| Toolbox |
|---|
| Thispeer reviewdiscussion is closed. |
I've listed this article for peer review because I would like for it to have both high-quality prose as well as high-quality scientific content throughout. It was last up for peer review in 2012, and I've made hundreds of edits and updates to the article since late 2019. I plan to submit this article to theWikiJournal of Medicineandpotentially,to the featured article process. I have some ideas as to where I could polish the article further, but I would appreciate having some fresh looks and input from others.
Thank you,Biosthmors(talk)16:13, 16 April 2021 (UTC)
For anyone who might wonder why this peer review currently looks stagnant I am now busy IRL. I plan to be able to focus on article improvement again in mid- to late-June. I am very happy to receive further feedback in the interim or thereafter. Thank you.Biosthmors(talk)05:55, 28 May 2021 (UTC)
Comments from NikosGouliaros]
editCongratulations and thanks for the obvious hard work that has been put to this article. Please read what follows as a humble, well-meaning, good-faith review. It will be updated section by section.
- Thank you for the kind words and introduction. I look forward to hearing your feedback, and I appreciate you taking the time. Please also bear with me when I have questions or ideas that might differ from your own.
Lead
editBackground
editThemedical manual of style(MEDMOS) does not include such a section. Moreover, the information it currently contains can easily be included in other sections, like Pathophysiology. The second paragraph hardly includes any "background" information; it would better be classified under Classification, Complications, and Epidemiology.A section onclassificationcan include not only what subtypes a condition like DVT can comprise, but also what groups of conditions DVT is a part of, e.g. the spectrum of VTE.My humble opinion is that the article would benefit from removing the whole section and repositioning the information it contains in the respective sections, as delineated in MEDMOS.- Thank you for helping me see how the section could be split up and distributed. It no longer remains.
If one paragraph is collectively supported by one source,it is sufficientfor the inline citation to appear once at the end of the paragraph.- Noted, made one related change
Source[21]is inappropriate for the information it supports. Itself it cites:ISTH Steering Committee for World Thrombosis Day (2014)."Thrombosis: a major contributor to the global disease burden".J Thromb Haemost.12(10): 1580–90.doi:10.1111/jth.12698.PMID25302663..(More on that under Epidemiology.)- I went ahead andremovedthis statement after reviewing the 2014 source. Thanks. After looking at the 2014 source, I feel like the sentence tries to sound important but is ultimately unhelpful and vague.
[22]citesa possibly predatory journal,that is not indexed in MEDLINE. A more appropriate source is:Pristipino C, Sievert H, D'Ascenzo F, Mas JL, Meier B, Scacciatella P; et al. (2019)."European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism".EuroIntervention.14(13): 1389–1402.doi:10.4244/EIJ-D-18-00622.PMID30141306.{{cite journal}}:CS1 maint: multiple names: authors list (link).- Thank you for the suggested source. It appears to be a very high-quality source. If you would please allow me, I have some questions that relate to the concept of "predatory journals". For what it's worth, I did see that a couple authors in theFrontiers in Neurologyarticle publish widely[1][2]in medical journals, so I think the source is reliable for its claim.[3]My thinking is that the VTE/PFO/paradoxical embolism/stroke concept is a fairly well-known one in medicine. So I don't think it needs a top-tier source. I see at WP:MEDRS that MEDLINE indexed journals are preferred, but do we know why / what evidence there is that journals in PubMed that are MEDLINE indexed are thought to be more reliable than non-MEDLINE indexed ones? Personally, I feel like the text of the current source is more accessible for lay readers should they wish to verify the concept. The wording of the suggested high-quality source reads as more technical, in my opinion. I see that the first sentence ofthe relevant subsectionin MEDRS says "Avoid articles from journals with a poor reputation for fact-checking and accuracy". Is there any indication thatFrontiers in Neurologyhas this sort of reputation? I would guess that that's not the case, simply because these highly-published authors chose to submit their work to the journal.Biosthmors(talk)21:25, 17 April 2021 (UTC)
- Fair questions. I'm afraid I'm not experienced enough as an editor to give definitive answers. One can't have a well-founded opinion on everything in Wikipedia, and in medical sourcing; sometimes you just follow consensus on best practice. The "Frontiers" series of Journals are called "controversial" in the Wikipedia page ontheir publisherand included ina list used in Wikipedia;please check alsoWikipedia:Vanity and predatory publishing.Medline-inde xing is a very widely used determinant of a Journal's reliability, all over the medical world. You can check if a Journal is indexed in Medlinehere(Search, eg, for: "Frontiers in Neurology" [Title]). There are the good Journals, and the less well-known ones, which are often of a local interest, or in languages other than English; I'm not sure if you can find any researchers without publications in non-Medline-indexed journals, even if they are top in their field. Sure, it's no big deal to use less-than-ideal sources, especially for readily believable info; but I failed to mention that this review followsfeatured article criteria,which call for "high-quality reliable sources".NikosGouliaros(talk)22:56, 17 April 2021 (UTC)
- Thank you for the reply. I did some research, and this journal is not listed as predatory here:Manca A, Martinez G, Cugusi L, Dragone D, Dvir Z, Deriu F (June 2017). "The surge of predatory open-access in neurosciences and neurology".Neuroscience.353:166–173.doi:10.1016/j.neuroscience.2017.04.014.PMID28433651..Andthissource lists features of potential predatory journals in Box 1. I doubt they apply toFrontiers in Neurology.In my opinion, the article in this journal is a high-quality source. The journal has editors, an editorial board, peer review, etc. and the authors are established academics. But I did go ahead and add the other source you suggested. I haven't yet removed the Frontiers source because I feel like it may add value to readers in aiding verification.
- Fair questions. I'm afraid I'm not experienced enough as an editor to give definitive answers. One can't have a well-founded opinion on everything in Wikipedia, and in medical sourcing; sometimes you just follow consensus on best practice. The "Frontiers" series of Journals are called "controversial" in the Wikipedia page ontheir publisherand included ina list used in Wikipedia;please check alsoWikipedia:Vanity and predatory publishing.Medline-inde xing is a very widely used determinant of a Journal's reliability, all over the medical world. You can check if a Journal is indexed in Medlinehere(Search, eg, for: "Frontiers in Neurology" [Title]). There are the good Journals, and the less well-known ones, which are often of a local interest, or in languages other than English; I'm not sure if you can find any researchers without publications in non-Medline-indexed journals, even if they are top in their field. Sure, it's no big deal to use less-than-ideal sources, especially for readily believable info; but I failed to mention that this review followsfeatured article criteria,which call for "high-quality reliable sources".NikosGouliaros(talk)22:56, 17 April 2021 (UTC)
- Another way to look up journals is athttps:// scopus /sourcesIf you're looking for a rule of thumb, I avoid anything that turns up in the bottom 20% (because research indicates that the bottom 20% of journals is particularly risky) and I think twice about anything in the next quintile. But if it's in the median quintile or higher, I don't worry about it. Most Frontiers journals are better than they used to be, and even back in the day, about half of them were okay. Wikipedia has them on a "double check" list, not a "probably bad" list.WhatamIdoing(talk)18:01, 18 April 2021 (UTC)
- Thanks for explaining that approach. I used scopus to look up the journal, and it is ranked as 180/348 in the field of clinical Neurology.Biosthmors(talk)18:45, 18 April 2021 (UTC)
- Thank you for the suggested source. It appears to be a very high-quality source. If you would please allow me, I have some questions that relate to the concept of "predatory journals". For what it's worth, I did see that a couple authors in theFrontiers in Neurologyarticle publish widely[1][2]in medical journals, so I think the source is reliable for its claim.[3]My thinking is that the VTE/PFO/paradoxical embolism/stroke concept is a fairly well-known one in medicine. So I don't think it needs a top-tier source. I see at WP:MEDRS that MEDLINE indexed journals are preferred, but do we know why / what evidence there is that journals in PubMed that are MEDLINE indexed are thought to be more reliable than non-MEDLINE indexed ones? Personally, I feel like the text of the current source is more accessible for lay readers should they wish to verify the concept. The wording of the suggested high-quality source reads as more technical, in my opinion. I see that the first sentence ofthe relevant subsectionin MEDRS says "Avoid articles from journals with a poor reputation for fact-checking and accuracy". Is there any indication thatFrontiers in Neurologyhas this sort of reputation? I would guess that that's not the case, simply because these highly-published authors chose to submit their work to the journal.Biosthmors(talk)21:25, 17 April 2021 (UTC)
The last paragraph, on unusual, non-deep, vein thrombosis, is perhaps unnecessary.NikosGouliaros(talk)23:51, 16 April 2021 (UTC)- Agreed, thanks. Moved tovenous thrombosis
Signs and symptoms
edit- The text starting from "Signs and symptoms alone are not sufficiently..." until the end, with info on diagnostic pathways and differential diagnosis, belongs to Diagnosis.
Agreed.Update: I actually reinserted the sentence with modifications. It saysSigns and symptoms help in determining the likelihood of DVT, but they are not used alone for diagnosis.[4]Does it still sound out of place to you? Link:Deep_vein_thrombosis#Signs_and_symptomsBiosthmors(talk)14:29, 23 April 2021 (UTC)
- What remains would benefit from more details. It's a type of medical content that is difficult to source only from journal articles, without also citing a textbook. The ones on my bookshelves are a bit old and therefore not ideal, but literature on signs and symptoms doesn't change so fast as to demand the most recent citations; so I'm attempting a rewrite:
"DVT affects the legs approximately 10 times more often than the arms.[1]People with DVT complain of pain, tightness, or a sense of fulness of the affected limb; if it is a leg, symptoms are worsened by standing and walking.[2][3]The leg or arm may be swollen, and when pressure is applied to a small area, the indentation persists after its release ( "pitting edema" ); it may also be warm andreddened,cyanoticordiscolored.Tenderness is another sign, especially along the affected vein, which may be palpable as a cord. Distented superficial veins and prominent venouscollateralsmay be noted, and vein distention is not reversable by raising the member.[3][4]The presence ofinflammationof the vein walls, which may precede or follow clot formation and is termedthrombophlebitis,may cause the skin above them to becomeredand hot. They patient may havefeverand complain ofcrampsin the adjoining muscles.[3]
DVT located at thecalfmay have fewer manifestations, especially if only one vein is obstructed, allowing venous blood return to continue through the rest.[4]On the other hand, proximal DVT located at thefemoraloriliac veinscan produce intense pain and massive leg edema, as well as pallor from reduced arterial flow (due toarterial spasm,or theinterstitialpressure from the edema surpassing thecapillaryperfusion pressure). This condition is referred to as phlegmasia alba dolens (painful white inflammation). Total obstruction of venous outflow can cause fluid to accumulate and increase interstitial pressures further, collapsing the arteries and producinglimb ischemiathat gives it a cyanotic hue (phlegmasia cerulea dolens,painful blue inflammation). Interstitial fluid accumulation can reduce intravascular fluid volume, and cause the blood pressure to drop, along with other manifestations ofhypovolemia.[3][4][5]"This paragraph is not complete, as it lacks info on what changes with different sites of DVT, eg femoral vs saphenous veins, and with the presence of inflammation; I can come back with more.(I seem to have become a writer instead of a reviewer, so another reviewer, of what I myself write, is needed.) Note that StatPearls, from what I read in archived discussions in WikiProject Medicine, is not the best of sources, but I consider it acceptable for simple information on signs and symptoms, and pathophysiology. It's obvious that I too, unfortunately, lack a good vascular medicine textbook.- I think this is a great idea, and I totally agree with you on the need to find other sources that might not have been published in the last several years. I like the text you propose. The only thing I'd add is that I've heard that "palpable cords" are actually superficial vein thrombosis (SVT) (or was itsuperficial thrombophlebitis?), thus why you can feel them (they aren't deep), and because an association with SVT and DVT raises suspicion for DVT.
- (We have been editing at the same time). I don't mind removing the palpable cords, it's probably one of the things that physicians read in books but never encounter in real life.NikosGouliaros(talk)18:13, 18 April 2021 (UTC)
- I could go either way, depending on what the sources say.
- NikosGouliaros,I have expanded the signs and symptoms section more in line with the text you proposed.[5]While our texts vary quite a bit, there is some overlap. Do you think there is anything in your proposed text above that definitely deserves mention in the article? Thank you.Biosthmors(talk)22:18, 8 May 2021 (UTC)
- Also, FYI, I was currently planning to discuss more about the different places/veins where DVT can form in the classification section.Biosthmors(talk)22:21, 8 May 2021 (UTC)
- (We have been editing at the same time). I don't mind removing the palpable cords, it's probably one of the things that physicians read in books but never encounter in real life.NikosGouliaros(talk)18:13, 18 April 2021 (UTC)
Skimming source [19] I cannot find support for asymptomatic DVT,and I couldn't find it in a quick search through PubMed either.The source can be changed to[6],and the text may be expanded as:People with DVT may experience no symptoms, especially if they are staying recumbent because of some other condition.[6]
This source is not ideal, as its 13 years of age may be challenged in a Featured Article Review, but the statement it sources in my opinion doesn't necessarily need a very recent publication.- I have done away with these concepts in the Classifications system and postedmy logic(it's just not discussed in the article) on the talk page.Biosthmors(talk)19:59, 8 May 2021 (UTC)
- The signs and symptoms section currently cites the source you recommended and includes the concept but with slightly altered prose. I also am doubtful that we need a more updated source for this.Biosthmors(talk)20:05, 8 May 2021 (UTC)
Phlegmasia cerulea dolens,and also phlegmasia alba dolens, probably merit a mention in this section, and perhaps only in this section. I can come back with more. In a sense, they too are complications of DVT.- I thinkphlegmasia cerulea dolensmerits a mention here, good idea. I spent a fair amount of time in the literature looking up phlegmasia cerulea dolens and phlegmasia alba dolens last year because I was confused on this point (how much they should be covered in the DVT article). I concluded that term phlegmasia alba dolens was not used in the current DVT literature and that the profile of phlegmasia cerulea dolens was rising in the current literature. That's why I mention it in several places, because management of iliofemoral DVT can overlap with phlegmasia cerulea dolens. Phlegmasia cerulea dolens is simply a severe form of DVT and because it is DVT it should be discussed throughout where it merits mention, in my opinion.
- While you were writing this I was adding material on the two types of phlegmasia dolens. On the white one, I have no strong feelings. However, although I have no access to the full text, searching in the Google Books Preview I see it is mentioned in Rutherford's vascular surgery and endovascular therapy, which is a major surgical textbook.NikosGouliaros(talk)18:13, 18 April 2021 (UTC)
- I would be happy to review your text, but I would need access to the sources. I'm wary of StatPearls myself. I was told it's a beginner source in medicine, and by extension, not high-quality. Did you want to go ahead and add your text or wait for it to be reviewed? I can add it and credit you in the edit summary. I didn't want to leave just one sentence behind in the Diagnosis section in the interim.
- Phlegmasia cerulea dolens is now discussed in the complications section.
- While you were writing this I was adding material on the two types of phlegmasia dolens. On the white one, I have no strong feelings. However, although I have no access to the full text, searching in the Google Books Preview I see it is mentioned in Rutherford's vascular surgery and endovascular therapy, which is a major surgical textbook.NikosGouliaros(talk)18:13, 18 April 2021 (UTC)
- I was thinking of starting with something like, "DVT symptoms, when present, classically affect a single leg. Less commonly, they affect an arm."Maybe also this:"Rarely, more than one limb is affected."Biosthmors(talk)15:48, 21 April 2021 (UTC)
According to MEDMOS, Complications should be included in this section. They can be described in a subsection, as inDengue fever,or (more commonly) simply mentioned along with their clinical presentation as separate paragraphs, as inInfluenza.I propose adding one or two paragraphs, with symptoms and signs of pulmonary embolism, paradoxic embolism, and post thrombotic syndrome. Doing so will eliminate most of the content of a section on Complications, which is not allowed for in the MEDMOS. The information on recurrent DVT, that is currently also included in Complications, may be moved to prognosis. 22:26, 17 April 2021 (UTC) 22:26, 17 April 2021 (UTC)Edited: 18:03, 18 April 2021 (UTC)- I have placed acute complications in signs and symptoms under a subsection since they can directly and immediately cause clot-related symptoms. Personally, I think the long-term sequela of post-thrombotic syndrome is better suited for the prognosis section. (The section was previously named Prognosis, then I recently changed it to Complications, and now I have just changed it back to Prognosis.) Clots over a much longer time span can become a ball of fibrosis before they might cause post-thrombotic syndrome, so to me its conceptually different. I think of post-thrombotic syndrome as more of a sign of chronic DVT, not a sign of acute DVT.Biosthmors(talk)22:57, 22 April 2021 (UTC)
Classification
editThis section can have various positions, but this one is fine.- Thanks.
As I wrote earlier, I think it's better of pulmonary embolism (PE) is described briefly as a complication of DVT in Signs and symptoms; therefore, I would move the first sentence of this section there (if no other source is at hand,Braunwald (2019)can be cited). The second sentence contains the info that I prefer this section to start with (i.e., that DVT and PE constitute the entity of venous thromboembolism); the source is fine.- Now this is cited in a complications subsection of the signs and symptoms section.
I believe it's currently sourceless because the context provides basic medical facts, but I would rather cite an freely-available source over a textbook for this information if you think a citation is necessary.The prose has been cited to sources,but the first sentence goes into more basic science facts (to make it more understandable for lay readers) than the first source delves into.
- Now this is cited in a complications subsection of the signs and symptoms section.
About two-thirds of VTE manifests as DVT, with one-third manifesting as PE.
:A more recent source would be:Ortel TL, Neumann I, Ageno W, Beyth R, Clark NP, Cuker A; et al. (2020)."American Society of Hematology 2020 guidelines for management of venous thromboembolism: treatment of deep vein thrombosis and pulmonary embolism".Blood Adv.4(19): 4693–4738.doi:10.1182/bloodadvances.2020001830.PMC7556153.PMID33007077.{{cite journal}}:CS1 maint: multiple names: authors list (link).To be more specific, it should read "About two-thirds of VTE manifests as DVT without PE; one-third manifests as PE (with or without DVT).- Done,good point
Up to one-forth of PE cases cause sudden death
:I would move this to to the PE section of Signs and symptoms. More recent source same as above.- That makes sense.Done
The next paragraph could begin with a phrasing like "DVT is classified as provoked etc", and later "It is also classified as acute...", to better justify the title of the section.I see your point. That makes sense. Although, my current thinking on the section is that I'm trying to classify DVT as a diagnosis in relation to other diagnoses, such as PE, VT (venous thrombosis), and VTE for readers. I currently think this section is the best spot for it but hmmmm... Maybe put it at the beginning of the epidemiology section?Biosthmors(talk)23:11, 22 April 2021 (UTC)- I think I originally misunderstood what you were saying. The second paragraph in this section now begins like this.Biosthmors(talk)19:55, 8 May 2021 (UTC)
Ortel (2020) could be used for the definition of provoked and unprovoked DVT, as more recent. On provoked and unprovoked DVT, one could add "This distinction has important implications to therapy".- Interestingly, while looking at newer sources for this I ran across[6]leading me to find "Terminology such as ‘provoked’ vs. ‘unprovoked’ PE/VTE is no longer supported by the Guidelines, as it is potentially misleading and not helpful for decision-making regarding the duration of anticoagulation."[7](2019 ESC) Perhaps that's a minority opinion but it does seem to be a bit of a trend. The first paper cited in this comment cites at least 1 other paper making the argument to move away from this terminology. I'm not yet sure what to make of this, because the article (and other sources) still do use these terms a good bit.Biosthmors(talk)00:36, 24 April 2021 (UTC)
- Excellent point, I wish I had noticed it myself. It makes little difference if the actual term "provoked" is used; in light of this source though, I rather prefer omitting the concept from Classification and mentioning it under Management (in the context of anticoagulation duration). But I have no strong feelings, no solution is wrong.NikosGouliaros(talk)10:09, 24 April 2021 (UTC)
- I have currently opted to discuss it in the last paragraph of the Classifications section by citing the paper that mentions the 2019 ESC opinion.Biosthmors(talk)19:57, 8 May 2021 (UTC)
- Excellent point, I wish I had noticed it myself. It makes little difference if the actual term "provoked" is used; in light of this source though, I rather prefer omitting the concept from Classification and mentioning it under Management (in the context of anticoagulation duration). But I have no strong feelings, no solution is wrong.NikosGouliaros(talk)10:09, 24 April 2021 (UTC)
- Interestingly, while looking at newer sources for this I ran across[6]leading me to find "Terminology such as ‘provoked’ vs. ‘unprovoked’ PE/VTE is no longer supported by the Guidelines, as it is potentially misleading and not helpful for decision-making regarding the duration of anticoagulation."[7](2019 ESC) Perhaps that's a minority opinion but it does seem to be a bit of a trend. The first paper cited in this comment cites at least 1 other paper making the argument to move away from this terminology. I'm not yet sure what to make of this, because the article (and other sources) still do use these terms a good bit.Biosthmors(talk)00:36, 24 April 2021 (UTC)
Acute DVT is characterized by pain and swelling and is usually occlusive, which means that it obstructs blood flow, whereas non-occlusive DVT is less symptomatic.
:The distinction between occlusive and non-occlusive DVT is self-evident, and seems to attract little attention in literature; I haven't been able to find a direct mention in it in a source more recent than the two cited ones [Scarvelis (2009) quotes a 1992 paper}. I propose deleting this sentence (but this is getting outside my field of expertise, so my proposal is weak).NikosGouliaros(talk)17:55, 19 April 2021 (UTC)(To be continued)- I have removed the text that mentions of occlusive vs. non-occlusive.
Acute DVT is characterized by pain and swelling
remains.Biosthmors(talk)00:45, 24 April 2021 (UTC)- And even that is gone now.Biosthmors(talk)20:08, 8 May 2021 (UTC)
- I have removed the text that mentions of occlusive vs. non-occlusive.
Comments from Axl
editFrom the lead section, paragraph 3: "Asian, Asian-American, Native American, and Hispanic individuals have a lower VTE risk than whites or Blacks."The word" whites "has lower case while" Blacks "has upper case. Is this correct?Axl¤[Talk]18:25, 27 April 2021 (UTC)- Good question. I was following the NYT style guide,[8](based on a 2020 decision). The 2016 sources cited do not do this. I see atBlack peoplesome do and some do not do this. I do not yet know if there is a trend in the medical literature.Biosthmors(talk)22:26, 27 April 2021 (UTC)
- It appears the CDC and the AMA[9]are consistent in their capitalization of bothWhiteandBlack.The NYT, on the other hand, says this about their decision: "white doesn’t represent a shared culture and history in the way Black does, and also has long been capitalized by hate groups." I'd be interested to know what happens in other countries, as all of this is US-centric.Biosthmors(talk)23:33, 27 April 2021 (UTC)
- It looks like both BMJ and the NEJM opt for capitalizing both words, so I guess I'll follow their lead. Will change.Biosthmors(talk)01:23, 28 April 2021 (UTC)
- Thank you for addressing this point. However please don't
strikethroughmy questions. I shall do so myself when I am happy that the matter is resolved.Axl¤[Talk]09:25, 28 April 2021 (UTC)- Noted, sorry about that. Thanks for prompting me to dig deeper on this style point.Biosthmors(talk)11:41, 28 April 2021 (UTC)
- Thank you for addressing this point. However please don't
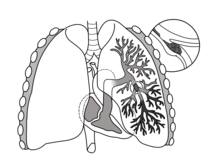
This diagram showing pulmonary embolism is in "Signs and symptoms", subsection "Acute complications". Overall, the heart is too small and the trachea is a little too short. The top of the heart should be closer to the carina (where the trachea branches into the two main bronchi). Also, the arch of the aorta should pass over the left main bronchus. I realise that this diagram is intended to portray pulmonary embolism, not the anatomical relationship between the heart and lungs, so maybe this is only a minor point. It might be helpful if there was an arrow on the diagram to indicate the PE.
- Perhaps the best solution might be to contact the original artist of the diagram and ask for a correction?Axl¤[Talk]10:03, 29 April 2021 (UTC)
- I havedone so,thanks.Biosthmors(talk)17:00, 29 April 2021 (UTC)
- Went ahead andreplacedthe image for now.Biosthmors(talk)23:29, 2 May 2021 (UTC)
Comments by Spicy
editI was asked to take a look at this on my talk page. I'm not well-versed in the topic & have only had a cursory look at the article - these comments are mostly from a prose perspective.
- Lead
Also, recurrent VTE occurs in about 30% of those in the ten years following an initial VTE
- I'd remove "also" - seeUser:Tony1/How_to_improve_your_writing#Eliminating_redundancy- Done, thanks for the link
An estimated 4–10% of DVTs affect the arms.
- this sentence seems a bit out of place; would it fit better after "...most commonly in the legs or pelvis."?- Done, that suggestion makes sense
Data has been historically dominated by European and North American populations,
- this sentence is a bit ambiguous; are you saying that DVT is understudied in non-European and North American populations, or just that it occurs more commonly in Europeans and North Americans?- Removed from the lead for now. Zakai and McClure (2011) state "VTE results from a complex interplay between genetic and environmental risk factors, which are poorly studied in non-European populations and outside of North America and Europe." I am trying to state that DVT was (more than is) understudied in non-European and North American populations, nodding to the fact that the source is 10 years old and that science has presumably progressed since then. That said, I can see that this sort of nuanced "fact", which also rests on an assumption that science has progressed, isn't really suited for a high-level summary that is supposed to be the lead. I was also trying to hint that the preceding sentence (When compared to those aged 40 and below, people aged 65 and above are at an approximate 15 times higher risk) might not be from a population that mimics the global population. I have already commented out this sort of content from the body of the article, however, because it read as outdated.
- Signs and symptoms
Yet, the signs and symptoms are highly variable
- can remove 'yet'- Done, withtweaksto sentence order and flow
- It may be useful to briefly explain the difference between SVT and DVT
- Done
a blue or purplish discoloration (cyanosis)
- probably best to explain the term at its first occurence ('cyanosis with fever')- Done
- Classification
- linkproximalanddistal?
- Done
Upper extremity DVT occurs in the arms or the base of the neck.
- inline ref?- Removed sentence for now, doesn't seem informative enough to include
- linkEuropean Society of Cardiology?
- Done. In that same edit I inserted an editorial note asking if I should aggressively simplify a paragraph FYI[10]
- I don't think the paragraph is too complex as it is, though IMO either option is probably fine.Spicy(talk)19:06, 4 August 2021 (UTC)
- Done. In that same edit I inserted an editorial note asking if I should aggressively simplify a paragraph FYI[10]
- Causes
Infections, including sepsis, COVID-19, HIV, and active tuberculosis, increase risk.
- Do *all* infections increase risk, e.g. a cold or a yeast infection?- One cited source says "All types of infection can elevate risk, although some appear to increase risk more than others. Thus, augmented risk of venous thromboembolism is observed in cases of pneumonia (OR, 3.6), symptomatic urinary tract (OR, 2.2), oral (periodontitis and gingivitis–OR, 12), intra-abdominal (OR, 18), and systemic/bloodstream infections (with or without laboratory-confirmed culture–OR, 11–21) (1–3, 6)."[11]In general, reliable sources say infection is a risk factor. This includes a recent seminar inThe LancetI plan to incorporate into the article:Khan F, Tritschler T, Kahn SR, Rodger MA (May 2021). "Venous thromboembolism".The Lancet.doi:10.1016/S0140-6736(20)32658-1.PMID33984268..Like you, however, I do wonder if in fact some infections, like a minor cold, might not increase DVT risk, but I haven't seen reliable sources express this doubt. The infections I highlight by name are ones that have stood out in the literature and are major global causes of morbidity and mortality, so I thought they were worth mentioning separately.
- Interesting, thanks for clarifying.Spicy(talk)19:06, 4 August 2021 (UTC)
- One cited source says "All types of infection can elevate risk, although some appear to increase risk more than others. Thus, augmented risk of venous thromboembolism is observed in cases of pneumonia (OR, 3.6), symptomatic urinary tract (OR, 2.2), oral (periodontitis and gingivitis–OR, 12), intra-abdominal (OR, 18), and systemic/bloodstream infections (with or without laboratory-confirmed culture–OR, 11–21) (1–3, 6)."[11]In general, reliable sources say infection is a risk factor. This includes a recent seminar inThe LancetI plan to incorporate into the article:Khan F, Tritschler T, Kahn SR, Rodger MA (May 2021). "Venous thromboembolism".The Lancet.doi:10.1016/S0140-6736(20)32658-1.PMID33984268..Like you, however, I do wonder if in fact some infections, like a minor cold, might not increase DVT risk, but I haven't seen reliable sources express this doubt. The infections I highlight by name are ones that have stood out in the literature and are major global causes of morbidity and mortality, so I thought they were worth mentioning separately.
- linkhomozygous?
- Done
- Management
warfarin only therapy.
- should be 'warfarin-only'- Done
- may want to explain what the INR is measuring
- I agree an explainer would be useful for readers, soI added a footnotefrom an introductory-level source
- linkstatins?
- Done
- Prevention
Avoiding smoking and a Western pattern diet is also thought to reduce risk.
- ambiguous; are you saying "a Western pattern diet is also thought to reduce risk" or "Avoiding... a Western pattern diet is also thought to reduce risk"?- Clarified by adding "Avoiding both...", thanks
Low-molecular-weight heparin is usually given by subcutaneous injections with a needle under the skin of these colored areas
- source? (yes, this is obvious, but it isn'tWP:SKYISBLUEterritory for the average reader)- Despite it being kind of obvious, saying "these colored areas", is a synthesis of sources and unlikely to be found it just one source, so I've removed it for now. After all, this image is more related to subcutaneous injections than VTE itself.
Warfarin, a common VKA
- acronym isn't previously explained- Expanded to "vitamin K antagonist"
- Epidemiology
About 1.5 out of 1000 adults a year have a first VTE in high-income countries,[163][164] with it becoming much more common with age.[58]
- seeUser:Tony1/Noun_plus_-ing;could be rephrased as '...in high-income countries. The condition becomes much more common with age'. or similar- Done, thank you
Acute VTE occurs about 1.2 of 1000 deliveries.
- occurs in?- Done, good catch
- linkMaternal mortality?
- Done
- Social
NBC journalist David Bloom died at age 39 while covering the Iraq War from a PE that was thought to have progressed from a missed DVT.[180] And actor Jimmy Stewart had DVT
- should be a comma- Done
- the 'Field of medicine' subsection seems a bit out of place here; might work better if integrated into 'Management'
- Done
The bookSushruta Samhita
- book titles should be italicized- Done
To avoid the blood monitoring required with warfarin and the injections required by heparin and heparin-like medicines, a new generation of oral anticoagulant pills that do not require blood monitoring
- redundant... you've already said that they don't require monitoring- Reworded
making this field of medicine fast changing.
- seems a bit awkward and unencyclopedic, I think you could drop this and be fine- Done
VTE costs the U.S. healthcare system
- elsewhere in the article you haveFormer US President
,seeMOS:US- Thanks, now consistent
- General
- See also sections are also frowned upon at FAC - ideally a FA should be comprehensive and should already contain whatever links are in the 'see also' section. I don't think these topics are directly relevant enough to be covered in the main text - but that means they're probably not worth including in the 'see also' section either. Consider adding{{Bleeding and clotting disorders}}instead?
- Thanks. Upon further research and thinking, I decided to remove 3 links and subsume the other two.Linkto the final edit that did away with the see also section
- Notes a and b probably need refs
- All notes have refs now
- Do we need an external link to a Wells score calculator? Seems like verging on giving medical advice
- Removed
- Some images lack alt text
- Thanks, work continues on this as of mid-July (I'm back to being busy in real life again)
- Not a formal image review, but I checked out the licensing on the images. Most are fine.ticket:2013061010006654forFile:Blausen_0290_DeepVeinThrombosis.pngappears valid.
- Minor point, but the descriptions onFile:2136ab_Lower_Limb_Veins_Anterior_Posterior.jpgandFile:2134_Thoracic_Upper_Limb_Veins.jpgsay they're licensed under CC-BY-3.0 while thesourcesays it's CC-BY-4.0.
- File:Rudolf Virchow older portrait.jpgneeds proof that it was *published* (not taken) before 1926.
- To potentially get around this issue, I did see that the CDC has a photo quiz published on Virchow that is marked as public domain[12](then go to the supporting files tab and the DS3.jpeg file is nice). Granted, I suppose it would be nicer to have whichever picture of Virchow was taken closest to the time that he had his work published that gave rise to the triad. But at least that picture to be public domain. Can we rely on the fact the CDC published it, instead of having to go dig around for the publication date of the primary source?User:Spicy,I thought I'd go ahead and ping you to make sure you saw this question. Thank you very much for all of your comments!! I found them very helpful.Biosthmors(talk)22:59, 31 July 2021 (UTC)
- I've now found a higher quality image than the one the CDC published that is sourced to the NIH:https://commons.wikimedia.org/wiki/File:Rudolf_Virchow-cropped.jpgHowever, I guessing we're back to the original issue. Do we still need proof it was *published* before 1926? That sounds difficult / complicated but maybe it's not.Biosthmors(talk)23:21, 31 July 2021 (UTC)
- Well, the NIH source does state 'The National Library of Medicine believes this item to be in the public domain' (archive link). I'm notentirelysure that will hold up at FAC, but it's better than nothing.Spicy(talk)19:06, 4 August 2021 (UTC)
- I haven't had time to look at the references yet.
My overall impression is that the article is quite comprehensive and well-written. My comments are mostly nitpicking.Spicy(talk)17:25, 16 May 2021 (UTC)
Sorry for the delayed reply. You have been doing incredible work on this article... a few more comments:
- The anatomical diagrams in the pathophysiology section aresandwichingand one of them doesn't have a caption. I think these might work better if formatted with the
{{Multiple images}}template and downscaled somewhat. - What makes[13]a high-quality MEDRS source?
- A single laboratory's test catalogue[14]isn't a great source either and the exact cutoff level can vary. For example, one of my textbooks (Rodak's Hematology, 2017) gives an upper limit of 240 ng/mL. I don't think the explanatory note about normal ranges is even necessary, really.
- From a glance at the reference section most other citations appear to be from appropriate MEDRS sources. There are a few older and lower-quality sources but they only seem to be supporting basic and uncontroversial information or historical items.
- There has been some debate at FAC over whether or not long journal articles (>10 pages or so) should have specific page numbers cited. Whether or not someone brings this up at FAC will probably depend on who shows up.*shrug*Spicy(talk)19:06, 4 August 2021 (UTC)
Comments from Cas Liber
editLooks promising...queries below:
- An estimated 4–10% of DVTs affect the arms- sounds like ones in legs can reach the arms....I'd say "An estimated 4–10% of DVTs occur in the arms"
- Changed
- The mechanism of clot formation typically involves some combination of decreased blood flow rate, increased tendency to clot,- reads funny with the two "clots" in the one sentence.
- Reworded
- When compared to those aged 40 and below, people aged 65 and above are at an approximate 15 times higher risk.- smoothe out as, "people aged 65 and above have an approximately 15 times greater risk than those aged under 40."
- Done
- but in the lower limbs of those who are not able to walk, these symptoms might not manifest- flip these clauses as sounds awkward
- Done
more later
Comments from jfdwolff
editSome comments, with many apologies for the late response:
- General comments:
- I think UEDVT and other rare forms of thrombosis should be distinguished right from the start and not discussed further. DVT without a modifier is leg & pelvis. This would remove the need for the confusing discussion about SVCO in UEDVT in the "signs and symptoms" section. Currently there is no article about UEDVT as a whole, onlyPaget–Schroetter disease.
- Lead section:
- I firmly believe that "blood thinners" is an undesirable imprecise colloquialism. I think "anticoagulants ('blood thinners')" is borderline acceptable.
- Unsure why only apixaban and rivaroxaban are mentioned, where edoxaban and dabigatran are licensed in many countries for VTE (with heparin bridging on initiation).
- Signs and symptoms:
- Under "differential diagnosis", I have never heard of "muscle vein thrombosis" and it seems odd that this would be a distinct pathology from DVT.
- Similarly "connective tissue disorders" without any further information strikes me as completely uninformative because this group of diseases usually affects multiple parts of the body. Why would it cause symptoms similar to a DVT?
- Classification:
- "Differences between these two types of DVT can be seen with ultrasound" is not entirely precise. Ultrasound can't always distinguish, and there is an expanding literature on the use of MRDTI. At any rate, why is this in "classification" and not in "diagnosis"?
- Causes:
- There is a good deal of overlap between "Causes" and "Pathophysiology". Some rebalancing is needed, e.g. "Virchow's triad" should be under "pathophysiology" and not "causes".
- Lower limb amputation as a risk factor: undoubtedly true but worth explaining what that means in practice ( "thrombosis in an amputated limb" ). Does it really need to mentioned if reported in a single source?
- "Solid tumors such as adenocarcinomas can contribute to both VTE and disseminated intravascular coagulation": this is factual but also possibly beyond the scope of the article. DIC is not easy to understand for the average reader and may discharge from the flow of this section.
- "fibrinogen gamma gene variant rs2066865" - this is based on a primary source that is only about cancer. Consider removing this association as relatively weak.
- Pathophysiology:
- See under "Causes"
- Treatment
- "A 2018 study associated IVC filter placement with a 50% reduction in PE, a 70% increase in DVT, and an 18% increase in 30 day mortality when compared to no IVC placement." Is there sufficient reason to provide the results of a primary research study?
Happy to comment further.JFW|T@lk14:31, 1 August 2021 (UTC)
References
editReferences
- ^Goldhaber, SJ (2019). "Chapter 84: Pulmonary Embolism". In Zipes, DP; Libby, P; Bonow, RO; Mann, DL; Tomaselli, GM; Braunwald, E (eds.).Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine(11th ed.). Elsevier. pp. 1681–1698.ISBN978-0-323-46342-3.
- ^Mazzolai L, Aboyans V, Ageno W, Agnelli G, Alatri A, Bauersachs R, et al. (December 2018)."Diagnosis and management of acute deep vein thrombosis: a joint consensus document from the European Society of Cardiology working groups of aorta and peripheral vascular diseases and pulmonary circulation and right ventricular function".European Heart Journal.39(47): 4208–4218.doi:10.1093/eurheartj/ehx003.PMID28329262.
- ^abcdLeBlond, RF; DeGowin, RL; Brown, DD (2009).DeGowin's Diagnostic Examination(9th ed.). McGraw-Hill. pp. 430–431.ISBN978-0-07-147898-4.
- ^abcCreager, MA; Dzau, VJ (2005). "Chapter 232: Vascular Diseases of the Extremities". In Kasper, DE; Braunwald, E; Fauci, AS; Hauser, SL; Longo, DL; Jameson, JL (eds.).Harrison's Principles of Internal Medicine(16th ed.). McGraw-Hill. pp. 1486–1494.ISBN0-07-139140-1.
- ^Gardella, L; Faulk, JB (2020),"Phlegmasia Alba And Cerulea Dolens",StatPearls,Treasure Island (FL): StatPearls Publishing,PMID33085284,retrieved2021-04-18
- ^abLloyd NS, Douketis JD, Moinuddin I, Lim W, Crowther MA (March 2008)."Anticoagulant prophylaxis to prevent asymptomatic deep vein thrombosis in hospitalized medical patients: a systematic review and meta-analysis".Journal of Thrombosis and Haemostasis.6(3): 405–14.doi:10.1111/j.1538-7836.2007.02847.x.PMID18031292.