Bronchitisis inflammation of thebronchi(large and medium-sized airways) in thelungsthat causescoughing.Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms includecoughing up sputum,wheezing,shortness of breath,andchest pain.Bronchitis can beacuteorchronic.[1]
| Bronchitis | |
|---|---|
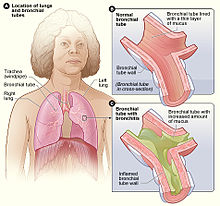 | |
| Figure A shows the location of the lungs and bronchial tubes. Figure B is an enlarged view of a normal bronchial tube. Figure C is an enlarged view of a bronchial tube with bronchitis. | |
| Pronunciation | |
| Specialty | Infectious disease,pulmonology |
| Symptoms | Coughingupmucus,wheezing,shortness of breath,chest discomfort[1] |
| Types | Acute, chronic[1] |
| Frequency | Acute:~5% of people a year[2][3] Chronic:~5% of people[3] |
Acute bronchitisusually has a cough that lasts around three weeks,[4]and is also known as a chest cold.[5]In more than 90% of cases, the cause is aviral infection.[4]These viruses may be spread through the air when people cough or by direct contact.[6]A small number of cases are caused by abacterial infectionsuch asMycoplasma pneumoniaeorBordetella pertussis.[4]Risk factors include exposure totobacco smoke,dust, and otherair pollution.[6]Treatment of acute bronchitis typically involves rest,paracetamol(acetaminophen), andnonsteroidal anti-inflammatory drugs(NSAIDs) to help with the fever.[7][8]
Chronic bronchitisis defined as aproductive cough– one that producessputum– that lasts for three months or more per year for at least two years.[9][10]Many people with chronic bronchitis also havechronic obstructive pulmonary disease(COPD).[11]Tobacco smokingis the most common cause, with a number of other factors such asair pollutionandgeneticsplaying a smaller role.[12]Treatments includequitting smoking,vaccinations,rehabilitation,and often inhaledbronchodilatorsandsteroids.[13]Some people may benefit fromlong-term oxygen therapy.[13]
Acute bronchitis is one of the more common diseases.[7][14]About 5% of adults and 6% of children have at least one episode a year.[2][15]Acute bronchitis is the most common type of bronchitis.[16]By contrast in the United States, in 2018, 9.3 million people were diagnosed with the less common chronic bronchitis.[17][18]
Acute bronchitis
editAcute bronchitis, also known as a chest cold, is short terminflammationof thebronchiof thelungs.[4][6]The most common symptom is acough,that may or may not produce sputum.[4][19]Other symptoms may includecoughing up mucus,wheezing,shortness of breath,fever,and chest discomfort.[6]Fever when present is mild.[20]The infection may last from a few to ten days.[6]The cough may persist for several weeks afterwards, with the total duration of symptoms usually around three weeks.[4][6]Symptoms may last for up to six weeks.[7]
Cause
editIn more than 90% of cases, the cause is aviral infection.[4]These viruses may spread through theair when people cough or by direct contact.[6]Risk factors include exposure totobacco smoke,dust,and otherair pollutants.[6]A small number of cases are due tobacteriasuch asMycoplasma pneumoniaeorBordetella pertussis.[4]
Diagnosis
editDiagnosis is typically based on a person's signs and symptoms.[20]The color of the sputum does not indicate if the infection is viral or bacterial.[4]Determining the underlying organism is usually not required.[4]Other causes of similar symptoms includeasthma,pneumonia,bronchiolitis,bronchiectasis,andCOPD.[2][4]Achest X-raymay be useful to detect pneumonia.[4]
Another common sign of bronchitis is a cough which lasts ten days to three weeks. If the cough lasts for longer than a month, it may become chronic bronchitis. In addition, a fever may be present. Acute bronchitis is normally caused by a viral infection. Typically, these infections arerhinovirus,adenovirus,parainfluenza,orinfluenza.No specific testing is normally needed in order to diagnose acute bronchitis.[20]
Treatment
editOne form of prevention is to avoid smoking and other lung irritants.[21]Frequent hand washing may also be protective.[21]Treatment for acute bronchitis usually involves rest,paracetamol(acetaminophen), andNSAIDsto help with the fever.[7][8]Cough medicinehas little support for its use, and is not recommended in children under the age of six.[4][22]There is tentative evidence thatsalbutamolmay be useful in treatingwheezing;however, it may result in nervousness and tremors.[4][23]Antibioticsshould generally not be used.[19]An exception is when acute bronchitis is due topertussis.[4]Tentative evidence supportshoneyandpelargoniumto help with symptoms.[4]Getting plenty of rest and drinking enough fluids are often recommended as well.[24]Chinese medicinal herbsare of unclear effect.[25]
Epidemiology
editAcute bronchitis is one of the most common diseases[7][14]and the most common type of bronchitis.[5]About 5% of adults are affected, and about 6% of children have at least one episode a year.[2][15]It occurs more often in the winter.[2]More than 10 million people in the US visit a doctor each year for this condition, with about 70% receiving antibiotics which are mostly not needed.[7]There are efforts to decrease the use of antibiotics in acute bronchitis.[14]
Chronic bronchitis
editChronic bronchitis is alower respiratory tract disease,[26]defined by aproductive coughthat lasts for three months or more per year for at least two years.[1][10]The cough is sometimes referred to as asmoker's coughsince it often results from smoking. When chronic bronchitis occurs together with decreased airflow it is known aschronic obstructive pulmonary disease(COPD).[27][26]Many people with chronic bronchitis have COPD; however, most people with COPD do not also have chronic bronchitis.[10][28]Estimates of the number of people with COPD who have chronic bronchitis are 7–40%.[29][30]Estimates of the number of people who smoke and have chronic bronchitis who also have COPD is 60%.[31]
The term "chronic bronchitis" was used in previous definitions of COPD but is no longer included in the definition.[10][32][33]The term is still used clinically.[34]While both chronic bronchitis andemphysemaare often associated with COPD, neither is needed to make the diagnosis.[34]A Chinese consensus commented on symptomatic types of COPD that include chronic bronchitis with frequent exacerbations.[35]
Chronic bronchitis is marked bymucus hypersecretionandmucins.[9][36]The excess mucus is produced by an increased number ofgoblet cells,and enlargedsubmucosal glandsin response to long-term irritation.[37]The mucous glands in the submucosa secrete more than the goblet cells.[38]Mucins thicken mucus, and their concentration has been found to be high in cases of chronic bronchitis, and also to correlate with the severity of the disease.[39]Excess mucus can narrow the airways, thereby limiting airflow and accelerating the decline in lung function, and result in COPD.[35][40]Excess mucus shows itself as a chronic productive cough and its severity and volume of sputum can fluctuate in periods of acute exacerbations.[35]In COPD, those with the chronic bronchitic phenotype with associated chronic excess mucus, experience a worse quality of life than those without.[35][41]
The increased secretions are initially cleared by coughing.[36]The cough is often worse soon after awakening, and the sputum produced may have a yellow or green color and may be streaked with specks of blood.[42]In the early stages, a cough can maintain mucus clearance. However, with continued excessive secretion mucus clearance is impaired, and when the airways become obstructed a cough becomes ineffective.[43]Effectivemucociliary clearancedepends on airway hydration, ciliary beating, and the rates of mucin secretion. Each of these factors is impaired in chronic bronchitis.[44]Chronic bronchitis can lead to a higher number ofexacerbationsand a faster decline in lung function.[40][45]TheICD-11lists chronic bronchitis with emphysema (emphysematous bronchitis) as a "certain specified COPD".[46][47]
Cause
editMost cases of chronic bronchitis are caused bytobacco smoking.[48][49]Chronic bronchitis in young adults who smoke is associated with a greater chance of developing COPD.[50]There is an association between smokingcannabisand chronic bronchitis.[51][52]In addition, chronic inhalation ofair pollution,or irritating fumes or dust from hazardous exposures in occupations such as coal mining, grain handling, textile manufacturing, livestock farming,[53]and metal moulding may also be a risk factor for the development of chronic bronchitis.[54][55][56]Bronchitis caused in this way is often referred to asindustrial bronchitis,oroccupational bronchitis.[57]Rarely genetic factors also play a role.[58]
Air quality can also affect the respiratory system with higher levels ofnitrogen dioxideandsulfur dioxidecontributing to bronchial symptoms. Sulfur dioxide can cause inflammation which can aggravate chronic bronchitis and make infections more likely.[59]
Air pollution in the workplace is the cause of severalnon-communicable diseases(NCDs) including chronic bronchitis.[60]
Treatment
editDecline in lung function in chronic bronchitis may be slowed bystopping smoking.[61][62]Chronic bronchitis may be treated with a number ofmedicationsand occasionallyoxygen therapy.[1]Pulmonary rehabilitationmay also be used.[1]
A distinction has been made betweenexacerbations(sudden worsenings) of chronic bronchitis, and otherwise stable chronic bronchitis. Stable chronic bronchitis can be defined as the normal definition of chronic bronchitis, plus the absence of an acute exacerbation in the previous four weeks.[45]A Cochrane review found thatmucolyticsin chronic bronchitis may slightly decrease the chance of developing an exacerbation.[63]The mucolyticguaifenesinis a safe and effective treatment for stable chronic bronchitis. This has an advantage in that it is available as an extended use tablet which lasts for twelve hours.[64]Erdosteineis a mucolytic recommended by NICE.[65]GOLD also supports the use of some mucolytics that are advised against when inhaled corticosteroids are being used, and singles out erdosteine as having good effects regardless of corticosteroid use. Erdosteine also has antioxidant properties. Erdosteine has been shown to significantly reduce the risk of exacerbations, shorten their duration, and hospital stays.[66]In those with thechronic bronchitic phenotype of COPD,thephosphodiesterase-4 inhibitorroflumilastmay decrease significant exacerbations.[37]
Epidemiology
editChronic bronchitis affects about 3.4–22% of the general population.[67]Individuals over 45 years of age, smokers, those that live or work in areas with high air pollution, and anybody with asthma all have a higher risk of developing chronic bronchitis.[68]This wide range is due to the different definitions of chronic bronchitis that can be diagnosed based on signs and symptoms or the clinical diagnosis of the disorder. Chronic bronchitis tends to affect men more often than women. While the primary risk factor for chronic bronchitis is smoking, there is still a 4–22% chance that non-smokers can get chronic bronchitis. This might suggest other risk factors such as the inhalation of fuels, dusts, fumes and genetic factor.[40]In the United States, in 2016, 8.6 million people were diagnosed with chronic bronchitis, and there were 518 reported deaths. Per 100,000 of population the death rate of chronic bronchitis was 0.2.[17]
History
editThe condition of bronchitis has been recognised for many centuries, in several different cultures including the Ancient Greek, Chinese, and Indian, with the presence of excess phlegm and cough noted in recognition of the same condition. Early treatments of chronic bronchitis included garlic, cinnamon andipecac,among others.[69]Modern treatments were developed during the second half of the 20th century.[70]
The British physicianCharles Badhamwas the first person to describe the condition and name the acute form asacute bronchitisin his bookObservations on the inflammatory affections of the mucous membrane of the bronchiæ,published in 1808. In this book, Badham distinguished three forms of bronchitis, including acute and chronic. A second, expanded edition of the book was published in 1814 with the titleAn essay on bronchitis.[69]Badham used the term catarrh to refer to the cardinal symptoms of chronic cough andmucus hypersecretionof chronic bronchitis, and described chronic bronchitis as a disabling disorder.[71]
In 1901 an article was published on the treatment of chronic bronchitis in the elderly. The symptoms described have remained unchanged. The cause was thought to be brought on by dampness, cold weather, and foggy conditions, and treatments were aimed towards various cough mixtures, respiratory stimulants, and tonics. It was noted that something other than the weather was thought to be at play.[72]Exacerbations of the condition were also described at this time. Another physicianHarry Campbellwas referred to who had written in theBritish Medical Journala week before. Campbell had suggested that the cause of chronic bronchitis was due to toxic substances, and recommended pure air, simple food, and exercise to remove them from the body.[72]
A joint research programme was undertaken in Chicago and London from 1951 to 1953 in which the clinical features of one thousand cases of chronic bronchitis were detailed. The findings were published in the Lancet in 1953.[73]It was stated that since its introduction by Badham, chronic bronchitis had become an increasingly popular diagnosis. The study had looked at various associations such as the weather, conditions at home, and at work, age of onset, childhood illnesses, smoking habits, and breathlessness. It was concluded that chronic bronchitis invariably led to emphysema, particularly when the bronchitis had persisted for a long time.[73]
In 1957 it was noted that at the time there were many investigations being carried out into chronic bronchitis and emphysema in general, and among industrial workers exposed to dust.[74]Excerpts were published dating from 1864 in which Charles Parsons had noted the occurring consequence of the development of emphysema from bronchitis. This was seen to be not always applicable. His findings were in association with his studies on chronic bronchitis among pottery workers.[74]
A CIBA (nowNovartis) meeting in 1959, and a meeting of theAmerican Thoracic Societyin 1962, defined chronic bronchitis as a component of COPD, in the terms that have not changed.[71][75]
Eosinophilic bronchitis
editEosinophilic bronchitisis a chronic dry cough, defined by the presence of an increased number of a type ofwhite blood cellknown aseosinophils.It has a normal finding on X-ray and has no airflow limitation.[76]
Protracted bacterial bronchitis
editProtracted bacterial bronchitisin children, is defined as a chronic productive cough with a positivebronchoalveolar lavagethat resolves withantibiotics.[77][78]Protracted bacterial bronchitis is usually caused byStreptococcus pneumoniae,non-typableHaemophilus influenzae,orMoraxella catarrhalis.[78]Protracted bacterial bronchitis (lasting more than 4 weeks) in children may be helped by antibiotics.[79]
Plastic bronchitis
editPlastic bronchitisis a rarely found condition in which thickened secretions plug the bronchi.[81][82]The plugs are rubbery or plastic-feeling (thus the name). The light-colored plugs take the branching shape of the bronchi that they fill, and are known asbronchial casts.[81]When these casts are coughed up, they are firmer in texture from typicalphlegmor the short, softer mucus plugs seen in some people with asthma.[81]However, some people with asthma have larger, firmer, and more complex plugs. These differ from the casts seen in people whose plastic bronchitis is associated withcongenital heart diseaseor lymphatic vessel abnormalities mainly becauseeosinophilsandCharcot–Leyden crystalsare present in the asthma-associated casts but not in the others.[81]
Casts obstruct the airflow, and can result in the overinflation of the opposite lung. Plastic bronchitis usually occurs in children. Some cases may result from abnormalities in thelymphatic vessels.Advanced cases may show imaging similarities tobronchiectasis.[82]
Eosinophilic plastic bronchitis
editEosinophilic plastic bronchitis is a subtype of plastic bronchitis that is more often found in children. Symptoms may include a cough, and wheezing, and imaging may reveal a lung that is completely collapsed.[83]Depending on the size of the casts, and the location the condition may present with mild symptoms, or prove fatal.[83]
Aspergillus bronchitis
editAspergillus bronchitisis a type ofaspergillosis,afungal infectioncaused byAspergillusa commonmoldthat affects the bronchi. Unlike other types of pulmonary aspergillosis, it can affect individuals who are notimmunocompromised.[84][85]Inimmunocompetentindividuals, Aspergillus bronchitis may manifest as persistent respiratory infections or symptoms that do not respond to antibiotics, but may improve withantifungals.[86]
References
edit- ^abcdef"Bronchitis".NHLBI.Retrieved9 June2019.
- ^abcdeWenzel, RP; Fowler AA, 3rd (16 November 2006)."Clinical practice. Acute bronchitis".The New England Journal of Medicine.355(20): 2125–30.doi:10.1056/nejmcp061493.PMID17108344.
{{cite journal}}:CS1 maint: numeric names: authors list (link) - ^abVos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, et al. (December 2012)."Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010".Lancet.380(9859): 2163–96.doi:10.1016/S0140-6736(12)61729-2.PMC6350784.PMID23245607.
- ^abcdefghijklmnopKin, S (1 October 2016)."Acute Bronchitis".American Family Physician.94(7): 560–565.PMID27929206.
- ^ab"Antibiotics Aren't Always the Answer".Centers for Disease Control and Prevention.25 September 2017.
- ^abcdefgh"What Is Bronchitis?".August 4, 2011.Archivedfrom the original on 2 April 2015.Retrieved1 April2015.
- ^abcdefTackett, KL; Atkins, A (December 2012)."Evidence-based acute bronchitis therapy".Journal of Pharmacy Practice.25(6): 586–90.doi:10.1177/0897190012460826.PMID23076965.S2CID37651935.
- ^ab"How Is Bronchitis Treated?".August 4, 2011.Archivedfrom the original on 2 April 2015.Retrieved1 April2015.
- ^ab"Bronchitis, Chronic".Medical Subject Headings.National Library of Medicine.MeSHD029481.Retrieved2023-03-16.
- ^abcdGlobal Initiative for Chronic Obstructive Lung Disease - GOLD(PDF).2018. pp. 4–5, 25.Retrieved29 May2019.
- ^Reilly, John J.; Silverman, Edwin K.; Shapiro, Steven D. (2011). "Chronic Obstructive Pulmonary Disease". In Longo, Dan; Fauci, Anthony; Kasper, Dennis; Hauser, Stephen; Jameson, J.; Loscalzo, Joseph (eds.).Harrison's Principles of Internal Medicine(18th ed.). McGraw Hill. pp. 2151–9.ISBN978-0-07-174889-6.
- ^Decramer M, Janssens W, Miravitlles M (April 2012)."Chronic obstructive pulmonary disease".Lancet.379(9823): 1341–51.CiteSeerX10.1.1.1000.1967.doi:10.1016/S0140-6736(11)60968-9.PMC7172377.PMID22314182.
- ^abRabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J (September 2007)."Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary".Am. J. Respir. Crit. Care Med.176(6): 532–55.doi:10.1164/rccm.200703-456SO.hdl:2066/51740.PMID17507545.S2CID20863981.
- ^abcBraman, SS (January 2006)."Chronic cough due to acute bronchitis: ACCP evidence-based clinical practice guidelines".Chest.129(1 Suppl): 95S–103S.doi:10.1378/chest.129.1_suppl.95S.PMC7094612.PMID16428698.
- ^abFleming, DM; Elliot, AJ (March 2007)."The management of acute bronchitis in children".Expert Opinion on Pharmacotherapy.8(4): 415–26.doi:10.1517/14656566.8.4.415.PMID17309336.S2CID46247982.
- ^"Bronchitis".WebMD.Retrieved13 January2024.
- ^ab"FastStats".Centers for Disease Control and Prevention.23 May 2019.Retrieved30 May2019.
- ^Villarroel, MA; Blackwell, DL; Jen, A (2019),"Summary Health Statistics: National Health Interview Survey, 2018"(PDF),ftp.cdc.gov,retrieved22 March2020
- ^abSmith, Susan M.; Fahey, Tom; Smucny, John; Becker, Lorne A. (2017)."Antibiotics for acute bronchitis".The Cochrane Database of Systematic Reviews.2017(6): CD000245.doi:10.1002/14651858.CD000245.pub4.hdl:10779/rcsi.10778735.v1.ISSN1469-493X.PMC6481481.PMID28626858.
- ^abcSethi, Sanjay (May 2023)."Acute Bronchitis".Merck Manuals Professional Edition.
- ^ab"How Can Bronchitis Be Prevented?".NIH. August 4, 2011. Archived fromthe originalon 2 April 2015.
- ^Smith, SM; Schroeder, K; Fahey, T (24 November 2014)."Over-the-counter (OTC) medications for acute cough in children and adults in community settings".The Cochrane Database of Systematic Reviews.2014(11): CD001831.doi:10.1002/14651858.CD001831.pub5.PMC7061814.PMID25420096.
- ^Becker, Lorne A.; Hom, Jeffrey; Villasis-Keever, Miguel; van der Wouden, Johannes C. (2015-09-03)."Beta2-agonists for acute cough or a clinical diagnosis of acute bronchitis".The Cochrane Database of Systematic Reviews.2015(9): CD001726.doi:10.1002/14651858.CD001726.pub5.ISSN1469-493X.PMC7078572.PMID26333656.
- ^"Acute Bronchitis | Bronchitis Symptoms | MedlinePlus".Retrieved2017-11-30.
- ^Jiang, Lanhui; Li, Ka; Wu, Taixiang (15 February 2012)."Chinese medicinal herbs for acute bronchitis".Cochrane Database of Systematic Reviews.2012(2): CD004560.doi:10.1002/14651858.CD004560.pub4.PMC7202254.PMID22336804.
- ^ab"ICD-11 - ICD-11 for Mortality and Morbidity Statistics".icd.who.int.Retrieved15 August2021.
- ^"Chronic Obstructive Pulmonary Disease (COPD) - Pulmonary Disorders".MSD Manual Professional Edition.Retrieved3 June2019.
Chronic bronchitis becomes chronic obstructive bronchitis if spirometric evidence of airflow obstruction develops.
- ^Widysanto, A; Mathew, G (January 2019)."Chronic Bronchitis".StatPearls [Internet].PMID29494044.NBK482437.
Chronic bronchitis... is very often secondary to chronic obstructive pulmonary disease (COPD).
- ^Lee, Sang-Do (2017).COPD: Heterogeneity and Personalized Treatment.Springer. p. 150.ISBN9783662471784.
- ^Maselli, DJ (May 2019)."Clinical Epidemiology of COPD: Insights From 10 Years of the COPDGene Study".Chest.156(2): 228–238.doi:10.1016/j.chest.2019.04.135.PMC7198872.PMID31154041.
- ^Dotan, Y; So, JY; Kim, V (9 April 2019)."Chronic Bronchitis: Where Are We Now?".Chronic Obstructive Pulmonary Diseases.6(2): 178–192.doi:10.15326/jcopdf.6.2.2018.0151.PMC6596437.PMID31063274.
with CB by symptoms (18.9%), approximately 60% had COPD (i.e., had also airflow obstruction on spirometry)
- ^"Chronic obstructive pulmonary disease (COPD)".who.int.Retrieved15 July2019.
The more familiar terms "chronic bronchitis" and "emphysema" have often been used as labels for the condition.
- ^"COPD: Definition".WHO.Retrieved15 July2019.
The more familiar terms 'chronic bronchitis' and 'emphysema' are no longer used, but are now included within the COPD diagnosis.
- ^abFerri, Fred (2019).Ferri's Clinical Advisor.Elsevier. p. 331.ISBN9780323530422.
- ^abcdShen, Y (30 January 2018)."Management of airway mucus hypersecretion in chronic airway inflammatory disease: Chinese expert consensus (English edition)".International Journal of Chronic Obstructive Pulmonary Disease.13:399–407.doi:10.2147/COPD.S144312.PMC5796802.PMID29430174.
- ^abVoynow, J (Feb 2009). "Mucins, mucus, and sputum".Chest.135(2): 505–512.doi:10.1378/chest.08-0412.PMID19201713.
- ^abVestbo, J.; Hurd, S. S.; Agustí, A. G.; Jones, P. W.; Vogelmeier, C.; Anzueto, A.; Barnes, P. J.; Fabbri, L. M.; Martinez, F. J.; Nishimura, M.; Stockley, R. A.; Sin, D. D.; Rodriguez-Roisin, R. (2013)."Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary".American Journal of Respiratory and Critical Care Medicine.187(4): 347–65.doi:10.1164/rccm.201204-0596PP.PMID22878278.
- ^Weinberger, Steven (2019).Principles of Pulmonary Medicine.Elsevier. p. 98.ISBN9780323523714.
- ^"New Insights on Chronic Bronchitis:Diagnostic Test and Better Treatments on the Horizon".nhlbi.nih.gov.September 2017.Retrieved3 August2019.
- ^abcKim, V; Criner, G (Feb 2013)."Chronic bronchitis and chronic obstructive pulmonary disease".Am J Respir Crit Care Med.187(3): 228–237.doi:10.1164/rccm.201210-1843CI.PMC4951627.PMID23204254.
- ^Global Strategy for Prevention, Diagnosis and Management of COPD: 2021 Report(PDF).Global Initiative for Chronic Obstructive Lung Disease. 25 November 2020. p. 106.Retrieved3 August2021.
- ^Cohen, Jonathan; Powderly, William (2004).Infectious Diseases, 2nd ed.Mosby (Elsevier). Chapter 33: Bronchitis, Bronchiectasis, and Cystic Fibrosis.ISBN978-0323025737.
- ^Foster, W (2002). "Mucociliary transport and cough in humans".Pulm Pharmacol Ther.15(3): 277–282.doi:10.1006/pupt.2002.0351.PMID12099778.
- ^Ghosh, A (October 2015)."Airway hydration and COPD".Cell Mol Life Sci.72(19): 3637–52.doi:10.1007/s00018-015-1946-7.PMC4567929.PMID26068443.
- ^abOhar, JA; Donohue, JF; Spangenthal, S (23 October 2019)."The Role of Guaifenesin in the Management of Chronic Mucus Hypersecretion Associated with Stable Chronic Bronchitis: A Comprehensive Review".Chronic Obstructive Pulmonary Diseases.6(4): 341–349.doi:10.15326/jcopdf.6.4.2019.0139.PMC7006698.PMID31647856.
- ^"ICD-11 - Mortality and Morbidity Statistics".icd.who.int.
- ^"ICD-11 - Mortality and Morbidity Statistics".icd.who.int.
- ^"Understanding Chronic Bronchitis".American Lung Association. 2012. Archived fromthe originalon 18 December 2012.Retrieved30 December2012.
- ^Forey, BA; Thornton, AJ; Lee, PN (June 2011)."Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema".BMC Pulmonary Medicine.11(36): 36.doi:10.1186/1471-2466-11-36.PMC3128042.PMID21672193.
- ^Global Initiative for Chronic Obstructive Lung Disease(PDF).2019. p. 13.Retrieved25 May2019.
- ^Ribeiro, L (October 2016)."Effect of cannabis smoking on lung function and respiratory symptoms: a structured literature review".npj Primary Care Respiratory Medicine.26:16071.doi:10.1038/npjpcrm.2016.71.PMC5072387.PMID27763599.
- ^Pfeifer, A (May 2006). "Pulmonary consequences of marijuana smoking".Ugeskr Laeger.168(18): 1743–6.PMID16729923.
- ^Szczyrek, M; Krawczyk, P; Milanowski, J; Jastrzebska, I; Zwolak, A; Daniluk, J (2011). "Chronic obstructive pulmonary disease in farmers and agricultural workers-an overview".Annals of Agricultural and Environmental Medicine.18(2): 310–313.PMID22216804.
- ^Fischer, BM; Pavlisko, E; Voynow, JA (2011)."Pathogenic triad in COPD: oxidative stress, protease-antiprotease imbalance, and inflammation".International Journal of Chronic Obstructive Pulmonary Disease.6:413–421.doi:10.2147/COPD.S10770.PMC3157944.PMID21857781.
- ^National Heart Lung and Blood Institute (2009)."Who Is at Risk for Bronchitis?".National Institutes of Health. Archived fromthe originalon 4 January 2013.Retrieved30 December2012.
- ^National Institute of Occupational Safety and Health (2012)."Respiratory Diseases Input: Occupational Risks".NIOSH Program Portfolio.Centers for Disease Control and Prevention.Archivedfrom the original on 20 December 2012.Retrieved30 December2012.
- ^"Industrial bronchitis: MedlinePlus Medical Encyclopedia".medlineplus.gov.Retrieved28 May2019.
- ^"What Causes COPD".American Lung Association.Retrieved24 February2019.
- ^"Ambient (outdoor) air quality and health".who.int.2 May 2018.Retrieved11 July2019.
- ^"Protecting workers' health".who.int.November 2017.Retrieved12 July2019.
- ^Fauci, Anthony S.; Daniel L. Kasper; Dan L. Longo; Eugene Braunwald; Stephen L. Hauser; J. Larry Jameson (2008).Chapter 254. Chronic Obstructive Pulmonary DiseaseHarrison's Principles of Internal Medicine(17th ed.). New York: McGraw-Hill.ISBN978-0-07-147691-1.
- ^Willemse, BW; Postma, DS; Timens, W; ten Hacken, NH (March 2004)."The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation".The European Respiratory Journal.23(3): 464–476.doi:10.1183/09031936.04.00012704.PMID15065840.
- ^Poole, Phillippa; Sathananthan, K; Fortescue, R (May 2019)."Mucolytic agents versus placebo for chronic bronchitis or chronic obstructive pulmonary disease".The Cochrane Database of Systematic Reviews.5(7): CD001287.doi:10.1002/14651858.CD001287.pub6.PMC6527426.PMID31107966.
- ^Albrecht, H. H.; Dicpinigaitis, P. V.; Guenin, E. P. (2017)."Role of guaifenesin in the management of chronic bronchitis and upper respiratory tract infections".Multidisciplinary Respiratory Medicine.12:31.doi:10.1186/s40248-017-0113-4.PMC5724298.PMID29238574.
- ^"Erdosteine".NICE.Retrieved20 July2021.
- ^Meldrum OW, Chotirmall SH (June 2021)."Mucus, Microbiomes and Pulmonary Disease".Biomedicines.9(6): 675.doi:10.3390/biomedicines9060675.PMC8232003.PMID34199312.
- ^Kim, Victor; Criner, Gerard J. (2015)."The chronic bronchitis phenotype in chronic obstructive pulmonary disease".Current Opinion in Pulmonary Medicine.21(2). Ovid Technologies (Wolters Kluwer Health): 133–141.doi:10.1097/mcp.0000000000000145.ISSN1070-5287.PMC4373868.PMID25575367.
- ^Kochanek, Kenneth (June 2016)."Deaths: Final Data for 2014"(PDF).National Vital Statistics Reports.65(4): 1–122.PMID27378572.
- ^abZiment I (1991). "History of the treatment of chronic bronchitis".Respiration; International Review of Thoracic Diseases.58(Suppl 1): 37–42.doi:10.1159/000195969.PMID1925077.
- ^Fishman AP (May 2005). "One hundred years of chronic obstructive pulmonary disease".American Journal of Respiratory and Critical Care Medicine.171(9): 941–8.doi:10.1164/rccm.200412-1685OE.PMID15849329.
- ^abPetty, TL (2006)."The history of COPD".International Journal of Chronic Obstructive Pulmonary Disease.1(1): 3–14.doi:10.2147/copd.2006.1.1.3.PMC2706597.PMID18046898.
- ^ab"Chronic Bronchitis".The Hospital.31(786): 48–49. 19 October 1901.PMC5211570.PMID29819251.
- ^abOswald, NC; Harold, JT; Martin, WJ (26 September 1953). "Clinical pattern of chronic bronchitis".Lancet.265(6787): 639–43.doi:10.1016/s0140-6736(53)90369-9.PMID13098028.
- ^abMeiklejohn, A (July 1957)."A house-surgeon's observations on bronchitis in North Staffordshire pottery workers in 1864".British Journal of Industrial Medicine.14(3): 211–2.doi:10.1136/oem.14.3.211.PMC1037807.PMID13446354.
- ^"Terminology, Definitions, and Classification of Chronic Pulmonary Emphysema and Related Conditions: A Report of the Conclusions of a Ciba Guest Symposium".Thorax.14(4): 286–299. December 1959.doi:10.1136/thx.14.4.286.PMC1018516.
- ^Longo, Dan (2012).Harrison's Principles of Internal Medicine.McGraw Hill. p. 284.ISBN9780071748896.
- ^Goldsobel, AB; Chipps, BE (March 2010). "Cough in the pediatric population".The Journal of Pediatrics.156(3): 352–358.e1.doi:10.1016/j.jpeds.2009.12.004.PMID20176183.
- ^abCraven, V; Everard, ML (January 2013). "Protracted bacterial bronchitis: reinventing an old disease".Archives of Disease in Childhood.98(1): 72–76.doi:10.1136/archdischild-2012-302760.PMID23175647.S2CID34977990.
- ^Marchant, JM; Petsky, HL; Morris, PS; Chang, AB (31 July 2018)."Antibiotics for prolonged wet cough in children".The Cochrane Database of Systematic Reviews.2018(7): CD004822.doi:10.1002/14651858.CD004822.pub3.PMC6513288.PMID30062732.
- ^Kamaltynova, E. M.; Krivoshchekov, E. V.; Yanulevich, O. S.; Kavardakova, E. S. (2017-08-11)."Plastic bronchitis associated with corrected cardiac anomaly in a child".Bulletin of Siberian Medicine.16(2): 180–186.doi:10.20538/1682-0363-2017-2-180-186.ISSN1819-3684.
- ^abcdKotloff, Robert; McCormack, Francis X. (2016-08-16).Rare and Orphan Lung Diseases, An Issue of Clinics in Chest Medicine, E-Book.Elsevier Health Sciences. pp. 405–408.ISBN978-0-323-46274-7.
- ^abPanchabhai, TS; Mukhopadhyay, S; Sehgal, S; Bandyopadhyay, D; Erzurum, SC; Mehta, AC (November 2016)."Plugs of the Air Passages: A Clinicopathologic Review".Chest.150(5): 1141–1157.doi:10.1016/j.chest.2016.07.003.PMC6026239.PMID27445091.
- ^abGipsman, AI; Feld, L; Johnson, B (November 2023). "Eosinophilic plastic bronchitis: Case series and review of the literature".Pediatric pulmonology.58(11): 3023–3031.doi:10.1002/ppul.26650.PMID37606213.
- ^"Aspergillus bronchitis | Aspergillus & Aspergillosis Website".aspergillus.org.uk.
- ^Kosmidis, Chris; Denning, David W. (1 March 2015)."The clinical spectrum of pulmonary aspergillosis".Thorax.70(3): 270–277.doi:10.1136/thoraxjnl-2014-206291.PMID25354514.Retrieved8 November2019.
- ^Chrdle, Ales; Mustakim, Sahlawati; Bright-Thomas, Rowland J.; Baxter, Caroline G.; Felton, Timothy; Denning, David W. (December 2012). "Aspergillus bronchitis without significant immunocompromise".Annals of the New York Academy of Sciences.1272(1): 73–85.Bibcode:2012NYASA1272...73C.doi:10.1111/j.1749-6632.2012.06816.x.PMID23231717.
External links
edit- NIHentry onBronchitis
- MedlinePlusentries onAcute bronchitisandChronic bronchitis
- Mayo Clinicfactsheet on bronchitis