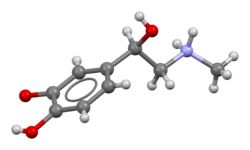
Adrenaline,also known asepinephrine,is ahormoneandmedication[10][11]which is involved in regulating visceral functions (e.g., respiration).[10][12]It appears as a white microcrystalline granule.[13]Adrenaline is normally produced by theadrenal glandsand by a small number ofneuronsin themedulla oblongata.[14]It plays an essential role in thefight-or-flight responseby increasing blood flow to muscles,heart outputby acting on theSA node,[15]pupil dilation response,andblood sugar level.[16][17]It does this by binding toAlphaandbeta receptors.[17]It is found in many animals, including humans, and somesingle-celled organisms.[18][19]It has also been isolated from the plantScoparia dulcisfound in Northern Vietnam.[20]
Medical uses
editAs a medication, it is used to treat several conditions, includingallergic reactionanaphylaxis,cardiac arrest,and superficial bleeding.[8]Inhaledadrenaline may be used to improve the symptoms ofcroup.[21]It may also be used forasthmawhen other treatments are not effective. It is givenintravenously,byinjection into a muscle,by inhalation, or byinjection just under the skin.[8]Common side effects include shakiness,anxiety,and sweating. A fast heart rate and high blood pressure may occur. Occasionally it may result in anabnormal heart rhythm.While the safety of its use duringpregnancyandbreastfeedingis unclear, the benefits to the mother must be taken into account.[8]
A case has been made for the use of adrenaline infusion in place of the widely accepted treatment ofinotropesfor preterm infants with clinical cardiovascular compromise. Although sufficient data strongly recommends adrenaline infusions as a viable treatment, more trials are needed to conclusively determine that these infusions will successfully reducemorbidityandmortalityrates among preterm, cardiovascularly compromised infants.[22]
Epinephrine can also be used to treat open-angle glaucoma, as it has been found to increase the outflow of aqueous humor in the eye. This lowers the intraocular pressure in the eye and thus aids in treatment.[23]
Physiological effects
editTheadrenal medullais a major contributor to total circulatingcatecholamines(L-DOPAis at a higher concentration in theplasma),[24]though it contributes over 90% of circulating adrenaline. Little adrenaline is found in other tissues, mostly in scatteredchromaffin cellsand in a small number ofneuronsthat use adrenaline as aneurotransmitter.[25]Followingadrenalectomy,adrenaline disappears below the detection limit in the bloodstream.[26]
Pharmacological doses of adrenaline stimulateα1,α2,β1,β2,andβ3adrenoceptors of thesympathetic nervous system.Sympathetic nerve receptors are classified as adrenergic, based on their responsiveness to adrenaline.[27]The term "adrenergic" is often misinterpreted in that the main sympathetic neurotransmitter isnoradrenaline,rather than adrenaline, as discovered byUlf von Eulerin 1946.[28][29]Adrenaline has a β2adrenoceptor-mediated effect onmetabolismand theairway,with no direct neural connection from thesympathetic gangliato theairway.[30][31][32]
Walter Bradford Cannonoriginally proposed the concept of the adrenal medulla and thesympathetic nervous systembeing involved in the flight, fight, and fright response.[33]But the adrenal medulla, in contrast to the adrenal cortex, is not required for survival. In adrenalectomized patients, hemodynamic and metabolic responses to stimuli such as hypoglycemia and exercise remain normal.[34][35]
Exercise
editOne physiological stimulus to adrenaline secretion is exercise. This was first demonstrated by measuring the dilation of a (denervated) pupil of a cat on a treadmill,[36]later confirmed using a biological assay of urine samples.[37]Biochemical methods for measuring catecholamines in plasma were published from 1950 onwards.[38]Although much valuable work has been published using fluorimetric assays to measure total catecholamine concentrations, the method is too non-specific and insensitive to accurately determine the very small quantities of adrenaline in plasma. The development of extraction methods and enzyme–isotope derivate radio-enzymatic assays (REA) transformed the analysis down to a sensitivity of 1 pg for adrenaline.[39]Early REA plasma assays indicated that adrenaline and total catecholamines rise late in exercise, mostly when anaerobic metabolism commences.[40][41][42]
During exercise, the adrenaline blood concentration rises partially from the increased secretion of the adrenal medulla and partly from the decreased metabolism of adrenaline due to reduced blood flow to the liver.[43]Infusion of adrenaline to reproduce exercise circulating concentrations of adrenaline in subjects at rest has little hemodynamic effect other than a slight β2-mediated fall in diastolic blood pressure.[44][45]Infusion of adrenaline well within the physiological range suppresses human airway hyper-reactivity sufficiently to antagonize the constrictor effects of inhaled histamine.[46]
A link between the sympathetic nervous system and the lungs was shown in 1887 when Grossman showed that stimulation of cardiac accelerator nerves reversed muscarine-induced airway constriction.[47]In experiments in the dog, where the sympathetic chain was cut at the level of the diaphragm, Jackson showed that there was no direct sympathetic innervation to the lung, but bronchoconstriction was reversed by the release of adrenaline from the adrenal medulla.[48]An increased incidence of asthma has not been reported for adrenalectomized patients; those with a predisposition to asthma will have some protection from airway hyper-reactivity from their corticosteroid replacement therapy. Exercise induces progressive airway dilation in normal subjects that correlates with workload and is not prevented by beta-blockade.[49]The progressive airway dilation with increasing exercise is mediated by a progressive reduction in resting vagal tone. Beta blockade with propranolol causes a rebound in airway resistance after exercise in normal subjects over the same time course as the bronchoconstriction seen with exercise-induced asthma.[50]The reduction in airway resistance during exercise reduces the work of breathing.[51]
Emotional responses
editEvery emotional response has a behavioral, an autonomic, and a hormonal component. The hormonal component includes the release of adrenaline, an adrenomedullary response to stress controlled by thesympathetic nervous system.The major emotion studied in relation to adrenaline is fear. In an experiment, subjects who were injected with adrenaline expressed more negative and fewer positive facial expressions to fear films compared to a control group. These subjects also reported a more intense fear from the films and greater mean intensity of negative memories than control subjects.[52]The findings from this study demonstrate that there are learned associations between negative feelings and levels of adrenaline. Overall, the greater amount of adrenaline is positively correlated with an aroused state ofnegative emotions.These findings can be an effect in part that adrenaline elicits physiological sympathetic responses, including an increased heart rate and knee shaking, which can be attributed to the feeling of fear regardless of the actual level of fear elicited from the video. Although studies have found a definite relation between adrenaline and fear, other emotions have not had such results. In the same study, subjects did not express a greater amusement to an amusement film nor greater anger to an anger film.[52]Similar findings were also supported in a study that involved rodent subjects that either were able or unable to produce adrenaline. Findings support the idea that adrenaline has a role in facilitating the encoding of emotionally arousing events, contributing to higher levels of arousal due to fear.[53]
Memory
editIt has been found that adrenergic hormones, such as adrenaline, can produce retrograde enhancement oflong-term memoryin humans. The release of adrenaline due to emotionally stressful events, which is endogenous adrenaline, can modulate memory consolidation of the events, ensuring memory strength that is proportional to memory importance. Post-learning adrenaline activity also interacts with the degree of arousal associated with the initial coding.[54]There is evidence that suggests adrenaline does have a role in long-term stress adaptation and emotional memory encoding specifically. Adrenaline may also play a role in elevating arousal and fear memory under particular pathological conditions, includingpost-traumatic stress disorder.[53]Overall, "Extensive evidence indicates that epinephrine (EPI) modulates memory consolidation for emotionally arousing tasks in animals and human subjects."[55]Studies have also found that recognition memory involving adrenaline depends on a mechanism that depends on β adrenoceptors.[55]Adrenaline does not readily cross the blood-brain barrier, so its effects on memory consolidation are at least partly initiated by β adrenoceptors in the periphery. Studies have found thatsotalol,aβ adrenoceptor antagonistthat also does not readily enter the brain, blocks the enhancing effects of peripherally administered adrenaline on memory.[56]These findings suggest that β adrenoceptors are necessary for adrenaline to have an impact on memory consolidation.[57][58]
Pathology
editIncreased adrenaline secretion is observed inpheochromocytoma,hypoglycemia,myocardial infarction,and to a lesser degree, inessential tremor(also known as benign, familial, or idiopathic tremor). A general increase in sympathetic neural activity is usually accompanied by increased adrenaline secretion, but there is selectivity during hypoxia and hypoglycemia, when the ratio of adrenaline to noradrenaline is considerably increased.[59][60][61]Therefore, there must be some autonomy of the adrenal medulla from the rest of the sympathetic system.
Myocardial infarction is associated with high levels of circulating adrenaline and noradrenaline, particularly in cardiogenic shock.[62][63]
Benign familial tremor (essential tremor) (BFT) is responsive to peripheral β adrenergic blockers, and β2-stimulation is known to cause tremor. Patients with BFT were found to have increased plasma adrenaline but not noradrenaline.[64][65]
Low or absent concentrations of adrenaline can be seen in autonomic neuropathy or following adrenalectomy. Failure of the adrenal cortex, as withAddison's disease,can suppress adrenaline secretion as the activity of the synthesizing enzyme,phenylethanolamine-N-methyltransferase,depends on the high concentration of cortisol that drains from the cortex to the medulla.[66][67][68]
Terminology
editIn 1901,Jōkichi Takaminepatented a purified extract from theadrenal glands,which wastrademarkedbyParke, Davis & Coin the US.[69]TheBritish Approved NameandEuropean Pharmacopoeiaterm for this drug is henceadrenaline(fromLatinad,"on", andrēnālis,"of the kidney", fromren,"kidney" ).[70]
However, the pharmacologistJohn Abelhad already prepared an extract from adrenal glands as early as 1897, and he coined the nameepinephrineto describe it (fromAncient Greekἐπῐ́(epí), "upon", andνεφρός(nephrós), "kidney" ).[69]As the termAdrenalinewas a registered trademark in the US,[69]and in the belief that Abel's extract was the same as Takamine's (a belief since disputed), epinephrine instead became[when?]the generic name used in the US[69]and remains thepharmaceutical'sUnited States Adopted NameandInternational Nonproprietary Name(though the name adrenaline is frequently used[71]).
The terminology is now one of the few differences between the INN and BAN systems of names.[72]Although European health professionals and scientists preferentially use the termadrenaline,the converse is true among American health professionals and scientists. Nevertheless, even among the latter, receptors for this substance are calledadrenergic receptorsoradrenoceptors,and pharmaceuticals that mimic its effects are often calledadrenergics.The history of adrenaline and epinephrine is reviewed by Rao.[73]
Mechanism of action
edit| Organ | Effects |
|---|---|
| Heart | Increases heart rate; contractility; conduction across AV node |
| Lungs | Increases respiratory rate; bronchodilation |
| Liver | Stimulatesglycogenolysis |
| Muscle | Stimulates glycogenolysis andglycolysis |
| Brain | Increased cerebral tissue oxygenation |
| Systemic | Vasoconstrictionandvasodilation |
| Triggerslipolysis | |
| Muscle contraction |
As a hormone, adrenaline acts on nearly all body tissues by binding toadrenergic receptors.Its effects on various tissues depend on the type of tissue and expression of specific forms ofadrenergic receptors.For example, high levels of adrenaline causesmooth musclerelaxation in the airways but causes contraction of the smooth muscle that lines mostarterioles.
Adrenaline is a nonselectiveagonistof all adrenergic receptors, including the major subtypesα1,α2,β1,β2,andβ3.[74]Adrenaline's binding to these receptors triggers a number of metabolic changes. Binding to α-adrenergic receptors inhibitsinsulinsecretion by thepancreas,stimulatesglycogenolysisin theliverandmuscle,[75]and stimulatesglycolysisand inhibits insulin-mediatedglycogenesisin muscle.[76][77]β adrenergic receptor binding triggersglucagonsecretion in the pancreas, increasedadrenocorticotropic hormone(ACTH) secretion by thepituitary gland,and increasedlipolysisbyadipose tissue.Together, these effects increaseblood glucoseandfatty acids,providing substrates for energy production within cells throughout the body.[77]Binding of β adrenergic receptor also increases the production of cyclic AMP.[78]
Adrenaline causesliver cellsto releaseglucoseinto the blood, acting through both Alpha and beta-adrenergic receptors to stimulate glycogenolysis. Adrenaline binds to β2receptors on liver cells, which changes conformation and helps Gs,aheterotrimeric G protein,exchange GDP to GTP. This trimeric G protein dissociates toGsAlphaand Gsbeta/gamma subunits. GsAlpha stimulatesadenylyl cyclase,thus convertingadenosine triphosphateintocyclic adenosine monophosphate(AMP). Cyclic AMP activatesprotein kinase A.Protein kinase A phosphorylates and partially activatesphosphorylase kinase.Adrenaline also binds to α1adrenergic receptors, causing an increase ininositol trisphosphate,inducing calcium ions to enter the cytoplasm. Calcium ions bind tocalmodulin,which leads to further activation of phosphorylase kinase. Phosphorylase kinase phosphorylatesglycogen phosphorylase,which then breaks downglycogenleading to the production of glucose.[79]
Adrenaline also has significant effects on the cardiovascular system. It increases peripheral resistance viaα1receptor-dependentvasoconstrictionand increasescardiac outputby binding to β1receptors. The goal of reducing peripheral circulation is to increase coronary and cerebral perfusion pressures and therefore increase oxygen exchange at the cellular level.[80][81]While adrenaline does increase aortic, cerebral, and carotid circulation pressure, it lowers carotid blood flow andend-tidal CO2or ETCO2levels. It appears that adrenaline improves microcirculation at the expense of the capillary beds where perfusion takes place.[82]
Measurement in biological fluids
editAdrenaline may be quantified in blood, plasma, or serum as a diagnostic aid, to monitor therapeutic administration, or to identify the causative agent in a potential poisoning victim. Endogenous plasma adrenaline concentrations in resting adults usually are less than 10 ng/L, but they may increase by 10-fold during exercise and by 50-fold or more during times of stress.Pheochromocytomapatients often have plasma adrenaline levels of 1000–10,000 ng/L. Parenteral administration of adrenaline to acute-care cardiac patients can produce plasma concentrations of 10,000 to 100,000 ng/L.[83][84]
Biosynthesis
editIn chemical terms, adrenaline is one of a group ofmonoaminescalled thecatecholamines.Adrenaline is synthesized in thechromaffin cellsof theadrenal gland'sadrenal medullaand a small number of neurons in themedulla oblongatain the brain through ametabolic pathwaythat converts theamino acidsphenylalanineandtyrosineinto a series of metabolic intermediates and, ultimately, adrenaline.[10][12][85]Tyrosine is first oxidized toL-DOPAbytyrosine hydroxylase;this is the rate-limiting step. Then it is subsequently decarboxylated to givedopamineby DOPA decarboxylase (aromaticL-amino acid decarboxylase). Dopamine is then converted tonoradrenalinebydopamine beta-hydroxylase,which utilizes ascorbic acid (vitamin C) and copper. The final step in adrenaline biosynthesis is themethylationof theprimary amineof noradrenaline. This reaction is catalyzed by the enzymephenylethanolamineN-methyltransferase(PNMT), which utilizesS-adenosyl methionine(SAMe) as themethyldonor.[86]While PNMT is found primarily in thecytosolof theendocrinecells of theadrenal medulla(also known aschromaffin cells), it has been detected at low levels in both theheartandbrain.[87]
Epinephrine is produced in a small group of neurons in the human brain (specifically, in themedulla oblongata) via the metabolic pathway shown above.[12] |
Regulation
editThe major physiologic triggers of adrenaline release center uponstresses,such as physical threat, excitement, noise, bright lights, and high or low ambient temperature. All of these stimuli are processed in thecentral nervous system.[91]
Adrenocorticotropic hormone(ACTH) and thesympathetic nervous systemstimulate the synthesis of adrenaline precursors by enhancing the activity oftyrosine hydroxylaseanddopamine β-hydroxylase,two key enzymes involved in catecholamine synthesis.[citation needed]ACTH also stimulates theadrenal cortexto releasecortisol,which increases the expression of PNMT in chromaffin cells, enhancing adrenaline synthesis. This is most often done in response to stress.[citation needed]The sympathetic nervous system, acting viasplanchnic nervesto the adrenal medulla, stimulates the release of adrenaline.Acetylcholinereleased by preganglionic sympathetic fibers of these nerves acts onnicotinic acetylcholine receptors,causing cell depolarization and an influx ofcalciumthroughvoltage-gated calcium channels.Calcium triggers theexocytosisof chromaffin granules and, thus, the release of adrenaline (and noradrenaline) into the bloodstream.[citation needed]For noradrenaline to be acted upon by PNMT in the cytosol, it must first be shipped out ofgranulesof the chromaffin cells. This may occur via the catecholamine-H+exchangerVMAT1.VMAT1 is also responsible for transporting newly synthesized adrenaline from the cytosol back into chromaffin granules in preparation for release.[92]
Unlike many other hormones, adrenaline (as with other catecholamines) does not exertnegative feedbacktodown-regulateits own synthesis. Abnormal adrenaline levels can occur in various conditions, such as surreptitious adrenaline administration,pheochromocytoma,and other tumors of thesympathetic ganglia.
Its action is terminated with reuptake into nerve terminal endings, some minute dilution, and metabolism bymonoamine oxidase[93]andcatechol-O-methyl transferaseinto3,4-Dihydroxymandelic acidandMetanephrine.
History
editExtracts of theadrenal glandwere first obtained by Polish physiologistNapoleon Cybulskiin 1895.[94]These extracts, which he callednadnerczyna( "adrenalin" ), contained adrenaline and other catecholamines.[95]American ophthalmologistWilliam H. Batesdiscovered adrenaline's usage for eye surgeries prior to 20 April 1896.[96]In 1897,John Jacob Abel(1857–1938), the father of modern pharmacology, found a natural substance produced by the adrenal glands that he named epinephrine. The first hormone to be identified, it remains a crucial, first-line treatment for cardiac arrests, severe allergic reactions, and other conditions. In 1901, Jokichi Takamine successfully isolated and purified the hormone from the adrenal glands of sheep and oxen.[97]Adrenaline was first synthesized in the laboratory byFriedrich StolzandHenry Drysdale Dakin,independently, in 1904.[98]
Although secretin is mentioned as the first hormone, adrenaline is the first hormone since the discovery of the activity of adrenal extract on blood pressure was observed in 1895 before that ofsecretinin 1902.[73]In 1895, George Oliver (1841–1915), a general practitioner in North Yorkshire, and Edward Albert Schäfer (1850–1935), a physiologist at University College of London published a paper about the active component ofadrenal glandextract causing the increase in blood pressure and heart rate was from the medulla, but not the cortex of the adrenal gland.[99]In 1897,John Jacob Abel(1857–1938) ofJohns Hopkins University,the first chairman of the first US department of pharmacology, found a compound called epinephrine with the molecular formula of C17H15NO4.[73]Abel claimed his principle from adrenal gland extract was active.
In 1900, Jōkichi Takamine (1854–1922), a Japanese chemist, worked with his assistant,Keizo Uenaka(1876–1960), to purify a 2000 times more active principle than epinephrine from the adrenal gland, named adrenaline with the molecular formula C10H15NO3.[73][99]Additionally, in 1900 Thomas Aldrich of Parke-Davis Scientific Laboratory also purified adrenaline independently. Takamine and Parke-Davis later in 1901 both got the patent for adrenaline. The fight for terminology between adrenaline and epinephrine was not ended until the first adrenaline structural discovery by Hermann Pauly (1870–1950) in 1903 and the first adrenaline synthesis byFriedrich Stolz(1860–1936), a German chemist in 1904. They both believed that Takamine's compound was the active principle while Abel's compound was the inactive one.[citation needed]Stolz synthesized adrenaline from its ketone form (adrenalone).[100]
Society and culture
editAdrenaline junkie
editAnadrenaline junkieis someone who engages in sensation-seeking behavior through "the pursuit of novel and intense experiences without regard for physical, social, legal or financial risk".[101]Such activities include extreme and risky sports, substance abuse, unsafe sex, and crime. The term relates to the increase in circulating levels of adrenaline during physiologicalstress.[102]Such an increase in the circulating concentration of adrenaline is secondary to the activation of the sympathetic nerves innervating the adrenal medulla, as it is rapid and not present in animals where the adrenal gland has been removed.[103]Although such stress triggers adrenaline release, it also activates many other responses within the central nervous systemreward system,which drives behavioral responses; while the circulating adrenaline concentration is present, it may not drive behavior. Nevertheless, adrenaline infusion alone does increase alertness[104]and has roles in the brain, including the augmentation of memory consolidation.[102]
Strength
editAdrenaline has been implicated in feats of great strength, often occurring in times of crisis. For example, there are stories of a parent lifting part of a car when their child is trapped underneath, showcasing the insane amount of potential the body can endure under stress and highlighting the profound effects of adrenaline in unlocking extraordinary physical abilities.[105][106]
See also
editReferences
edit- ^Andersen AM (1975)."Structural Studies of Metabolic Products of Dopamine. III. Crystal and Molecular Structure of (−)-Adrenaline".Acta Chem. Scand.29b(2): 239–244.doi:10.3891/acta.chem.scand.29b-0239.PMID1136652.
- ^"Neffy- epinephrine spray".DailyMed.20 August 2024.Retrieved5 September2024.
- ^"European Medicines Agency".Eurneffy EPAR.27 June 2024.Archivedfrom the original on 29 June 2024.Retrieved29 June2024.Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^"Eurneffy Product information".Union Register of medicinal products.23 August 2024.Retrieved27 August2024.
- ^El-Bahr SM, Kahlbacher H, Patzl M, Palme RG (May 2006). "Binding and clearance of radioactive adrenaline and noradrenaline in sheep blood".Veterinary Research Communications.30(4). Springer Science and Business Media LLC: 423–32.doi:10.1007/s11259-006-3244-1.PMID16502110.S2CID9054777.
- ^Franksson G, Anggård E (March 2009). "The plasma protein binding of amphetamine, catecholamines and related compounds".Acta Pharmacologica et Toxicologica.28(3). Wiley: 209–14.doi:10.1111/j.1600-0773.1970.tb00546.x.PMID5468075.
- ^Peaston RT, Weinkove C (January 2004)."Measurement of catecholamines and their metabolites".Annals of Clinical Biochemistry.41(Pt 1). SAGE Publications: 17–38.doi:10.1258/000456304322664663.PMID14713382.S2CID2330329.
- ^abcd"Epinephrine".The American Society of Health-System Pharmacists.Retrieved15 August2015.
- ^Hummel MD (2012)."Emergency Medications".In Pollak AN (ed.).Nancy Caroline's Emergency Care in the Streets(7th ed.). Burlington: Jones & Bartlett Learning. p. 557.ISBN9781449645861.Archivedfrom the original on 8 September 2017.
- ^abcLieberman M, Marks A, Peet A (2013).Marks' Basic Medical Biochemistry: A Clinical Approach(4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 175.ISBN9781608315727.
- ^"Adrenaline".21 August 2015.
- ^abcMalenka RC, Nestler EJ, Hyman SE (2009). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". In Sydor A, Brown RY (eds.).Molecular Neuropharmacology: A Foundation for Clinical Neuroscience(2nd ed.). New York, USA: McGraw-Hill Medical. p. 157.ISBN9780071481274.
Epinephrine occurs in only a small number of central neurons, all located in the medulla. Epinephrine is involved in visceral functions, such as the control of respiration. It is also produced by the adrenal medulla.
- ^Larrañaga M (2016).Hawley's Condensed Chemical Dictionary.New Jersey: John Wiley & Sons, Incorporated. p. 561.
- ^"Adrenaline: physiology and pharmacology | DermNet".dermnetnz.org.Retrieved20 March2023.
- ^Brown HF, DiFrancesco D, Noble SJ (July 1979). "How does adrenaline accelerate the heart?".Nature.280(5719): 235–236.Bibcode:1979Natur.280..235B.doi:10.1038/280235a0.PMID450140.S2CID4350616.
- ^Bell DR (2009).Medical physiology: principles for clinical medicine(3rd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 312.ISBN9780781768528.
- ^abKhurana I (2008).Essentials of Medical Physiology.Elsevier India. p. 460.ISBN9788131215661.
- ^Buckley E (2013).Venomous Animals and Their Venoms: Venomous Vertebrates.Elsevier. p. 478.ISBN9781483262888.
- ^Animal Physiology: Adaptation and Environment(5th ed.). Cambridge University Press. 1997. p. 510.ISBN9781107268500.
- ^Phan MG, Phan TS, Matsunami K, Otsuka H (April 2006)."Chemical and biological evaluation on scopadulane-type diterpenoids from Scoparia dulcis of Vietnamese origin".Chemical & Pharmaceutical Bulletin.54(4): 546–549.doi:10.1248/cpb.54.546.PMID16595962.
- ^Everard ML (February 2009). "Acute bronchiolitis and croup".Pediatric Clinics of North America.56(1): 119–133, x–xi.doi:10.1016/j.pcl.2008.10.007.PMID19135584.
- ^Paradisis M, Osborn DA (2004). "Adrenaline for prevention of morbidity and mortality in preterm infants with cardiovascular compromise".The Cochrane Database of Systematic Reviews(1): CD003958.doi:10.1002/14651858.CD003958.pub2.PMID14974048.
- ^Erickson-Lamy KA, Nathanson JA (August 1992)."Epinephrine increases facility of outflow and cyclic AMP content in the human eye in vitro".Investigative Ophthalmology & Visual Science.33(9): 2672–2678.PMID1353486.
- ^Rizzo V, Memmi M, Moratti R, Melzi d'Eril G, Perucca E (June 1996). "Concentrations ofL-dopa in plasma and plasma ultrafiltrates ".Journal of Pharmaceutical and Biomedical Analysis.14(8–10): 1043–1046.doi:10.1016/s0731-7085(96)01753-0.PMID8818013.
- ^Fuller RW (April 1982). "Pharmacology of brain epinephrine neurons".Annual Review of Pharmacology and Toxicology.22(1): 31–55.doi:10.1146/annurev.pa.22.040182.000335.PMID6805416.
- ^Cryer PE (August 1980). "Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system".The New England Journal of Medicine.303(8): 436–444.doi:10.1056/nejm198008213030806.PMID6248784.
- ^Barger G, Dale HH (October 1910)."Chemical structure and sympathomimetic action of amines".The Journal of Physiology.41(1–2): 19–59.doi:10.1113/jphysiol.1910.sp001392.PMC1513032.PMID16993040.
- ^Von Euler US (1946). "A specific sympathomimetic ergone in adrenergic nerve fibres (sympathin) and its relations to adrenaline and nor adrenaline".Acta Physiologica Scandinavica.12:73–97.doi:10.1111/j.1748-1716.1946.tb00368.x.
- ^Von Euler US, Hillarp NA (January 1956). "Evidence for the presence of noradrenaline in submicroscopic structures of adrenergic axons".Nature.177(4497): 44–45.Bibcode:1956Natur.177...44E.doi:10.1038/177044b0.PMID13288591.S2CID4214745.
- ^Warren J (January 1986). "The adrenal medulla and the airway".British Journal of Diseases of the Chest.80(1): 1–6.doi:10.1016/0007-0971(86)90002-1.PMID3004549.
- ^Twentyman OP, Disley A, Gribbin HR, Alberti KG, Tattersfield AE (October 1981). "Effect of beta-adrenergic blockade on respiratory and metabolic responses to exercise".Journal of Applied Physiology.51(4): 788–793.doi:10.1152/jappl.1981.51.4.788.PMID6795164.
- ^Richter EA, Galbo H, Christensen NJ (January 1981). "Control of exercise-induced muscular glycogenolysis by adrenal medullary hormones in rats".Journal of Applied Physiology.50(1).American Physiological Society:21–26.doi:10.1152/jappl.1981.50.1.21.PMID7009527.
- ^Canon WB (1931). "Studies on the conditions of activity in endocrine organs xxvii. Evidence that medulliadrenal secretion is not continuous".The American Journal of Physiology.98:447–453.doi:10.1152/ajplegacy.1931.98.3.447.
- ^Cryer PE, Tse TF, Clutter WE, Shah SD (August 1984). "Roles of glucagon and epinephrine in hypoglycemic and nonhypoglycemic glucose counterregulation in humans".The American Journal of Physiology.247(2 Pt 1): E198–E205.doi:10.1152/ajpendo.1984.247.2.E198.PMID6147094.
- ^Hoelzer DR, Dalsky GP, Schwartz NS, Clutter WE, Shah SD, Holloszy JO, et al. (July 1986). "Epinephrine is not critical to prevention of hypoglycemia during exercise in humans".The American Journal of Physiology.251(1 Pt 1): E104–E110.doi:10.1152/ajpendo.1986.251.1.E104.PMID3524257.(Retracted, seedoi:10.1152/ajpendo.1989.256.2.E338,PMID2645791)
- ^Hartman FA, Waite RH, McCordock HA (1922). "The liberation of epinephrine during muscular exercise".The American Journal of Physiology.62(2): 225–241.doi:10.1152/ajplegacy.1922.62.2.225.
- ^Von Euler US, Hellner S (September 1952). "Excretion of noradrenaline and adrenaline in muscular work".Acta Physiologica Scandinavica.26(2–3): 183–191.doi:10.1111/j.1748-1716.1952.tb00900.x.PMID12985406.
- ^Lund A (1950). "Simultaneous fluorimetric determinations of adrenaline and noradrenaline in blood".Acta Pharmacologica et Toxicologica.6(2): 137–146.doi:10.1111/j.1600-0773.1950.tb03460.x.PMID24537959.
- ^Johnson GA, Kupiecki RM, Baker CA (November 1980). "Single isotope derivative (radioenzymatic) methods in the measurement of catecholamines".Metabolism.29(11 Suppl 1): 1106–1113.doi:10.1016/0026-0495(80)90018-9.PMID7001177.
- ^Galbo H, Holst JJ, Christensen NJ (January 1975). "Glucagon and plasma catecholamine responses to graded and prolonged exercise in man".Journal of Applied Physiology.38(1): 70–76.doi:10.1152/jappl.1975.38.1.70.PMID1110246.
- ^Winder WW, Hagberg JM, Hickson RC, Ehsani AA, McLane JA (September 1978). "Time course of sympathoadrenal adaptation to endurance exercise training in man".Journal of Applied Physiology.45(3): 370–374.doi:10.1152/jappl.1978.45.3.370.PMID701121.
- ^Kindermann W, Schnabel A, Schmitt WM, Biro G, Hippchen M (May 1982). "[Catecholamines, GH, cortisol, glucagon, insulin, and sex hormones in exercise and beta 1-blockade (author's transl)]".Klinische Wochenschrift.60(10): 505–512.doi:10.1007/bf01756096.PMID6124653.S2CID30270788.
- ^Warren JB, Dalton N, Turner C, Clark TJ, Toseland PA (January 1984). "Adrenaline secretion during exercise".Clinical Science.66(1): 87–90.doi:10.1042/cs0660087.PMID6690194.
- ^Fitzgerald GA, Barnes P, Hamilton CA, Dollery CT (October 1980). "Circulating adrenaline and blood pressure: the metabolic effects and kinetics of infused adrenaline in man".European Journal of Clinical Investigation.10(5): 401–406.doi:10.1111/j.1365-2362.1980.tb00052.x.PMID6777175.S2CID38894042.
- ^Warren JB, Dalton N (May 1983). "A comparison of the bronchodilator and vasopressor effects of exercise levels of adrenaline in man".Clinical Science.64(5): 475–479.doi:10.1042/cs0640475.PMID6831836.
- ^Warren JB, Dalton N, Turner C, Clark TJ (November 1984)."Protective effect of circulating epinephrine within the physiologic range on the airway response to inhaled histamine in nonasthmatic subjects".The Journal of Allergy and Clinical Immunology.74(5): 683–686.doi:10.1016/0091-6749(84)90230-6.PMID6389647.
- ^Grossman M (1887). "Das muscarin-lungen-odem".Zeitschrift für klinische Medizin.12:550–591.
- ^Jackson DE (1912). "The pulmonary action of the adrenal glands".Journal of Pharmacology and Experimental Therapeutics.4:59–74.
- ^Kagawa J, Kerr HD (February 1970). "Effects of brief graded exercise on specific airway conductance in normal subjects".Journal of Applied Physiology.28(2): 138–144.doi:10.1152/jappl.1970.28.2.138.PMID5413299.
- ^Warren JB, Jennings SJ, Clark TJ (January 1984). "Effect of adrenergic and vagal blockade on the normal human airway response to exercise".Clinical Science.66(1): 79–85.doi:10.1042/cs0660079.PMID6228370.
- ^Jennings SJ, Warren JB, Pride NB (July 1987). "Airway caliber and the work of breathing in humans".Journal of Applied Physiology.63(1): 20–24.doi:10.1152/jappl.1987.63.1.20.PMID2957350.
- ^abMezzacappa ES, Katkin ES, Palmer SN (1999). "Epinephrine, arousal, and emotion: A new look at two-factor theory".Cognition and Emotion.13(2): 181–199.doi:10.1080/026999399379320.
- ^abToth M, Ziegler M, Sun P, Gresack J, Risbrough V (February 2013)."Impaired conditioned fear response and startle reactivity in epinephrine-deficient mice".Behavioural Pharmacology.24(1): 1–9.doi:10.1097/FBP.0b013e32835cf408.PMC3558035.PMID23268986.
- ^Cahill L, Alkire MT (March 2003). "Epinephrine enhancement of human memory consolidation: interaction with arousal at encoding".Neurobiology of Learning and Memory.79(2): 194–198.doi:10.1016/S1074-7427(02)00036-9.PMID12591227.S2CID12099979.
- ^abDornelles A, de Lima MN, Grazziotin M, Presti-Torres J, Garcia VA, Scalco FS, et al. (July 2007). "Adrenergic enhancement of consolidation of object recognition memory".Neurobiology of Learning and Memory.88(1): 137–142.doi:10.1016/j.nlm.2007.01.005.PMID17368053.S2CID27697668.
- ^Roozendaal B, McGaugh JL (December 2011)."Memory modulation".Behavioral Neuroscience.125(6): 797–824.doi:10.1037/a0026187.PMC3236701.PMID22122145.
- ^Tully K, Bolshakov VY (May 2010)."Emotional enhancement of memory: how norepinephrine enables synaptic plasticity".Molecular Brain.3(1): 15.doi:10.1186/1756-6606-3-15.PMC2877027.PMID20465834.
- ^Ferry B, Roozendaal B, McGaugh JL (June 1999)."Basolateral amygdala noradrenergic influences on memory storage are mediated by an interaction between beta- and Alpha 1-adrenoceptors".The Journal of Neuroscience.19(12): 5119–5123.doi:10.1523/JNEUROSCI.19-12-05119.1999.PMC6782651.PMID10366644.
- ^Feldberg W, Minz B, Tsudzimura H (June 1934)."The mechanism of the nervous discharge of adrenaline".The Journal of Physiology.81(3): 286–304.doi:10.1113/jphysiol.1934.sp003136.PMC1394156.PMID16994544.
- ^Burn JH, Hutcheon DE, Parker RH (September 1950)."Adrenaline and noradrenaline in the suprarenal medulla after insulin".British Journal of Pharmacology and Chemotherapy.5(3): 417–423.doi:10.1111/j.1476-5381.1950.tb00591.x.PMC1509946.PMID14777865.
- ^Outschoorn AS (December 1952)."The hormones of the adrenal medulla and their release".British Journal of Pharmacology and Chemotherapy.7(4): 605–615.doi:10.1111/j.1476-5381.1952.tb00728.x.PMC1509311.PMID13019029.
- ^Benedict CR, Grahame-Smith DG (August 1979)."Plasma adrenaline and noradrenaline concentrations and dopamine-beta-hydroxylase activity in myocardial infarction with and without cardiogenic shock".British Heart Journal.42(2): 214–220.doi:10.1136/hrt.42.2.214.PMC482137.PMID486283.
- ^Nadeau RA, de Champlain J (November 1979). "Plasma catecholamines in acute myocardial infarction".American Heart Journal.98(5): 548–554.doi:10.1016/0002-8703(79)90278-3.PMID495400.
- ^Larsson S, Svedmyr N (1977). "Tremor caused by sympathomimetics is mediated by beta 2-adrenoceptors".Scandinavian Journal of Respiratory Diseases.58(1): 5–10.PMID190674.
- ^Warren JB, O'Brien M, Dalton N, Turner CT (February 1984). "Sympathetic activity in benign familial tremor".Lancet.1(8374): 461–462.doi:10.1016/S0140-6736(84)91804-X.PMID6142198.S2CID36267406.
- ^Wurtman RJ, Pohorecky LA, Baliga BS (June 1972). "Adrenocortical control of the biosynthesis of epinephrine and proteins in the adrenal medulla".Pharmacological Reviews.24(2): 411–426.PMID4117970.
- ^Wright A, Jones IC (June 1955). "Chromaffin tissue in the lizard adrenal gland".Nature.175(4466): 1001–1002.Bibcode:1955Natur.175.1001W.doi:10.1038/1751001b0.PMID14394091.S2CID36742705.
- ^Coupland RE (April 1953). "On the morphology and adrenaline-nor-adrenaline content of chromaffin tissue".The Journal of Endocrinology.9(2): 194–203.doi:10.1677/joe.0.0090194.PMID13052791.
- ^abcdAronson JK (February 2000).""Where name and image meet" —the argument for "adrenaline"".BMJ.320(7233): 506–509.doi:10.1136/bmj.320.7233.506.PMC1127537.PMID10678871.
- ^European Pharmacopoeia 7.0 07/2008:2303
- ^"Has adrenaline become a generic trademark?".genericides.org.Archived fromthe originalon 1 May 2021.
- ^"Naming human medicines – GOV.UK".mhra.gov.uk.6 June 2019.
- ^abcdRao Y (June 2019). "The First Hormone: Adrenaline".Trends in Endocrinology and Metabolism.30(6): 331–334.doi:10.1016/j.tem.2019.03.005.PMID31064696.S2CID144207341.
- ^Shen H (2008).Illustrated Pharmacology Memory Cards: PharMnemonics.Minireview. p. 4.ISBN978-1-59541-101-3.
- ^Arnall DA, Marker JC, Conlee RK, Winder WW (June 1986). "Effect of infusing epinephrine on liver and muscle glycogenolysis during exercise in rats".The American Journal of Physiology.250(6 Pt 1): E641–E649.doi:10.1152/ajpendo.1986.250.6.E641.PMID3521311.
- ^Raz I, Katz A, Spencer MK (March 1991). "Epinephrine inhibits insulin-mediated glycogenesis but enhances glycolysis in human skeletal muscle".The American Journal of Physiology.260(3 Pt 1): E430–E435.doi:10.1152/ajpendo.1991.260.3.E430.PMID1900669.
- ^abSircar S (2007).Medical Physiology.Thieme Publishing Group. p. 536.ISBN978-3-13-144061-7.
- ^Vasudevan NT, Mohan ML, Goswami SK, Naga Prasad SV (November 2011)."Regulation of β-adrenergic receptor function: an emphasis on receptor resensitization".Cell Cycle.10(21): 3684–3691.doi:10.4161/cc.10.21.18042.PMC3266006.PMID22041711.
- ^Berg JM, Tymoczko JL, Stryer L (2002). "Epinephrine and Glucagon Signal the Need for Glycogen Breakdown".Biochemistry(5th ed.). New York: W.H. Freeman.ISBN0-7167-3051-0.
- ^"Guideline 11.5: Medications in Adult Cardiac Arrest"(PDF).Australian Resuscitation Council.December 2010.Retrieved7 March2015.
- ^Chang YT, Huang WC, Cheng CC, Ke MW, Tsai JS, Hung YM, et al. (February 2020)."Effects of epinephrine on heart rate variability and cytokines in a rat sepsis model".Bosnian Journal of Basic Medical Sciences.20(1): 88–98.doi:10.17305/bjbms.2018.3565.PMC7029199.PMID29984678.
- ^Burnett AM, Segal N, Salzman JG, McKnite MS, Frascone RJ (August 2012). "Potential negative effects of epinephrine on carotid blood flow and ETCO2during active compression-decompression CPR utilizing an impedance threshold device ".Resuscitation.83(8): 1021–1024.doi:10.1016/j.resuscitation.2012.03.018.PMID22445865.
- ^Raymondos K, Panning B, Leuwer M, Brechelt G, Korte T, Niehaus M, et al. (May 2000). "Absorption and hemodynamic effects of airway administration of adrenaline in patients with severe cardiac disease".Annals of Internal Medicine.132(10): 800–803.doi:10.7326/0003-4819-132-10-200005160-00007.PMID10819703.S2CID12713291.
- ^Baselt R (2008).Disposition of Toxic Drugs and Chemicals in Man(8th ed.). Foster City, CA: Biomedical Publications. pp. 545–547.ISBN978-0-9626523-7-0.
- ^von Bohlen und Haibach O, Dermietzel R (2006).Neurotransmitters and Neuromodulators: Handbook of Receptors and Biological Effects.Wiley-VCH. p. 125.ISBN978-3-527-31307-5.
- ^Kirshner N, Goodall M (June 1957). "The formation of adrenaline from noradrenaline".Biochimica et Biophysica Acta.24(3): 658–659.doi:10.1016/0006-3002(57)90271-8.PMID13436503.
- ^Axelrod J (May 1962)."Purification and properties of phenylethanolamine-N-methyl transferase ".The Journal of Biological Chemistry.237(5): 1657–1660.doi:10.1016/S0021-9258(19)83758-4.PMID13863458.
- ^Broadley KJ (March 2010). "The vascular effects of trace amines and amphetamines".Pharmacology & Therapeutics.125(3): 363–375.doi:10.1016/j.pharmthera.2009.11.005.PMID19948186.
- ^Lindemann L, Hoener MC (May 2005). "A renaissance in trace amines inspired by a novel GPCR family".Trends in Pharmacological Sciences.26(5): 274–281.doi:10.1016/j.tips.2005.03.007.PMID15860375.
- ^Wang X, Li J, Dong G, Yue J (February 2014). "The endogenous substrates of brain CYP2D".European Journal of Pharmacology.724:211–218.doi:10.1016/j.ejphar.2013.12.025.PMID24374199.
- ^Nelson L, Cox M (2004).Lehninger Principles of Biochemistry(4th ed.). New York: Freeman. p.908.ISBN0-7167-4339-6.
- ^"SLC18 family of vesicular amine transporters".Guide to Pharmacology.IUPHAR/BPS.Retrieved21 August2015.
- ^Oanca G, Stare J, Mavri J (December 2017). "How fast monoamine oxidases decompose adrenaline? Kinetics of isoenzymes A and B evaluated by empirical valence bond simulation".Proteins.85(12): 2170–2178.doi:10.1002/prot.25374.PMID28836294.S2CID5491090.
- ^Szablewski L (2011).Glucose Homeostasis and Insulin Resistance.Bentham Science Publishers. p. 68.ISBN9781608051892.
- ^Skalski JH, Kuch J (April 2006)."Polish thread in the history of circulatory physiology".Journal of Physiology and Pharmacology.57(Suppl 1): 5–41.PMID16766800.
- ^Bates WH (16 May 1896)."The Use of Extract of Suprarenal Capsule in the Eye".New York Medical Journal:647–650.Retrieved7 March2015.
Read before the Section in Ophthalmology of the New York Academy of Medicine, 20 April 1896
- ^Takamine J (1901)."The isolation of the active principle of the suprarenal gland".The Journal of Physiology.Great Britain: Cambridge University Press: xxix–xxx.
- ^Bennett MR (June 1999). "One hundred years of adrenaline: the discovery of autoreceptors".Clinical Autonomic Research.9(3): 145–159.doi:10.1007/BF02281628.PMID10454061.S2CID20999106.
- ^abBall CM, Featherstone PJ (May 2017)."The early history of adrenaline".Anaesthesia and Intensive Care.45(3): 279–281.doi:10.1177/0310057X1704500301.PMID28486885.
- ^Arthur G (May 2015)."Epinephrine: a short history".The Lancet. Respiratory Medicine.3(5): 350–351.doi:10.1016/S2213-2600(15)00087-9.PMID25969360.
- ^Zuckerman M (2007).Sensation seeking and risky behavior.Washington, DC: American Psychological Association.doi:10.1016/0191-8869(93)90173-Z.ISBN9781591477389.
- ^abJänig W (6 July 2006).The integrative action of the autonomic nervous system: neurobiology of homeostasis.England: Cambridge University Press. pp. 143–146.ISBN9780521845182.
- ^Deane WH, Rubin BL (1964). "Absence of adrenal meduallary secretions".The Adrenocortical Hormones Their Origin – Chemistry Physiology and Pharmacology.Berlin, Heidelberg: Springer Berlin Heidelberg. p. 105.ISBN9783662131329.
- ^Frankenhaeuser M, Jarpe G, Matell G (February 1961). "Effects of intravenous infusions of adrenaline and noradrenaline on certain psychological and physiological functions".Acta Physiologica Scandinavica.51(2–3): 175–186.doi:10.1111/j.1748-1716.1961.tb02126.x.PMID13701421.
- ^Wise J (28 December 2009)."When Fear Makes Us Superhuman".Scientific American.Retrieved25 August2015.
- ^Wise J (8 December 2009).Extreme Fear: The Science of Your Mind in Danger(1st ed.). New York:Palgrave Macmillan.ISBN9780230101807.
External links
edit- Media related toEpinephrineat Wikimedia Commons
- "U.S. National Library of Medicine: Drug Information Portal – Epinephrine".Archived fromthe originalon 14 December 2019.