Thetrochlear nerve(/ˈtrɒklɪər/),[1](lit.pulley-likenerve) also known as thefourth cranial nerve,cranial nerve IV,orCN IV,is acranial nervethat innervates a single muscle - thesuperior oblique muscleof the eye (which operates through thepulley-liketrochlea). Unlike most other cranial nerves, the trochlear nerve is exclusively amotor nerve(somaticefferent nerve).
| Trochlear nerve | |
|---|---|
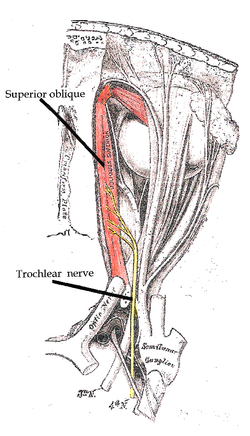 The trochlear nerve entering theorbit,seen from above, supplies thesuperior oblique muscle | |
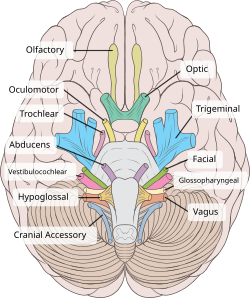 The trochlear nerve (CN IV) seen with othercranial nerves.It is the only cranial nerve to emerge from behind the brainstem, and curves around it to reach the front | |
| Details | |
| Innervates | Superior oblique muscle |
| Identifiers | |
| Latin | nervus trochlearis |
| MeSH | D014321 |
| NeuroNames | 466 |
| TA98 | A14.2.01.011 |
| TA2 | 6191 |
| FMA | 50865 |
| Anatomical terms of neuroanatomy | |
The trochlear nerve is unique among the cranial nerves in several respects:
- It is thesmallestnerve in terms of the number of axons it contains.
- It has the greatest intracranial length.
- It is the only cranial nerve that exits from the dorsal (rear) aspect of thebrainstem.
- It innervates a muscle, the superior oblique muscle, on the opposite side (contralateral) from its nucleus. The trochlear nervedecussateswithin the brainstem before emerging on the contralateral side of the brainstem (at the level of theinferior colliculus). An injury to the trochlear nucleus in the brainstem will result in an contralateralsuperior obliquemuscle palsy, whereas an injury to the trochlear nerve (after it has emerged from the brainstem) results in an ipsilateralsuperior obliquemuscle palsy.
The superior oblique muscle which the trochlear nerve innervates ends in a tendon that passes through a fibrous loop, thetrochlea,located anteriorly on the medial aspect of the orbit.Trochleameans “pulley” in Latin; the fourth nerve is thus also named after this structure. The wordstrochleaandtrochlear(/ˈtrɒkliə/,/ˈtrɒkliər/) come fromAncient Greekτροχιλέαtrokhiléa,“pulley; block-and-tackle equipment”.
Structure
editThe trochlear nerve provides motorinnervationto thesuperior oblique muscleof the eye,[2]a skeletal muscle; the trochlear nerve thus carries axons ofgeneral somatic efferent type.[citation needed]
Course
editEach trochlear nerve originates from atrochlear nucleusin the medialmidbrain.From their respective nuclei, the two trochlear nerves then travel dorsal-ward through the substance of the midbrain surrounded by theperiaqueductal gray,crossing over (decussating)within the midbrain before emerging from the dorsal midbrain[3][4]just inferior to theinferior colliculus.[4]Each trochlear nerve thus comes to course on the contralateral side, first passing laterally (to the side) and then anteriorly around thepons,[3]then running forward toward the eye in thesubarachnoid space.It passes between theposterior cerebral arteryand thesuperior cerebellar artery.It then pierces thedurajust under free margin of thetentorium cerebelli,close to the crossing of the attached margin of the tentorium and within millimeters of theposterior clinoid process.[5]It runs on the outer wall of thecavernous sinus.[2]Finally, it enters the orbit through thesuperior orbital fissureand to innervate thesuperior oblique muscle.[2]
Development
editThe human trochlear nerve is derived from thebasal plateof theembryonicmidbrain.[citation needed]
Clinical significance
editVertical diplopia
editInjury to the trochlear nerve cause weakness of downward eye movement with consequent verticaldiplopia(double vision). The affected eye drifts upward relative to the normal eye, due to the unopposed actions of the remaining extraocular muscles. The patient sees two visual fields (one from each eye), separated vertically. To compensate for this, patients learn to tilt the head forward (tuck the chin in) in order to bring the fields back together—to fuse the two images into a single visual field. This accounts for the “dejected” appearance of patients with “pathetic nerve” palsies.
Torsional diplopia
editTrochlear nerve palsy also affects torsion (rotation of the eyeball in the plane of the face). Torsion is a normal response to tilting the head sideways. The eyes automatically rotate in an equal and opposite direction, so that the orientation of the environment remains unchanged—vertical things remain vertical.
Weakness of intorsion results intorsional diplopia,in which two different visual fields, tilted with respect to each other, are seen at the same time. To compensate for this, patients with trochlear nerve palsies tilt their heads to the opposite side, in order to fuse the two images into a single visual field.
The characteristic appearance of patients with fourth nerve palsies (head tilted to one side, chin tucked in) suggests the diagnosis, but other causes must be ruled out. For example,torticolliscan produce a similar appearance.
Causes
editThe clinical syndromes can originate from both peripheral and central lesions.
Peripheral lesion
editA peripheral lesion is damage to the bundle of nerves, in contrast to a central lesion, which is damage to the trochlear nucleus. Acute symptoms are probably a result of trauma or disease, while chronic symptoms probably are congenital.
Acute palsy
editThe most common cause ofacutefourth nerve palsy is head trauma.[6]Even relatively minor trauma can transiently stretch the fourth nerve (by transiently displacing the brainstem relative to the posterior clinoid process). Patients with minor damage to the fourth nerve will complain of “blurry” vision. Patients with more extensive damage will notice frank diplopia and rotational (torsional) disturbances of the visual fields. The usual clinical course is complete recovery within weeks to months.
Isolated injury to the fourth nerve can be caused by any process that stretches or compresses the nerve. A generalized increase in intracranial pressure—hydrocephalus,pseudotumor cerebri,hemorrhage,edema—will affect the fourth nerve, but theabducens nerve(VI) is usually affected first (producinghorizontal diplopia,notvertical diplopia). Infections (meningitis,herpes zoster), demyelination (multiple sclerosis),diabetic neuropathyandcavernous sinusdisease can affect the fourth nerve, as can orbital tumors andTolosa–Hunt syndrome.In general, these diseases affect other cranial nerves as well. Isolated damage to the fourth nerve is uncommon in these settings.
Chronic palsy
editThe most common cause ofchronicfourth nerve palsy is a congenital defect, in which the development of the fourth nerve (or its nucleus) is abnormal or incomplete. Congenital defects may be noticed in childhood, but minor defects may not become evident until adult life, when compensatory mechanisms begin to fail. Congenital fourth nerve palsies are amenable to surgical treatment.
Central lesion
editCentral damage is damage to the trochlear nucleus. It affects thecontralateraleye. The nuclei of other cranial nerves generally affectipsilateralstructures (for example, the optic nerves - cranial nerves II - innervate both eyes).
The trochlear nucleus and its axons within the brainstem can be damaged by infarctions,hemorrhage,arteriovenous malformations,tumors anddemyelination.Collateral damage to other structures will usually dominate the clinical picture.
The fourth nerve is one of the final common pathways for cortical systems that control eye movement in general. Cortical control of eye movement (saccades,smooth pursuit,accommodation) involvesconjugate gaze,not unilateral eye movement.
Clinical assessment
editThe trochlear nerve is tested by examining the action of its muscle, the superior oblique. When acting on its own this muscle depresses and abducts the eyeball. However, movements of the eye by the extraocular muscles aresynergistic(working together). Therefore, the trochlear nerve is tested by asking the patient to look 'down and in' as the contribution of the superior oblique is greatest in this motion. Common activities requiring this type of convergent gaze are reading the newspaper and walking down stairs. Diplopia associated with these activities may be the initial symptom of a fourth nerve palsy.
Alfred Bielschowsky'shead tilt testis a test for palsy of the superior oblique muscle caused by damage to cranial nerve IV (trochlear nerve).
Other animals
editHomologoustrochlear nerves are found in alljawed vertebrates.The unique features of the trochlear nerve, including its dorsal exit from the brainstem and its contralateral innervation, are seen in the primitive brains of sharks.[7]
References
edit- ^"Trochlear | Definition of Trochlear by Oxford Dictionary on Lexico also meaning of Trochlear".Lexico Dictionaries | English.Archived fromthe originalon November 12, 2020.
- ^abcStandring, Susan, ed. (2016). ""Orbit and accessory visual apparatus: trochlear nerve"".Gray's anatomy: the anatomical basis of clinical practice(41st ed.). Philadelphia. p. 678.ISBN9780702052309.OCLC920806541.
{{cite book}}:CS1 maint: location missing publisher (link) - ^abKim, Seung Y.; Motlagh, Mahsaw; Naqvi, Imama A. (2022),"Neuroanatomy, Cranial Nerve 4 (Trochlear)",StatPearls,Treasure Island (FL): StatPearls Publishing,PMID30725929,retrieved2023-01-03
- ^abPatestas, Maria A.; Gartner, Leslie P. (2016).A Textbook of Neuroanatomy(2nd ed.). Hoboken, New Jersey: Wiley-Blackwell. p. 90.ISBN978-1-118-67746-9.
- ^Bisaria KK. "Cavernous portion of the trochlear nerve with special reference to its site of entrance".J. Anat.159:29–35, 1988
- ^Hoya K, Kirino T. Traumatic "Trochlear Nerve Palsy Following Minor Occipital Impact".Neurol Med Chir40:358-360, 2000
- ^Maisey JG. "Morphology of the Braincase in the Broadnose Sevengill SharkNotorynchus(Elasombranchii, Hexanchiformes), Based on CT Scanning ".American Museum Novitates,Number 3429. New York: American Museum of Natural History, 2004
Bibliography
edit- Blumenfeld H. Neuroanatomy Through Clinical Cases. Sinauer Associates, 2002
- Brodal A. Neurological Anatomy in Relation to Clinical Medicine, 3rd ed. Oxford University Press, 1981
- Brodal P. The Central Nervous System, 3rded. Oxford University Press, 2004
- Butler AB, Hodos W. Comparative Vertebrate Neuroanatomy, 2nd ed. Wiley-Interscience, 2005
- Carpenter MB. Core Text of Neuroanatomy, 4th ed. Williams & Wilkins, 1991
- Kandel ER, Schwartz JH, Jessell TM. Principles of Neural Science, 4th ed. McGraw-Hill, 2000
- Martin JH. Neuroanatomy Text and Atlas, 3rd ed. McGraw-Hill, 2003
- Patten J. Neurological Differential Diagnosis, 2nd ed. Springer, 1996
- Ropper, AH, Brown RH. Victor's Principles of Neurology, 8th ed. McGraw-Hill, 2005
- Standring S (ed.) Gray's Anatomy, 39th edition. Elsevier Churchill Livingstone, 2005
- Wilson-Pauwels L, Akesson EJ, Stewart PA. Cranial Nerves: Anatomy and Clinical Comments. Decker, 1998
Additional images
edit-
Dura mater and its processes exposed by removing part of the right half of the skull, and the brain.
-
Hind- and mid-brains; postero-lateral view.
-
Dissection showing origins of right ocular muscles, and nerves entering by the superior orbital fissure.
-
Upper part of medulla spinalis and hind- and mid-brains; posterior aspect, exposed in situ.
-
Trochlear nerve.Deep dissection.Superior view.
External links
edit- hier-449atNeuroNames
- oph/697ateMedicine- "Trochlear Nerve Palsy"
- MedEd at LoyolaGrossanatomy/h_n/cn/cn1/cn4.htm
- lesson3at The Anatomy Lesson by Wesley Norman (Georgetown University) (orbit2)
- cranialnervesat The Anatomy Lesson by Wesley Norman (Georgetown University) (IV)
- Animations of extraocular cranial nerve and muscle function and damage (University of Liverpool)
- Trochlear nerveat Neurolex