Thebrachial plexusis a network of nerves (nerve plexus) formed by theanterior ramiof the lower fourcervical nervesand firstthoracic nerve(C5,C6,C7,C8,andT1). This plexus extends from thespinal cord,through thecervicoaxillary canalin the neck, over the first rib, and into thearmpit,it suppliesafferentandefferent nerve fibersto thechest,shoulder,arm,forearm,andhand.
| Brachial plexus | |
|---|---|
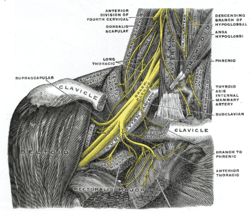 The right brachial plexus with its short branches, viewed from in front. | |
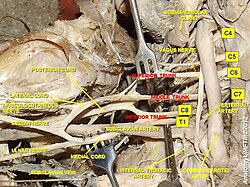 The roots, trunks and cords of the plexus shown in a dissectedcadavaricspecimen. | |
| Details | |
| Function | Network (nerveplexus) of nerves that supply the arms. |
| Identifiers | |
| Latin | plexus brachialis |
| MeSH | D001917 |
| TA98 | A14.2.03.001 |
| TA2 | 6395 |
| FMA | 5906 |
| Anatomical terms of neuroanatomy | |
Structure
editThe brachial plexus is divided into fiveroots,threetrunks,sixdivisions(three anterior and three posterior), threecords,and fivebranches.There are five "terminal" branches and numerous other "pre-terminal" or "collateral" branches, such as the subscapular nerve, the thoracodorsal nerve, and the long thoracic nerve,[1]that leave the plexus at various points along its length.[2]A common structure used to identify part of the brachial plexus in cadaver dissections is the M or W shape made by themusculocutaneous nerve,lateral cord,median nerve,medial cord, andulnar nerve.
Roots
editThe fiverootsare the fiveanterior primary ramiof thespinal nerves,after they have given off their segmental supply to the muscles of theneck. The brachial plexus emerges at five different levels: C5, C6, C7, C8, and T1. C5 and C6 merge to establish the upper trunk, C7 continuously forms the middle trunk, and C8 and T1 merge to establish the lower trunk. Prefixed or postfixed formations in some cases involve C4 or T2, respectively. Thedorsal scapular nervecomes from the superior trunk[2]and innervates therhomboid muscleswhich retract and downwardly rotate the scapula. The subclavian nerve originates in both C5 and C6 and innervates thesubclavius,a muscle that involves lifting the first ribs during respiration. The long thoracic nerve arises from C5, C6, and C7. This nerve innervates theserratus anterior,which draws the scapula laterally and is the prime mover in all forward-reaching and pushing actions.
Trunks
editThese roots merge to form thetrunks:
Divisions
editEach trunk then splits in two, to form sixdivisions:
- anterior divisions of the upper, middle, and lower trunks
- posterior divisions of the upper, middle, and lower trunks
- when observing the body in the anatomical position, the anterior divisions are superficial to the posterior divisions
Cords
editThese six divisions regroup to become the threecordsor large fiber bundles. The cords are named by their position with respect to theaxillary artery.
- Theposterior cordis formed from the three posterior divisions of the trunks (C5-C8, T1)
- Thelateral cordis formed from the anterior divisions of the upper and middle trunks (C5-C7)
- Themedial cordis simply a continuation of the anterior division of the lower trunk (C8, T1)
Diagram
edit
Branches
editThebranchesare listed below. Most branches arise from the cords, but a few branches (indicated in italics) arise directly from earlier structures. The five on the left are considered "terminal branches". These terminal branches are themusculocutaneous nerve,theaxillary nerve,theradial nerve,themedian nerve,and theulnar nerve.Due to both emerging from the lateral cord themusculocutaneous nerveand themedian nerveare well connected. Themusculocutaneous nervehas even been shown to send a branch to themedian nervefurther connecting them.[1]There have been several variations reported in the branching pattern but these are very rare.[3]
Boldindicates primary spinal root component of nerve.Italicsindicate spinal roots that frequently, but not always, contribute to the nerve.
| From | Nerve | Roots[4] | Muscles | Cutaneous |
| roots | dorsal scapular nerve | C4,C5 | rhomboid musclesandlevator scapulae | - |
| roots | long thoracic nerve | C5,C6,C7 | serratus anterior | - |
| roots | branch tophrenic nerve | C3, C4,C5 | Diaphragm | - |
| upper trunk | nerve to the subclavius | C5,C6 | subclavius muscle | - |
| upper trunk | suprascapular nerve | C5,C6 | supraspinatusandinfraspinatus | - |
| lateral cord | lateral pectoral nerve | C5,C6,C7 | pectoralis majorandpectoralis minor(by communicating with themedial pectoral nerve) | - |
| lateral cord | musculocutaneous nerve | C5, C6, C7 | coracobrachialis,brachialisandbiceps brachii | Becomes thelateral cutaneous nerve of the forearmInnervates the skin of the anterolateral forearm; elbow joint.[2] |
| lateral cord | lateral root of themedian nerve | C5,C6,C7 | fibres to the median nerve
(see below) |
- |
| posterior cord | upper subscapular nerve | C5, C6 | subscapularis(upper part) | - |
| posterior cord | thoracodorsal nerve(middle subscapular nerve) | C6,C7,C8 | latissimus dorsi | - |
| posterior cord | lower subscapular nerve | C5, C6 | subscapularis (lower part ) andteres major | - |
| posterior cord | axillary nerve | C5,C6 | anterior branch:deltoidand a small area of overlying skin posterior branch:teres minorand deltoid muscles |
posterior branch becomessuperior lateral cutaneous nerve of arm.Innervates the skin of the lateral shoulder and arm: shoulder joint.[2] |
| posterior cord | radial nerve | C5, C6, C7, C8, T1 | tricepsbrachii,supinator,anconeus,theextensormuscles of theforearm,andbrachioradialis | skin of the posterior arm and posterior forearm as the posterior cutaneous nerve of the arm and the posterior cutaneous nerve of the forearm, respectively. Also superficial branch of radial nerve supplies back of the hand, including the web of skin between the thumb and index finger. |
| medial cord | medial pectoral nerve | C8, T1 | pectoralis majorandpectoralis minor | - |
| medial cord | medial root of themedian nerve | C8, T1 | all of theflexors in the forearmexceptflexor carpi ulnarisand that part offlexor digitorum profundusthat supplies the 2nd and 3rd digits
1st and 2ndlumbricalmuscles. muscles of thethenar eminenceby a recurrent thenar branch |
portions of hand not served by ulnar or radial, i.e skin of the palmar side of thethumb,theindexandmiddle finger,half thering finger,and thenail bedof thesefingers |
| medial cord | medial cutaneous nerve of the arm | C8, T1 | - | front and medial skin of thearm |
| medial cord | medial cutaneous nerve of the forearm | C8, T1 | - | medial skin of the forearm |
| medial cord | ulnar nerve | C7, C8, T1(C7 because it supplies to the Flexor carpi ulnaris) | flexor carpi ulnaris,the medial two bellies offlexor digitorum profundus,theintrinsic hand muscles,except thethenar musclesand the two laterallumbricals of the handwhich are served by themedian nerve | the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side |
Function
editThe brachial plexus provides nerve supply to the skin and muscles of the arms, with two exceptions: thetrapeziusmuscle (supplied by thespinal accessory nerve) and an area of skin near the axilla (supplied by theintercostobrachial nerve). The brachial plexus communicates through the sympathetic trunk via gray rami communicantes that join the plexus roots.
The terminal branches of the brachial plexus (musculocutaneous n., axillary n., radial n., median n., and ulnar n.) all have specific sensory, motor and proprioceptive functions.[5][6]
| Terminal Branch | Sensory Innervation | Muscular Innervation |
|---|---|---|
| musculocutaneous nerve | Skin of the anterolateral forearm | Brachialis, biceps brachii, coracobrachialis |
| axillary nerve | Skin of lateral portion of the shoulder and upper arm | Deltoid and teres minor |
| radial nerve | Posterior aspect of the lateral forearm and wrist; posterior arm | Triceps brachii, brachioradialis, anconeus, extensor muscles of the posterior arm and forearm |
| median nerve | Skin of lateral 2/3rd of hand and the tips of digits 1-4 | Forearm flexors, thenar eminence, lumbricals of the hand 1-2 |
| ulnar nerve | Skin of palm and medial side of hand and digits 3-5 | Hypothenar eminence, some forearm flexors, thumb adductor, lumbricals 3-4, interosseous muscles |
Clinical significance
editInjury
editInjury to the brachial plexusmay affect sensation or movement of different parts of the arm. Injury can be caused by the shoulder being pushed down and the head being pulled up, which stretches or tears the nerves. Injuries associated with malpositioning commonly affect the brachial plexus nerves, rather than other peripheral nerve groups.[7][8]Due to the brachial plexus nerves being very sensitive to position, there are very limited ways of preventing such injuries. The most common victims of brachial plexus injuries consist of victims of motor vehicle accidents and newborns.[9]
Injuries can be caused by stretching, diseases, and wounds to the lateral cervical region (posterior triangle) of the neck or the axilla. Depending on the location of the injury, the signs and symptoms can range from complete paralysis to anesthesia. Testing the patient's ability to perform movements and comparing it to their normal side is a method to assess the degree of paralysis. A common brachial plexus injury is from a hard landing where the shoulder widely separates from the neck (such as in the case of motorcycle accidents or falling from a tree). These stretches can cause ruptures to the superior portions of the brachial plexus or avulse the roots from the spinal cord. Upper brachial plexus injuries are frequent in newborns when excessive stretching of the neck occurs during delivery. Studies have shown a relationship between a newborn's weight and brachial plexus injuries; however, the number of cesarean deliveries necessary to prevent a single injury is high at most birth weights.[10]
For the upper brachial plexus injuries, paralysis occurs in those muscles supplied by C5 and C6 like the deltoid, biceps, brachialis, and brachioradialis. A loss of sensation in the lateral aspect of the upper limb is also common with such injuries. An inferior brachial plexus injury is far less common but can occur when a person grasps something to break a fall or a baby's upper limb is pulled excessively during delivery. In this case, the short muscles of the hand would be affected and cause the inability to form a full fist position.[11]
To differentiate between preganglionic and postganglionic injury, clinical examination requires that the physician keep the following points in mind. Preganglionic injuries cause loss of sensation above the level of the clavicle, pain in an otherwise insensate hand, ipsilateral Horner's syndrome, and loss of function of muscles supplied by branches arising directly from roots—i.e., long thoracic nerve palsy leading to winging of scapula and elevation of ipsilateral diaphragm due to phrenic nerve palsy.
Acute brachial plexus neuritis is a neurological disorder that is characterized by the onset of severe pain in the shoulder region. Additionally, the compression of cords can cause pain radiating down the arm, numbness, paresthesia, erythema, and weakness of the hands. This kind of injury is common for people who have prolonged hyperabduction of the arm when they are performing tasks above their head.
Sports injuries
editOne sports injury that is becoming prevalent in contact sports, particularly in the sport of American football, is called a "stinger."[12]An athlete can incur this injury in a collision that can cause cervical axial compression, flexion, or extension of nerve roots or terminal branches of the brachial plexus.[13]In a study conducted on football players at United States Military Academy, researchers found that the most common mechanism of injury is, "the compression of the fixed brachial plexus between the shoulder pad and the superior medial scapula when the pad is pushed into the area ofErb's point,where the brachial plexus is most superficial. ".[14]The result of this is a "burning" or "stinging" pain that radiates from the region of the neck to the fingertips. Although this injury causes only a temporary sensation, in some cases it can cause chronic symptoms.
Penetrating wounds
editMost penetration wounds require immediate treatment and are not as easy to repair. For example, a deep knife wound to the brachial plexus could damage and/or sever the nerve. According to where the cut was made, it could inhibit action potentials needed to innervate that nerve's specific muscle or muscles.
Injuries during birth
editBrachial plexus injuries can occur during the delivery of newborns when after the delivery of the head, the anterior shoulder of the infant cannot pass below the pubic symphysis without manipulation. This manipulation can cause the baby's shoulder to stretch, which can damage the brachial plexus to varying degrees.[15]This type of injury is referred to asshoulder dystocia.Shoulder dystocia can cause obstetric brachial plexus palsy (OBPP), which is the actual injury to the brachial plexus. The incidence of OBPP in the United States is 1.5 per 1000 births, while it is lower in the United Kingdom and the Republic of Ireland (0.42 per 1000 births).[16]While there are no known risk factors for OBPP, if a newborn does have shoulder dystocia it increases their risk for OBPP 100-fold. Nerve damage has been connected tobirth weightwith largernewbornsbeing more susceptible to theinjurybut it also has to do with the delivery methods. Although very hard to prevent during livebirth,doctors must be able to deliver anewbornwith precise and gentle movements to decrease chances of injuring the child.
Tumors
editTumors that may occur in the brachial plexus areschwannomas,neurofibromasandmalignant peripheral nerve sheath tumors.
Imaging
editImaging of the Brachial Plexus can be done effectively by using a higher magnetic strength MRI Scanner like 1.5 T or more. It is impossible to evaluate the brachial plexuses with plain Xray, CT and ultrasound scanning can manage to view the plexuses to an extent; hence MRI is preferred in imaging brachial plexus over other imaging modalities due to its multiplanar capability and the tissue contrast difference between brachial plexus and adjacent vessels. The plexuses are best imaged in coronal and sagittal planes, but axial images give an idea about the nerve roots. Generally, T1 WI and T2 WI images are used in various planes for the imaging; but new sequences like MR Myelolography, Fiesta 3D and T2 cube are also used in addition to the basic sequences to gather more information to evaluate the anatomy more.
In anaesthetics
editSee also
editAdditional images
edit-
The brachial plexus surrounds thebrachial artery.
-
Nerves in the infraclavicular portion of the right brachial plexus in the axillary fossa.
-
The outermost (distal) part of the brachial plexus shown from a dissected cadaveric specimen.
-
Brachial plexus
-
Mind map showing branches of brachial plexus
-
Spinal cord. Brachial plexus. Cerebrum. Inferior view. Deep dissection.
-
Diagram of the brachial plexus using colour to illustrate the contributions of each nerve root to the branches.
-
The brachial plexus, including all branches of the C5-T1 ventral primary rami. Includes mnemonics for learning the plexus's connections and branches.
-
Mixed fibres of a spinal nerve
References
edit- ^abKawai, H; Kawabata, H (2000).Brachial Plexus Palsy.Singapore: World Scientific. pp. 6, 20.ISBN9810231393.
- ^abcdSaladin, Kenneth (2015).Anatomy and Physiology(7 ed.). New York: McGraw Hill. pp.489–491.ISBN9789814646437.
- ^Goel, Shivi; Rustagi, SM; Kumar, A; Mehta, V; Suri, RK (Mar 13, 2014)."Multiple unilateral variations in medial and lateral cords of brachial plexus and their branches".Anatomy & Cell Biology.47(1):77–80.doi:10.5115/acb.2014.47.1.77.PMC3968270.PMID24693486.
- ^Moore, K.L.; Agur, A.M. (2007).Essential Clinical Anatomy(3rd ed.). Baltimore: Lippincott Williams & Wilkins. pp.430–1.ISBN978-0-7817-6274-8.
- ^Saladin, Kenneth (2007).Anatomy and Physiology: The Unity of Form and Function.New York, NY: McGraw-Hill. pp.491.ISBN9789814646437.
- ^"Axillary Brachial Plexus Block".nysora.New York School of Regional Anesthesia. 2013-09-20. Archived fromthe originalon 2017-07-12.
- ^Cooper, DE; Jenkins, RS; Bready, L; Rockwood Jr, CA (1988). "The prevention of injuries of the brachial plexus secondary to malposition of the patient during surgery".Clinical Orthopaedics and Related Research.228(228):33–41.doi:10.1097/00003086-198803000-00005.PMID3342585.
- ^Jeyaseelan, L.; Singh, V. K.; Ghosh, S.; Sinisi, M.; Fox, M. (2013). "Iatropathic brachial plexus injury: A complication of delayed fixation of clavicle fractures".The Bone & Joint Journal.95-B(1):106–10.doi:10.1302/0301-620X.95B1.29625.PMID23307682.
- ^Midha, Rajiv (1997). "Epidemiology of Brachial Plexus Injuries in a Multitrauma Population".Neurosurgery.40(6):1182–8, discussion 1188–9.doi:10.1097/00006123-199706000-00014.PMID9179891.
- ^Ecker, Jeffrey L.; Greenberg, James A.; Norwitz, Errol R.; Nadel, Allan S.; Repke, John T. (1997). "Birth Weight as a Predictor of Brachial Plexus Injury".Obstetrics & Gynecology.89(5):643–47.doi:10.1016/S0029-7844(97)00007-0.PMID9166293.
- ^Moore, Keith (2006).Clinically Oriented Anatomy.Philadelphia: Lippincott Williams & Wilkins. pp.778–81.ISBN0-7817-3639-0.
- ^Dimberg, Elliot L.; Burns, Ted M. (July 2005)."Management of Common Neurologic Conditions in Sports".Clinics in Sports Medicine.24(3):637–662.doi:10.1016/j.csm.2005.04.002.ISSN0278-5919.
- ^Elias, Ilan (2014)."Recurrent burner syndrome due to presumed cervical spine osteoblastoma in a collision sport athlete - a case report".Journal of Brachial Plexus and Peripheral Nerve Injury.02:e61 –e65.doi:10.1186/1749-7221-2-13.PMC1904218.PMID17553154.
- ^Cunnane, M (2011)."A retrospective study looking at the incidence of 'stinger' injuries in professional rugby union players".British Journal of Sports Medicine.45(15): A19.1–A19.doi:10.1136/bjsports-2011-090606.60.Retrieved2015-02-12.
- ^"Brachial Plexus Injuries Information Page: National Institute of Neurological Disorders and Stroke (NINDS)".ninds.nih.gov.Archived fromthe originalon 2016-12-02.Retrieved2016-11-28.
- ^Doumouchtsis, Stergios K.; Arulkumaran, Sabaratnam (2009-09-01). "Are all brachial plexus injuries caused by shoulder dystocia?".Obstetrical & Gynecological Survey.64(9):615–623.doi:10.1097/OGX.0b013e3181b27a3a.ISSN1533-9866.PMID19691859.
Bibliography
edit- Saladin, Kenneth (2014).Anatomy and Physiology(7th ed.). McGraw-Hill Education. p. 491.
- Kishner, Stephen."Brachial Plexus Anatomy".Medscape.WebMD.Retrieved29 Nov2015.
External links
edit- Brachial Plexus Injury/Illustration, Cincinnati Children's Hospital Medical Center
- Learn the Brachial Plexus in Five Minutes or Less by Daniel S. Romm, M.D. and Dennis A. Chu Chu, M.D.[1]
- Video of the dissected axilla and brachial plexus