiving an MAOI.
- ^O'Brien P, Oyebode F (2003). "Psychotropic medication and the heart".Advances in Psychiatric Treatment.9(6):414–423.doi:10.1192/apt.9.6.414.ISSN1355-5146.
Postural hypotension is also a risk when antipsychotics are taken with β-blockers (probably because of pharmacokinetic interaction) or with diuretics (because of Na+ or volume depletion). The same hypotensive effects might be anticipated when tricyclic antidepressants or MAOIs are co-prescribed with peripheral antihypertensive agonists. One possible exception concerns phenelzine, whose hypotensive action was reversed on co-therapy with atenolol (Merikangas & Merikangas, 1995).
- ^abMerikangas KR, Merikangas JR (November 1995)."Combination monoamine oxidase inhibitor and beta-blocker treatment of migraine, with anxiety and depression".Biol Psychiatry.38(9):603–610.doi:10.1016/0006-3223(95)00077-1.PMID8573662.
- ^abcdCojocariu SA, Maștaleru A, Sascău RA, Stătescu C, Mitu F, Leon-Constantin MM (February 2021)."Neuropsychiatric Consequences of Lipophilic Beta-Blockers".Medicina (Kaunas).57(2): 155.doi:10.3390/medicina57020155.PMC7914867.PMID33572109.
- ^abc"Atenolol".PubChem.Retrieved1 August2024.
- ^"Atenolol: Uses, Interactions, Mechanism of Action".DrugBank Online.13 August 2004.Retrieved1 August2024.
- ^"DL-Atenolol".ChemSpider.21 July 2022.Retrieved1 August2024.
- ^abcdEpstein D (22 July 2017)."When Evidence Says No, But Doctors Say Yes".The Atlantic.Archivedfrom the original on 9 May 2018.Retrieved8 May2018.
- ^Choi HY, Oh IJ, Lee JA, Lim J, Kim YS, Jeon TH, et al. (November 2018)."Factors Affecting Adherence to Antihypertensive Medication".Korean Journal of Family Medicine.39(6):325–332.doi:10.4082/kjfm.17.0041.PMC6250947.PMID30384549.