Insulin (medication)
 Vials ofinsulin | |
| Clinical data | |
|---|---|
| Trade names | Humulin, Novolin, Insuman, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682611 |
| License data | |
| Routes of administration | Subcutaneous,intravenous,intramuscular,inhalation |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| CAS Number | |
| PubChemCID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| Chemical and physical data | |
| Formula | C257H383N65O77S6 |
| Molar mass | 5807.63g·mol−1 |
| Density | 1.09 g/cm3[4] |
| Melting point | 233 °C (451 °F)[5] |
As amedication,insulinis anypharmaceuticalpreparation of the protein hormoneinsulinthat is used to treathigh blood glucose.[6]Such conditions includetype 1 diabetes,type 2 diabetes,gestational diabetes,and complications ofdiabetessuch asdiabetic ketoacidosisandhyperosmolar hyperglycemic states.[6]Insulin is also used along withglucoseto treathyperkalemia(high blood potassium levels).[7]Typically it is given byinjection under the skin,but some forms may also be used byinjection into a veinormuscle.[6]There are various types of insulin, suitable for various time spans. The types are often all calledinsulinin the broadsense,although in a more precise sense, insulin is identical to the naturally occurring molecule whereasinsulin analogueshave slightly different molecules that allow for modified time of action. It is on theWorld Health Organization's List of Essential Medicines.[8]In 2021, it was the 179th most commonly prescribed medication in the United States, with more than 2million prescriptions.[9][10]
Insulin can be made from thepancreasof pigs or cows.[11]Human versions can be made either by modifying pig versions, orrecombinant technology[11]using mainlyE. coliorSaccharomycescerevisiae.[12]It comes in three main types: short–acting (such asregular insulin), intermediate-acting (such asneutral protamine Hagedorn(NPH) insulin), and longer-acting (such asinsulin glargine).[11]
History
[edit]Insulin was first used as a medication in Canada byCharles BestandFrederick Bantingin 1922.[13][14]
This is a chronology of key milestones in the history of the medical use of insulin. For more details on the discovery, extraction, purification, clinical use, and synthesis of insulin, seeInsulin
- 1921 Research on the role of pancreas in the nutritive assimilation[15]
- 1922Frederick Banting,Charles BestandJames Collipuse bovine insulin extract in humans atConnaught Laboratoriesin Toronto, Canada.[13]
- 1922Leonard Thompsonbecomes the first human to be treated with insulin.
- 1922James D. Havens,son of former congressmanJames S. Havens,becomes the first American to be treated with insulin.[16][17]
- 1922Elizabeth Hughes Gossett,daughter of the US Secretary of State, becomes the first American to be (officially) treated in Toronto.[18][19]
- 1923Eli Lillyproduces commercial quantities of much purer bovine insulin than Banting et al. had used
- 1923 FarbwerkeHoechst,one of the forerunners of today'sSanofi Aventis,produces commercial quantities of bovine insulin in Germany
- 1923Hans Christian Hagedornfounds the Nordisk Insulinlaboratorium in Denmark – forerunner of today'sNovo Nordisk
- 1923Constance Collierreturns to health after being successfully treated with insulin in Strasbourg[20]
- 1926Nordiskreceives a Danish charter to produce insulin as a non-profit
- 1936 Canadians David M. Scott and Albert M. Fisher formulate a zinc insulin mixture atConnaught Laboratoriesin Toronto and license it toNovo
- 1936 Hagedorn discovers that adding protamine to insulin prolongs the duration of action of insulin
- 1946 Nordisk formulates Isophane porcine insulin aka Neutral Protamine Hagedorn orNPH insulin
- 1946 Nordisk crystallizes a protamine and insulin mixture
- 1950 Nordisk marketsNPH insulin
- 1953 Novo formulates Lente porcine and bovine insulins by adding zinc for longer lasting insulin
- 1955Frederick Sangerdetermines theamino acid sequenceof insulin
- 1965 Synthesized by total synthesis byWang Yinglai,Chen-Lu Tsou,et al.
- 1969Dorothy Crowfoot Hodgkincharacterizes and describes the crystal structure of insulin byX-ray crystallography
- 1973 Purified monocomponent (MC) insulin is introduced
- 1973 The US officially "standardized" insulin sold for human use in the US to U-100 (100 units per milliliter). Prior to that, insulin was sold in different strengths, including U-80 (80 units per milliliter) and U-40 formulations (40 units per milliliter), so the effort to "standardize" the potency aimed to reduce dosage errors and ease doctors' job of prescribing insulin for people. Other countries also followed suit.
- 1978Genentechproduces biosynthetic human insulin inEscherichia colibacteria using recombinant DNA techniques, licenses to Eli Lilly
- 1981Novo Nordiskchemically and enzymatically converts porcine to human insulin
- 1982Genentechsynthetic human insulin (above) approved
- 1983Eli Lilly and Companyproduces biosynthetic human insulin withrecombinant DNAtechnology, Humulin
- 1985Axel Ullrichsequences a human cell membrane insulin receptor.
- 1988Novo Nordiskproduces recombinant biosynthetic human insulin
- 1996LillyHumalog "lispro" insulin analogue approved.
- 2000Sanofi AventisLantus insulin "glargine" analogue approved for clinical use in the US and the EU.
- 2004Sanofi AventisApidra insulin "glulisine" insulin analogue approved for clinical use in the US.
- 2006Novo NordiskLevemir"detemir" insulin analogue approved for clinical use in the US.
- 2008Abott laboratories"FreeStyle Navigator CGM" gets approved.[21]
- 2013 The USFood and Drug Administration(FDA) requested more cardiac safety tests forInsulin degludec.
- 2015Insulin degludecwas approved by the FDA in September 2015.
Medical uses
[edit]


Insulin is used to treat a number of diseases includingdiabetesand its acute complications such asdiabetic ketoacidosisandhyperosmolar hyperglycemic states.It is also used along withglucoseto treathigh blood potassium levels.Use duringpregnancyis relatively safe for the baby.[6]Insulin was formerly used in a psychiatric treatment calledinsulin shock therapy.[22]
Side effects
[edit]Some side effects arehypoglycemia(low blood sugar),hypokalemia(low blood potassium), andallergic reactions.[6]Allergy to insulin affected about 2% of people, of which most reactions are not due to the insulin itself but to preservatives added to insulin such as zinc,protamine,andmeta-cresol.Most reactions areType I hypersensitivityreactions and rarely causeanaphylaxis.A suspected allergy to insulin can be confirmed byskin prick testing,patch testingand occasionallyskin biopsy.First line therapy against insulin hypersensitivity reactions include symptomatic therapy with antihistamines. The affected persons are then switched to a preparation that does not contain the specific agent they are reacting to or undergodesensitization.[23]
Cutaneous adverse effects
Other side effects may include pain or skin changes at the sites of injection. Repeated subcutaneous injection without site rotation can lead tolipohypertrophyand amyloidomas, which manifest as firm palpable nodules under the skin.[24]
Effects of early routine use
[edit]Early initiation of insulin therapy for the long-term management of conditions such as type 2 diabetes would suggest that the use of insulin has unique benefits, however, with insulin therapy, there is a need to gradually raise the dose and the complexity of the regimen, as well as the likelihood of developing severe hypoglycemia which is why many people and their doctors are hesitant to begin insulin therapy in the early stage of disease management.[25]Many obstacles associated with health behaviors also prevent people with type 2 diabetes mellitus from starting or intensifying their insulin treatment, including lack of motivation, lack of familiarity with or experience with treatments, and time restraints causing people to have high glycemic loads for extended periods of time prior to starting insulin therapy. This is why managing the side effects associated with long-term early routine use of insulin for type 2 diabetes mellitus can prove to be a therapeutic and behavioral challenge.[26]
Principles
[edit]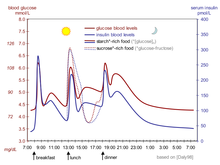
| Amino Acid Sequence of Insulin Preparations[27][28] | |||||||
|---|---|---|---|---|---|---|---|
| Amino Acid Substitutions | |||||||
|
|
A-Chain Position |
B-Chain Position | |||||
| Source Species |
A-8 | A-10 | A-21 | B-28 | B-29 | B-30 | B-31 B-32 |
| Bovine | Ala | Val | Asn | Pro | Lys | Ala | N/A |
| Porcine | Thr | Ile | Asn | Pro | Lys | Ala | N/A |
| Human | Thr | Ile | Asn | Pro | Lys | Thr | N/A |
| Aspart(Novolog) | Thr | Ile | Asn | Asp | Lys | Thr | N/A |
| Lispro(Humalog) | Thr | Ile | Asn | Lys | Pro | Thr | N/A |
| Glulisine(Apidra) | Thr | Ile | Asn | Pro | Glu | Thr | N/A |
| Glargine(Lantus) | Thr | Ilc | Gly | Pro | Lys | Thr | Arg |
| Detemir(Levemir) | Thr | Ile | Asn | Pro | Lys | N/A | Myristic acid |
| Degludec(Tresiba) | Thr | Ile | Asn | Pro | Lys | N/A | Hexadecanedioic acid |
|
Ala=Alanine Val=Valine Asn=Asparagine Pro=Proline Lys=Lysine Thr=Threonine Ile=Isoleucine Glu=Glutamine Gly=Glycine
| |||||||
Insulin is anendogenoushormone,which is produced by thepancreas.[29] The insulinproteinhas been highly conserved across evolutionary time, and is present in bothmammalsandinvertebrates.The insulin/insulin-like growth factorsignalling pathway (IIS) has been extensively studied in species including nematode worms (e.g.C. elegans), flies (Drosophila melanogaster) and mice (Mus musculus). Its mechanisms of action are highly similar across species.[30]
Bothtype 1 diabetesandtype 2 diabetesare marked by a loss of pancreatic function, though to differing degrees.[29]People who are affected with diabetes are referred to as diabetics. Many diabetics require an exogenous source of insulin to keep their blood sugar levels within a safe target range.[31][32][33]
In 1916, Nicolae C. Paulescu (1869–1931) succeeded in developing an aqueous pancreatic extract that normalized a diabetic dog. In 1921, he published 4 papers in the Society of Biology in Paris centering on the successful effects of the pancreatic extract in diabetic dogs. Research on the Role of the Pancreas in Food Assimilation by Paulescu was published in August 1921 in the Archives Internationales de Physiologie, Liège, Belgium. Initially, the only way to obtain insulin for clinical use was to extract it from the pancreas of another creature. Animal glands were obtainable as a waste product of the meatpacking industry. Insulin was derived primarily fromcows(Eli Lilly and Company) andpigs(Nordisk Insulinlaboratorium). The making of eight ounces of purified insulin could require as much as two tons of pig parts.[34][35][36]Insulin from these sources is effective in humans as it is highly similar to human insulin (three amino acid difference in bovine insulin, one amino acid difference in porcine).[36]Initially, lower preparation purity resulted in allergic reactions to the presence of non-insulin substances. Purity has improved steadily since the 1920s ultimately reaching purity of 99% by the mid-1970s thanks tohigh-pressure liquid chromatography(HPLC) methods. Minor allergic reactions still occur occasionally, even to synthetic "human" insulin varieties.[36]
Beginning in 1982, biosynthetic "human" insulin has been manufactured for clinical use through genetic engineering techniques usingrecombinant DNAtechnology.Genentechdeveloped the technique used to produce the first such insulin, Humulin, but did not commercially market the product themselves.Eli Lillymarketed Humulin in 1982.[37]Humulin was the first medication produced using modern genetic engineering techniques in which actual human DNA is inserted into a host cell (E. coliin this case). The host cells are then allowed to grow and reproduce normally, and due to the inserted human DNA, they produce a synthetic version of human insulin. Manufacturers claim this reduces the presence of many impurities. However, the clinical preparations prepared from such insulins differ from endogenous human insulin in several important respects; an example is the absence ofC-peptidewhich has in recent years been shown to have systemic effects itself. Novo Nordiskhas also developed a genetically engineered insulin independently using a yeast process.[38][39]
According to a survey that the International Diabetes Federation conducted in 2002 on the access to and availability of insulin in its member countries, approximately 70% of the insulin that is currently sold in the world is recombinant, biosynthetic 'human' insulin.[40]A majority of insulin used clinically today is produced this way, although clinical experience has provided conflicting evidence on whether these insulins are any less likely to produce an allergic reaction. Adverse reactions have been reported; these include loss of warning signs that patients may slip into a coma throughhypoglycemia,convulsions, memory lapse and loss of concentration.[41]However, the International Diabetes Federation's position statement from 2005 is very clear in stating that "there is NO overwhelming evidence to prefer one species of insulin over another" and "[modern, highly purified] animal insulins remain a perfectly acceptable alternative."[42]
Since January 2006, all insulins distributed in the US and some other countries are synthetic "human" insulins or their analogues. A special FDA importation process is required to obtain bovine or porcine derived insulin for use in the US,[43]although there may be some remaining stocks of porcine insulin made by Lilly in 2005 or earlier, and porcinelente insulinis also sold and marketed under the brand name Vetsulin(SM) in the US for veterinary usage in the treatment of companion animals with diabetes.[44]
Basal insulin
[edit]In type 1 diabetes, insulin production is extremely low, and as such the body requiresexogenousinsulin. Some people with type 2 diabetes, particularly those with very highhemoglobin A1cvalues, may also require a baseline rate of insulin, as their body is desensitized to the level of insulin being produced. Basal insulin regulates the body's blood glucose between mealtimes, as well as overnight. This basal rate of insulin action is generally achieved via the use of an intermediate-acting insulin (such as NPH) or a long-acting insulin analog. In type 1 diabetics, it may also be achieved via continuous infusion of rapid-acting insulin using aninsulin pump.Approximately half of a person's daily insulin requirement is administered as a basal insulin, usually administered once per day at night.[45]
Prandial insulin
[edit]When a person eats food containing carbohydrates and glucose, insulin helps regulate the body's metabolism of the food. Prandial insulin, also called mealtime or bolus insulin, is designed as abolusdose of insulin prior to a meal to regulate the spike in blood glucose that occurs following a meal. The dose of prandial insulin may be static, or may be calculated by the patient using either their current blood sugar, planned carbohydrate intake, or both. This calculation may also be performed by an insulin pump in patients using a pump. Insulin regiments that consist of doses calculated in this manner are consideredintensive insulin regimens.[46]Prandial insulin is usually administered no more than 15–30 minutes prior to a meal using a rapid-acting insulin or a regular insulin. In some patients, a combination insulin may be used that contains both NPH (long acting) insulin and a rapid/regular insulin to provide both a basal insulin and prandial insulin.[45]
Challenges in treatment
[edit]There are several challenges involved in the use of insulin as a clinical treatment for diabetes:[47]
- Mode of administration.
- Selecting the 'right' dose and timing. The amount of carbohydrates one unit of insulin handles varies widely between persons and over the day but values between 7 and 20 grams per 1 IE is typical.
- Selecting an appropriate insulin preparation (typically on 'speed of onset and duration of action' grounds).
- Adjusting dosage and timing to fit food intake timing, amounts, and types.
- Adjusting dosage and timing to fit exercise undertaken.
- Adjusting dosage, type, and timing to fit other conditions, for instance the increased stress of illness.
- Variability in absorption into the bloodstream via subcutaneous delivery
- The dosage is non-physiological in that a subcutaneousbolusdose of insulin alone is administered instead of combination of insulin andC-peptidebeing released gradually and directly into theportal vein.
- It is simply a nuisance for people to inject whenever they eat carbohydrate or have a high blood glucose reading.
- It is dangerous in case of mistake (such as 'too much' insulin).
Types
[edit]Medical preparations of insulin are never just insulin in water (with nothing else). Clinical insulins are mixtures of insulin plus other substances including preservatives. These prevent the protein from spoiling ordenaturingtoo rapidly, delay absorption of the insulin, adjust the pH of the solution to reduce reactions at the injection site, and so on.[48]
Slight variations of the human insulin molecule are calledinsulin analogues,(technically "insulin receptorligands") so named because they are not technically insulin, rather they are analogues which retain the hormone's glucose management functionality. They have absorption and activity characteristics not currently possible with subcutaneously injected insulin proper. They are either absorbed rapidly in an attempt to mimic real beta cell insulin (as withinsulin lispro,insulin aspart,andinsulin glulisine), or steadily absorbed after injection instead of having a 'peak' followed by a more or less rapid decline in insulin action (as withinsulin detemirandinsulin glargine), all while retaining insulin's glucose-lowering action in the human body. However, a number ofmeta-analyses,including those done by theCochrane Collaborationin 2005,[49]Germany's Institute for Quality and Cost Effectiveness in the Health Care Sector [IQWiG] released in 2007,[50]and the Canadian Agency for Drugs and Technology in Health (CADTH)[51]also released in 2007 have shown no unequivocal advantages in clinical use of insulin analogues over more conventional insulin types.[50][51]
The commonly used types of insulin are as follows.[29]
Fast-acting (Rapid-acting)
[edit]Includes the insulin analoguesaspart,lispro,andglulisine.These begin to work within 5 to 15 minutes and are active for 3 to 4 hours. Most insulins formhexamers,which delay entry into the blood in active form; these analog insulins do not but have normal insulin activity. Newer varieties are now pending regulatory approval in the US which are designed to work rapidly, but retain the same genetic structure asregular human insulin.[52][53]
Short-acting
[edit]Includesregular insulin,which begins working within 30 minutes and is active about 5 to 8 hours.[54]
Intermediate-acting
[edit]IncludesNPH insulin,which begins working in 1 to 3 hours and is active for 16 to 24 hours.[55]
Long-acting
[edit]Includes the analoguesglargineU100 anddetemir,each of which begins working within 1 to 2 hours and continues to be active, without major peaks or dips, for about 24 hours, although this varies in many individuals.[56][57]
Ultra-long acting
[edit]Includes the analoguesinsulin glargineU300 anddegludec,which begin working within 30 to 90 minutes and continues to be active for greater than 24 hours.[28]
Combination insulin products
[edit]Includes a combination of either fast-acting or short-acting insulin with a longer-acting insulin, typically anNPH insulin.The combination products begin to work with the shorter-acting insulin (5–15 minutes for fast-acting, and 30 minutes for short-acting), and remain active for 16–24 hours. There are several variations with different proportions of the mixed insulins (e.g.Novolog Mix 70/30contains 70% aspart protamine [akin to NPH], and 30% aspart.)[58]
Methods of administration
[edit]
Unlike many medicines, insulin cannot be taken orally at the present time. Like nearly all other proteins introduced into thegastrointestinal tract,it is reduced to fragments (single amino acid components), whereupon all activity is lost. There has been some research into ways to protect insulin from the digestive tract, so that it can be administered in a pill. So far this is entirely experimental.[59]
Subcutaneous
[edit]Insulin is usually taken assubcutaneous injectionsby single-usesyringeswithneedles,aninsulin pump,or by repeated-useinsulin penswith needles. People who wish to reduce repeated skin puncture of insulin injections often use aninjection portin conjunction with syringes.[60]
The use of subcutaneous injections of insulin is designed to mimic the natural physiological cycle of insulin secretion, while taking into account the various properties of the formulations used such as half-life, onset of action, and duration of action. In many people, both a rapid- or short-acting insulin product as well as an intermediate- or long-acting product are used to decrease the amount of injections per day. In some, insulin injections may be combined with other injection therapy such asGLP-1 receptor agonists.Cleansing of the injection site and injection technique are required to ensure effective insulin therapy.[45]
Insulin pump
[edit]Insulin pumpsare a reasonable solution for some. Advantages to the person are better control over background orbasalinsulin dosage, bolus doses calculated to fractions of a unit, and calculators in the pump that may help with determiningbolusinfusion dosages. The limitations are cost, the potential for hypoglycemic and hyperglycemic episodes, catheter problems, and no "closed loop" means of controlling insulin delivery based on current blood glucose levels.[citation needed]
Insulin pumps may be like 'electrical injectors' attached to a temporarily implantedcatheterorcannula.Some who cannot achieve adequate glucose control by conventional (or jet) injection are able to do so with the appropriate pump.[61]
Indwelling catheters pose the risk of infection and ulceration, and some peoples may also developlipodystrophydue to the infusion sets. These risks can often be minimized by keeping infusion sites clean. Insulin pumps require care and effort to use correctly.[61]
Dosage and timing
[edit]Dosage units
[edit]Oneinternational unitof insulin (1 IU) is defined as the "biological equivalent" of 34.7μgpure crystalline insulin.[citation needed]
The first definition of a unit of insulin was the amount required to inducehypoglycemiain a rabbit. This was set byJames Collipat the University of Toronto in 1922. Of course, this was dependent on the size and diet of the rabbits. The unit of insulin was set by the insulin committee at the University of Toronto.[62]The unit evolved eventually to the oldUSPinsulin unit, where one unit (U) of insulin was set equal to the amount of insulin required to reduce the concentration ofblood glucosein afastingrabbitto 45mg/dL(2.5mmol/L). Once the chemical structure and mass of insulin was known, the unit of insulin was defined by the mass of pure crystalline insulin required to obtain the USP unit.[citation needed]
Theunit of measurementused in insulin therapy is not part of theInternational System of Units(abbreviated SI) which is the modern form of themetric system.Instead thepharmacologicalinternational unit(IU) is defined by theWHO Expert Committee on Biological Standardization.[63]
Potential complications
[edit]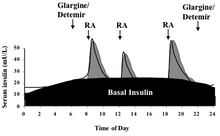
The central problem for those requiring external insulin is picking the right dose of insulin and the right timing.
Physiological regulation of blood glucose, as in the non-diabetic, would be best. Increased blood glucose levels after a meal is a stimulus for prompt release of insulin from the pancreas. The increased insulin level causes glucose absorption and storage in cells, reduces glycogen to glucose conversion, reducing blood glucose levels, and so reducing insulin release. The result is that the blood glucose level rises somewhat after eating, and within an hour or so, returns to the normal 'fasting' level. Even the best diabetic treatment with synthetic human insulin or even insulin analogs, however administered, falls far short of normal glucose control in the non-diabetic.[64]
Complicating matters is that the composition of the food eaten (seeglycemic index) affects intestinal absorption rates. Glucose from some foods is absorbed more (or less) rapidly than the same amount of glucose in other foods. In addition, fats and proteins cause delays in absorption of glucose from carbohydrates eaten at the same time. As well, exercise reduces the need for insulin even when all other factors remain the same, since working muscle has some ability to take up glucose without the help of insulin.[65]
Because of the complex and interacting factors, it is, in principle, impossible to know for certain how much insulin (and which type) is needed to 'cover' a particular meal to achieve a reasonable blood glucose level within an hour or two after eating. Non-diabetics' beta cells routinely and automatically manage this by continual glucose level monitoring and insulin release. All such decisions by a diabetic must be based on experience and training (i.e., at the direction of a physician, PA, or in some places a specialist diabetic educator) and, further, specifically based on the individual experience of the person. But it is not straightforward and should never be done by habit or routine. With some care however, it can be done reasonably well in clinical practice. For example, some people with diabetes require more insulin after drinkingskim milkthan they do after taking an equivalent amount of fat, protein, carbohydrate, and fluid in some other form. Their particular reaction to skimmed milk is different from other people with diabetes, but the same amount of whole milk is likely to cause a still different reaction even in that person. Whole milk contains considerable fat while skimmed milk has much less. It is a continual balancing act for all people with diabetes, especially for those taking insulin.[citation needed]
People with insulin-dependent diabetes typically require some base level of insulin (basal insulin), as well as short-acting insulin to cover meals (bolus also known as mealtime orprandialinsulin). Maintaining the basal rate and the bolus rate is a continuous balancing act that people with insulin-dependent diabetes must manage each day. This is normally achieved through regular blood tests, although continuous blood sugar testing equipment (Continuous Glucose Monitorsor CGMs) are now becoming available which could help to refine this balancing act once widespread usage becomes common.[citation needed]
Strategies
[edit]A long-acting insulin is used to approximate the basal secretion of insulin by the pancreas, which varies in the course of the day.[66]NPH/isophane, lente, ultralente, glargine, and detemir may be used for this purpose. The advantage of NPH is its low cost, the fact that you can mix it with short-acting forms of insulin, thereby minimizing the number of injections that must be administered, and that the activity of NPH will peak 4–6 hours after administration, allowing a bedtime dose to balance thetendency of glucose to rise with the dawn,along with a smaller morning dose to balance the lower afternoon basal need and possibly an afternoon dose to cover evening need. A disadvantage of bedtime NPH is that if not taken late enough (near midnight) to place its peak shortly before dawn, it has the potential of causing hypoglycemia. One theoretical advantage of glargine and detemir is that they only need to be administered once a day, although in practice many people find that neither lasts a full 24 hours. They can be administered at any time during the day as well, provided that they are given at the same time every day. Another advantage of long-acting insulins is that the basal component of an insulin regimen (providing a minimum level of insulin throughout the day) can be decoupled from the prandial or bolus component (providing mealtime coverage via ultra-short-acting insulins), while regimens using NPH and regular insulin have the disadvantage that any dose adjustment affects both basal and prandial coverage. Glargine and detemir are significantly more expensive than NPH, lente and ultralente, and they cannot be mixed with other forms of insulin.[citation needed]
A short-acting insulin is used to simulate the endogenous insulin surge produced in anticipation of eating. Regular insulin, lispro, aspart and glulisine can be used for this purpose. Regular insulin should be given with about a 30-minute lead-time prior to the meal to be maximally effective and to minimize the possibility of hypoglycemia. Lispro, aspart and glulisine are approved for dosage with the first bite of the meal, and may even be effective if given after completing the meal. The short-acting insulin is also used to correct hyperglycemia.[67]
Sliding scales
[edit]First described in 1934,[68]what physicians typically refer to as sliding-scale insulin (SSI) is fast- or rapid-acting insulin only, given subcutaneously, typically at meal times and sometimes bedtime,[69]but only when blood glucose is above a threshold (e.g. 10 mmol/L, 180 mg/dL).[70]The so-called "sliding-scale" method is widely taught, although it has been heavily criticized.[71][72][73][74]Sliding scale insulin (SSI) is not an effective way of managing long-term diabetes in individuals residing in nursing homes.[69][75]Sliding scale insulin leads to greater discomfort and increased nursing time.[75]
| before breakfast | before lunch | before dinner | at bedtime | |
|---|---|---|---|---|
| NPH dose | 12 units | 6 units | ||
| regular insulin dose if fingerstick glucose is (mg/dL) [mmol/L]: |
||||
| 70–100 [3.9–5.5] | 4 units | 4 units | ||
| 101–150 [5.6–8.3] | 5 units | 5 units | ||
| 151–200 [8.4–11.1] | 6 units | 6 units | ||
| 201–250 [11.2–13.9] | 7 units | 7 units | ||
| 251–300 [14.0–16.7] | 8 units | 1 unit | 8 units | 1 unit |
| >300 [>16.7] | 9 units | 2 units | 9 units | 2 units |
Sample regimen using insulin glargine and insulin lispro:
- Insulin glargine: 20 units at bedtime
| if fingerstick glucose is (mg/dL) [mmol/L]: |
before breakfast | before lunch | before dinner | at bedtime |
|---|---|---|---|---|
| 70–100 [3.9–5.5] | 5 units | 5 units | 5 units | |
| 101–150 [5.6–8.3] | 6 units | 6 units | 6 units | |
| 151–200 [8.4–11.1] | 7 units | 7 units | 7 units | |
| 201–250 [11.2–13.9] | 8 units | 8 units | 8 units | 1 unit |
| 251–300 [14.0–16.7] | 9 units | 9 units | 9 units | 2 units |
| >300 [>16.7] | 10 units | 10 units | 10 units | 3 units |
Insulin Medication in Pregnancy
[edit]During pregnancy, spontaneous hyperglycemia can develop and lead togestational diabetes mellitus (GDM),a frequent pregnancy complication. With a prevalence of 6-20% among pregnant women globally, gestational diabetes mellitus (GDM) is defined as any degree of glucose intolerance developing or initially recognized during pregnancy.[76]Neutral protamine Hagedorn(NPH) insulin has been the cornerstone of insulin therapy during pregnancy, administered two to four times per day. Women with GDM and pregnant women with type I diabetes mellitus who frequently check their blood glucose levels and utilize glucose monitoring equipment for doing so, use continuous insulin infusion of a rapid-acting insulin analogue, such aslisproandaspart.However, a number of considerations go into choosing a regimen for administering insulin to patients. When managing GDM in pregnant women, these guidelines are crucial and can vary depending on certain physiological and interestingly the sociocultural environment as well. The current perinatal guidelines recommend a low daily dose of insulin and take into account the woman's physiological features and the frequency of self-monitoring. The importance of using specialized insulin therapy planning based on parameters like those stated above rather than a broad approach is emphasized.[77]
Women with pre-existing diabetes have the highest levels of insulin sensitivity early in pregnancy. Close glucose monitoring is required to prevent hypoglycemia, which can potentially result in altered consciousness, seizures, and maternal damage.[78]Low birth weight newborns might also be the result of hypoglycemia, especially in patients with type 1 diabetes, because they are frequently more insulin sensitive than persons with type 2 diabetes and more likely to be unaware of their hypoglycemic state. Close glucose monitoring is essential because after 16 weeks of pregnancy, women with preexisting diabetes become more insulin resistant and their insulin demands may fluctuate weekly. The need for insulin may rise from one pregnancy to the next. Therefore, it is realistic to expect higher needs for glucose control with subsequent pregnancies in multiparous women.[78]
As a performance-enhancing drug
[edit]The possibility of using insulin in an attempt to improve athletic performance was suggested as early as the1998 Winter OlympicsinNagano, Japan,as reported byPeter Sönksenin the July 2001 issue ofJournal of Endocrinology.The question of whether non-diabetic athletes could legally use insulin was raised by a Russian medical officer.[79][80]Whether insulin would actually improve athletic performance is unclear, but concerns about its use led the International Olympic Committee to ban use of the hormone by non-diabetic athletes in 1998.[81]
The bookGame of Shadows(2001), by reporters Mark Fainaru-Wada and Lance Williams, included allegations that baseball playerBarry Bondsused insulin (as well as other drugs) in the apparent belief that it would increase the effectiveness of the growth hormone he was alleged to be taking.[82] Bonds eventually testified in front of a federal grand jury as part of a government investigation ofBALCO.[83]
Bodybuilders in particular are claimed to be using exogenous insulin and other drugs in the belief that they will increase muscle mass. Bodybuilders have been described as injecting up to 10IUof regular synthetic insulin before eating sugary meals.[81] A 2008 report suggested that insulin is sometimes used in combination withanabolic steroidsandgrowth hormone(GH), and that "Athletes are exposing themselves to potential harm by self‐administering large doses of GH, IGF‐I and insulin".[84][85] Insulin abuse has been mentioned as a possible factor in the deaths of bodybuilders Ghent Wakefield andRich Piana.[86]
Insulin, human growth hormone (HGH) and insulin-like growth factor 1 (IGF-1) are self-administered by those looking to increase muscle mass beyond the scope offered by anabolic steroids alone. Their rationale is that since insulin and HGH act synergistically to promote growth, and since IGF-1 is a primary mediator of musculoskeletal growth, the 'stacking' of insulin, HGH and IGF-1 should offer a synergistic growth effect on skeletal muscle. This theory has been supported in recent years by top-level bodybuilders whose competition weight is in excess of 50 lb (23 kg) of muscle, larger than that of competitors in the past, and with even lower levels of body fat.[citation needed]
Insulin effects on strength, and exercise performance
[edit]Exogenous insulin significantly boosts the rate of glucose metabolism in training athletes along with a substantial increase in the peakV̇O2.[87]Insulin is thought to enhance performance by increasing protein synthesis, reducing protein catabolism, and facilitating the transfer of certain amino acids in human skeletal muscle. Insulin-treated athletes are perceived to have lean body mass because physiological hyperinsulinemia in human skeletal muscle improves the activity of amino acid transport, which in turn promotes protein synthesis.[87]Insulin stimulates the transport of amino acids into cells and also controls glucose metabolism. It decreases lipolysis and increases lipogenesis which is why bodybuilders and athletes userhGHin conjunction with it as to offset this negative effect while maximizing protein synthesis. The athletes extrapolated the physiology of the diabetic patient in the sporting arena because they are interested in the suppression of proteolysis. Insulin administration is found to be protein anabolic in the insulin-resistant state of chronic renal failure.[88]It inhibits proteolysis and when administered along with amino acids, it enhances net protein synthesis. Exogenous insulin injection creates an in-vivo hyperinsulinemic clamp, boosting muscle glycogen before and during the recovery phases of intense exercise. Power, strength, and stamina are all expected to increase as a result, and it might also speed up the healing process after intense physical activity. Second, insulin is expected to increase muscle mass by preventing the breakdown of muscle protein when consumed along with high carb-protein diet. Although a limited number of studies do suggest that insulin medication can be abused as a pharmacological treatment to boost strength and performance in young, healthy people or athletes, a recent assessment of the research argues that this is only applicable to a small group of "drug-naïve" individuals.[87]
Abuse
[edit]The abuse of exogenous insulin carries with it an attendant risk of hypoglycemic coma and death when the amount used is in excess of that required to handle ingested carbohydrate. Acute risks includebrain damage,paralysis,anddeath.Symptoms may include dizziness, weakness, trembling,palpitations,seizures, confusion, headache, drowsiness, coma,diaphoresisandnausea.All persons with overdoses should be referred for medical assessment and treatment, which may last for hours or days.[89]
Data from the US National Poison Data System (2013) indicates that 89.3% of insulin cases reported to poison centers are unintentional, as a result of therapeutic error. Another 10% of cases are intentional, and may reflect attempted suicide, abuse, criminal intent, secondary gain or other unknown reasons.[89]Hypoglycemia that has been induced by exogenous insulin can be chemically detected by examining the ratio of insulin toC-peptidein peripheral circulation.[90]It has been suggested that this type of approach could be used to detect exogenous insulin abuse by athletes.[91]
Detection in biological fluids
[edit]Insulin is often measured in serum, plasma or blood in order to monitor therapy in people who are diabetic, confirm a diagnosis of poisoning in hospitalized persons or assist in a medicolegal investigation of suspicious death. Interpretation of the resulting insulin concentrations is complex, given the numerous types of insulin available, various routes of administration, the presence of anti-insulin antibodies in insulin-dependent diabetics and theex vivoinstability of the drug. Other potential confounding factors include the wide-ranging cross-reactivity of commercial insulin immunoassays for the biosynthetic insulin analogs, the use of high-dose intravenous insulin as an antidote to antihypertensive drug over dosage and postmortem redistribution of insulin within the body. The use of a chromatographic technique for insulin assay may be preferable to immunoassay in some circumstances, to avoid the issue of cross-reactivity affecting the quantitative result and also to assist identifying the specific type of insulin in the specimen.[92]
Combination with other antidiabetic drugs
[edit]A combination therapy of insulin and otherantidiabetic drugsappears to be most beneficial in people who are diabetic, who still have residual insulin secretory capacity.[93]A combination of insulin therapy andsulfonylureais more effective than insulin alone in treating people with type 2 diabetes after secondary failure to oral drugs, leading to better glucose profiles and/or decreased insulin needs.[93]
Society and culture
[edit]Economics
[edit]United States
[edit]In the United States the unit price of insulin has increased steadily from 1991 to 2019.[94][95]It rose threefold from 2002 to 2013.[96]Costs can be as high as US$900 per month.[96]Concerns were raised in 2016 of pharmaceutical companies working together to increase prices.[96]In January 2019, lawmakers from theUnited States House of Representativessent letters to insulin manufacturersEli Lilly and Company,Sanofi,andNovo Nordiskasking for explanations for their rapidly raising insulin prices. The annual cost of insulin for people with type 1 diabetes in the US almost doubled from $2,900 to $5,700 over the period from 2012 to 2016.[97]
In 2019, it was estimated that people in the US pay two to six times more than the rest of the world for brand name prescription medicine, according to the International Federation of Health Plans.[98]
California, in July 2022, approved a budget that allocates $100 million for the state to create its own insulin at a close-to-cost price.[99]
Canada
[edit]Canada, like many other industrialized countries, has price controls on the cost of pharmaceuticals. ThePatented Medicine Prices Review Boardensures the price of patented medicine sold in Canada is "not excessive" and remains "comparable with prices in other countries."[98]
United Kingdom
[edit]Insulin, and all other medications, are supplied free of charge to people who use it to manage their diabetes by theNational Health Servicesof the countries of the United Kingdom.[100]
Regulatory status
[edit]United States
[edit]In March 2020, the FDA changed the regulatory pathway for approval of new insulin products.[101]Insulin is regulated as a biologic rather than as a drug.[101]The changed status gives the FDA more flexibility for approval and labeling.[102]In July 2021, the FDA approvedinsulin glargine-yfgn(Semglee), a biosimilar product that contains the long acting analog insulin glargine.[103]Insulin glargine-yfgn is interchangeable and less expensive than the reference product,insulin glargine(Lantus), which had been approved in 2000.[104]The FDA requires that new insulin products are not inferior to existing insulin products with respect to reduction in hemoglobin A1c.[105]
Research
[edit]Inhalation
[edit]In 2006, the USFood and Drug Administration(FDA) approved the use ofExubera,the firstinhalable insulin.[106]It was withdrawn from the market by its maker as of third quarter of 2007 due to lack of acceptance.[citation needed]
Inhaled insulin claimed to have similar efficacy to injected insulin, both in terms of controlling glucose levels and blood half-life. Currently, inhaled insulin is short-acting and is typically taken before meals; an injection of long-acting insulin at night is often still required.[107]When people were switched from injected to inhaled insulin, no significant difference was observed in HbA1clevels over three months. Accurate dosing was a particular problem, although people showed no significant weight gain or pulmonary function decline over the length of the trial when compared to the baseline.[108]
Following its commercial launch in 2005 in the United Kingdom, it was not (as of July 2006) recommended byNational Institute for Health and Clinical Excellencefor routine use, except in cases where there is "proven injection phobia diagnosed by a psychiatrist or psychologist".[107]
In January 2008, the world's largest insulin manufacturer,Novo Nordisk,also announced that the company was discontinuing all further development of the company's own version of inhalable insulin, known as the AERx iDMS inhaled insulin system.[109]Similarly,Eli Lilly and Companyended its efforts to develop its inhaled Air Insulin in March 2008.[110]Afrezza,developed byMannkind,was authorized by the FDA in June 2014 for use in adults with Type 1 and Type 2 diabetes, with a label restriction limiting its use only to those who also haveasthma,activelung cancer,orchronic obstructive pulmonary disease(COPD).[111]Rapid-acting inhaled insulin is a component of the drug-device combination solution that is used at the start of every meal. It employs technosphere technology, which appears to have a more practical delivery method and more dosing flexibility, and a new inhaled insulin formulation (2.5 m). A thumb-sized inhaler with improved dosage flexibility is used to deliver inhalable insulin. It includes powder-dissolved recombinant human insulin (fumaryl diketopiperazine). Technosphere insulin is quickly absorbed by the lung surface after inhalation. Within 12 hours of inhalation, both substances—insulin, and powder (fumaryl diketopiperazine)—are virtually eliminated from healthy people's lungs. In comparison to Exubera (8–9%), just 0.3% of inhaled insulin was still present in the lungs after 12 hours. However, since serum antibody levels have been reported to increase without substantial clinical changes, acute bronchospasm in asthmatic and COPD patients along with a significant reduction in Diffusing Lung Capacity for Carbon Monoxide, in comparison to subcutaneous insulin, have been reported with its usage, Afrezza was given FDA approval with a warning (Risk Evaluation and Mitigation Strategy).[112][111]
Transdermal
[edit]There are several methods for transdermal delivery of insulin.Pulsatile insulinuses microjets to pulse insulin into the person, mimicking the physiological secretions of insulin by the pancreas.[113]Jet injectionhad different insulin delivery peaks and durations as compared to needle injection. Some diabetics may prefer jet injectors to hypodermic injection.[114]Both electricity usingiontophoresis[115]and ultrasound have been found to make the skin temporarily porous. The insulin administration aspect remains experimental, but the blood glucose test aspect of "wrist appliances" is commercially available Researchers have produced a watch-like device that tests for blood glucose levels through the skin and administers corrective doses of insulin throughporesin the skin. A similar device, but relying on skin-penetrating "microneedles", was in the animal testing stage in 2015.[116]In the last couple of years, the use of chemical enhancers, electrical devices, and microneedle devices has shown tremendous promise for improving the penetration of insulin compared to passive transport via the skin. Transdermal insulin delivery shows a more patient-friendly and minimally invasive approach to daily diabetes care than the conventional hypodermic injection however, additional research is necessary to address issues such as long-term use, delivery efficiency, and reliability, as well as side effects involving inflammation and irritation.[117]
Intranasal
[edit]Insulin can be delivered to the central nervous system via the intranasal (IN) route with little to no systemic uptake or associated peripheral side effects. It has been demonstrated that intranasally delivered insulin rapidly accumulates in CSF fluid, indicating effective transport to the brain. This accumulation is thought to occur along olfactory and nearby routes. Although numerous studies have published encouraging results, further study is still being conducted to comprehend its long-term impacts in order to begin the successful clinical application.[118]
By mouth
[edit]The basic appeal of hypoglycemic agents by mouth is that most people would prefer a pill or an oral liquid to an injection. However, insulin is apeptide hormone,which isdigestedin thestomachandgutand in order to be effective at controlling blood sugar, cannot be taken orally in its current form.[citation needed]
The potential market for an oral form of insulin is assumed to be enormous, thus many laboratories have attempted to devise ways of moving enough intact insulin from the gut to theportal veinto have a measurable effect on blood sugar.[119]
A number ofderivatizationandformulationstrategies are currently being pursued to in an attempt to develop an orally available insulin.[120]Many of these approaches employnanoparticledelivery systems[121][122][123]and several are being tested inclinical trials.[124][125][126]
Pancreatic transplantation
[edit]Another improvement would be atransplantationof the pancreas or beta cell to avoid periodic insulin administration. This would result in a self-regulating insulin source. Transplantation of an entire pancreas (as an individualorgan) is difficult and relatively uncommon. It is often performed in conjunction withliverorkidneytransplant, although it can be done by itself. It is also possible to do a transplantation of only the pancreatic beta cells. However, islet transplants had been highly experimental for many years, but some researchers inAlberta, Canada,have developed techniques with a highinitialsuccess rate (about 90% in one group). Nearly half of those who got an islet cell transplant were insulin-free one year after the operation; by the end of the second year that number drops to about one in seven. However, researchers at the University of Illinois at Chicago (UIC) have slightly modified the Edmonton Protocol procedure for islet cell transplantation and achieved insulin independence in diabetic people, with fewer but better-functioning pancreatic islet cells.[127]
Beta cell transplant may become practical in the near future. Additionally, some researchers have explored the possibility of transplantinggenetically engineerednon-beta cells to secrete insulin.[128]
References
[edit]- ^"Humulin S (Soluble) 100IU/mL solution for injection in cartridge – Summary of Product Characteristics (SmPC)".(emc).Archivedfrom the original on 5 August 2020.Retrieved4 September2020.
- ^"Inpremzia EPAR".European Medicines Agency.23 February 2022.Retrieved3 March2023.
- ^"Inpremzia Product information".Union Register of medicinal products.Archivedfrom the original on 17 June 2024.Retrieved3 March2023.
- ^Harding MM, Hodgkin DC, Kennedy AF, O'Conor A, Weitzmann PD (March 1966). "The crystal structure of insulin. II. An investigation of rhombohedral zinc insulin crystals and a report of other crystalline forms".Journal of Molecular Biology.16(1): 212–26.doi:10.1016/S0022-2836(66)80274-7.PMID5917731.
- ^Abel JJ (February 1926)."Crystalline Insulin".Proceedings of the National Academy of Sciences of the United States of America.12(2): 132–6.Bibcode:1926PNAS...12..132A.doi:10.1073/pnas.12.2.132.PMC1084434.PMID16587069.
- ^abcdeAmerican Society of Health-System Pharmacists."Insulin Human".www.drugs.com.Archivedfrom the original on 22 October 2016.Retrieved1 January2017.
- ^Mahoney BA, Smith WA, Lo DS, Tsoi K, Tonelli M, Clase CM (April 2005)."Emergency interventions for hyperkalaemia".The Cochrane Database of Systematic Reviews.2005(2): CD003235.doi:10.1002/14651858.CD003235.pub2.PMC6457842.PMID15846652.
- ^World Health Organization(2021).World Health Organization model list of essential medicines: 22nd list (2021).Geneva: World Health Organization.hdl:10665/345533.WHO/MHP/HPS/EML/2021.02.
- ^"The Top 300 of 2021".ClinCalc.Archivedfrom the original on 15 January 2024.Retrieved14 January2024.
- ^"Insulin Human; Insulin Isophane Human - Drug Usage Statistics".ClinCalc.Archivedfrom the original on 17 June 2024.Retrieved14 January2024.
- ^abcBritish national formulary: BNF 69(69 ed.). British Medical Association. 2015. pp. 464–472.ISBN978-0-85711-156-2.
- ^Baeshen NA, Baeshen MN, Sheikh A, Bora RS, Ahmed MM, Ramadan HA, et al. (October 2014)."Cell factories for insulin production".Microbial Cell Factories.13(1): 141.doi:10.1186/s12934-014-0141-0.PMC4203937.PMID25270715.
- ^ab"Frederick Banting, Charles Best, James Collip, and John Macleod".Science History Institute.June 2016.Archivedfrom the original on 1 December 2018.Retrieved22 August2018.
- ^Fleishman JL, Kohler JS, Schindler S (2009).Casebook for The Foundation a Great American Secret.New York: PublicAffairs. p. 22.ISBN978-0-7867-3425-2.Archivedfrom the original on 18 January 2017.
- ^"Recherche sur le rôle du pancréas dans l'assimilation nutritive | The Discovery and Early Development of Insulin".insulin.library.utoronto.ca.Archivedfrom the original on 1 August 2020.Retrieved26 March2020.
- ^Banting FG (17–29 May 1922)."Chart for James Havens".University of Toronto Libraries.Archivedfrom the original on 1 August 2020.Retrieved9 January2019.
- ^Woodbury DO (February 1963)."Please save my son!".University of Toronto Libraries.Archivedfrom the original on 29 May 2019.Retrieved9 January2019.
- ^Banting FG (16 August 1922)."Chart for Elizabeth Hughes".University of Toronto Libraries.Archivedfrom the original on 10 January 2019.Retrieved9 January2019.
- ^Zuger A (4 October 2010)."Rediscovering the First Miracle Drug".New York Times.Archivedfrom the original on 15 April 2023.Retrieved6 October2010.
- ^University of Toronto Libraries (1923)."Miss Collier's recovery".University of Toronto Libraries.Archivedfrom the original on 10 January 2019.Retrieved9 January2019.
- ^Vecchio I, Tornali C, Bragazzi NL, Martini M (23 October 2018)."The Discovery of Insulin: An Important Milestone in the History of Medicine".Frontiers in Endocrinology.9:613.doi:10.3389/fendo.2018.00613.PMC6205949.PMID30405529.
- ^Jones K (March 2000)."Insulin coma therapy in schizophrenia".Journal of the Royal Society of Medicine.93(3): 147–9.doi:10.1177/014107680009300313.PMC1297956.PMID10741319.
- ^Ghazavi MK, Johnston GA (May–June 2011). "Insulin allergy".Clinics in Dermatology.29(3): 300–5.doi:10.1016/j.clindermatol.2010.11.009.PMID21496738.
- ^Ip KH, Koch K, Lamont D (July 2021). "Cutaneous amyloidoma secondary to repeated insulin injections".Postgraduate Medical Journal.97(1149): 474.doi:10.1136/postgradmedj-2020-138428.PMID32817579.S2CID221221349.
- ^Hanefeld M (December 2014)."Use of insulin in type 2 diabetes: what we learned from recent clinical trials on the benefits of early insulin initiation".Diabetes & Metabolism.40(6): 391–399.doi:10.1016/j.diabet.2014.08.006.PMID25451189.
- ^Owens DR (September 2013)."Clinical evidence for the earlier initiation of insulin therapy in type 2 diabetes".Diabetes Technology & Therapeutics.15(9): 776–785.doi:10.1089/dia.2013.0081.PMC3757533.PMID23786228.
- ^Takiya L, Dougherty T."Pharmacist's Guide to Insulin Preparations: A Comprehensive Review".Pharmacy Times. Archived fromthe originalon 15 July 2011.Retrieved2 August2010.
- ^abNasrallah SN, Reynolds LR (1 April 2012)."Insulin Degludec, The New Generation Basal Insulin or Just another Basal Insulin?".Clinical Medicine Insights. Endocrinology and Diabetes.5:31–7.doi:10.4137/CMED.S9494.PMC3411522.PMID22879797.
- ^abcGaldo JA, Thurston MM, Bourg CA (April 2014)."Clinical Considerations for Insulin Pharmacotherapy in Ambulatory Care, Part One: Introduction and Review of Current Products and Guidelines".Clinical Diabetes.32(2): 66–75.doi:10.2337/diaclin.32.2.66.PMC4485243.PMID26130864.
- ^Papatheodorou I, Petrovs R, Thornton JM (November 2014)."Comparison of the mammalian insulin signalling pathway to invertebrates in the context of FOXO-mediated ageing".Bioinformatics.30(21): 2999–3003.doi:10.1093/bioinformatics/btu493.PMC4201157.PMID25064569.
- ^"Insulin Basics".American Diabetes Association.Archived fromthe originalon 14 February 2014.Retrieved22 August2018.
- ^McCall AL (March 2012)."Insulin therapy and hypoglycemia".Endocrinology and Metabolism Clinics of North America.41(1): 57–87.doi:10.1016/j.ecl.2012.03.001.PMC4265808.PMID22575407.
- ^Davidson MB (July 2015)."Insulin Therapy: A Personal Approach".Clinical Diabetes.33(3): 123–35.doi:10.2337/diaclin.33.3.123.PMC4503941.PMID26203205.
- ^Wendt D (1 November 2013)."Two tons of pig parts: Making insulin in the 1920s".National Museum of American History.Archivedfrom the original on 27 October 2018.Retrieved22 August2018.
- ^Kehoe A (1989)."The story of biosynthetic human insulin".In Sikdar SK, Bier M, Todd PW (eds.).Frontiers in Bioprocesssing.Boca Raton, FL: CRC Press.ISBN978-0-8493-5839-5.Archivedfrom the original on 3 August 2020.Retrieved22 August2018.
- ^abcCrasto W, Jarvis J, Davies M (9 September 2016)."Chapter 2 Existing insulin therapies".Handbook of Insulin Therapies.Springer. pp. 15–18.ISBN978-3-319-10939-8.Archivedfrom the original on 3 August 2020.Retrieved22 August2018.
- ^Altman LK (30 October 1982)."A New Insulin Given Approval For Use In U.S."The New York Times.Archivedfrom the original on 23 August 2018.Retrieved23 August2018.
- ^Bowden ME (2018)."Old Brew, New Brew".Distillations.4(2).Science History Institute:8–11.Archivedfrom the original on 21 August 2018.Retrieved21 August2018.
- ^Novolog Patient Leaflet
- ^Diabetes Atlas(2nd ed.). Brussels: International Diabetes Federation. 2004. Archived fromthe originalon 3 August 2012.
- ^Brown P (9 March 1999)."Diabetics not told of insulin risk".The Guardian.Archivedfrom the original on 4 February 2017.
- ^"Position Statement".Brussels: International Diabetes Federation. March 2005. Archived fromthe originalon 4 May 2009.
- ^"Importing Beef or Pork Insulin for Personal Use".U.S.Food and Drug Administration(FDA).6 July 2005.Retrieved17 June2024.
- ^"Overview".Vetsulin-Veterinary.Archived fromthe originalon 21 January 2010.
- ^abcAmerican Diabetes Association (20 December 2019)."Pharmacologic Approaches to Glycemic Treatment".Diabetes Care.43(Supplement 1): S98–S110.doi:10.2337/dc20-S009.PMID31862752.
- ^American Diabetes Association (20 December 2019)."Diabetes Technology: Standards of Medical Care in Diabetes—2020".Diabetes Care.43(Supplement 1): S77–S88.doi:10.2337/dc20-S007.PMID31862750.
- ^Sorli C (July 2014)."Identifying and meeting the challenges of insulin therapy in type 2 diabetes".Journal of Multidisciplinary Healthcare.7:267–82.doi:10.2147/JMDH.S64084.PMC4086769.PMID25061317.
- ^Weiss M, Steiner DF, Philipson LH (1 February 2014)."Insulin Biosynthesis, Secretion, Structure, and Structure-Activity Relationships".In Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, Dungan K, Hershman JM, Hofland J, Kalra S, Kaltsas G, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, Morley JE, New M, Purnell J, Sahay R, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP (eds.).Endotext.MDText.com, Inc.PMID25905258.
- ^Richter B, Neises G (January 2005)."'Human' insulin versus animal insulin in people with diabetes mellitus ".The Cochrane Database of Systematic Reviews.2010(1): CD003816.doi:10.1002/14651858.CD003816.pub2.PMC8406912.PMID15674916.
- ^abIQwiG (German Institute for Quality and Efficiency in Health Care) (6 June 2007)."Rapid-acting insulin analogues in the treatment of diabetes mellitus type 1: Superiority Not Proven".Archived fromthe originalon 19 July 2011.Retrieved2 August2010.
- ^abBanerjee S, Tran K, Li H, Cimon K, Daneman D, Simpson S, et al. (March 2007)."Short-acting insulin analogues for diabetes mellitus: meta-analysis of clinical outcomes and assessment of cost effectiveness".Canadian Agency for Drugs and Technologies in Health.87:1–55.Archivedfrom the original on 4 November 2019.Retrieved4 November2019.
- ^"Biodel Inc. Announces VIAject(TM) Data at Oral Presentation at the American Diabetes Association Meeting"(PDF).Archived fromthe original(PDF)on 31 October 2008.
- ^"FDA Accepts VIAject NDA for Review".Archived fromthe originalon 6 August 2011.
- ^Krzymien J, Ladyzynski P (March 2019)."Insulin in Type 1 and Type 2 Diabetes-Should the Dose of Insulin Before a Meal be Based on Glycemia or Meal Content?".Nutrients.11(3): 607.doi:10.3390/nu11030607.PMC6471836.PMID30871141.
- ^Saleem F, Sharma A (2022)."NPH Insulin".StatPearls.Treasure Island (FL): StatPearls Publishing.PMID31751050.Archivedfrom the original on 17 June 2024.Retrieved4 January2023.
- ^Cunningham AM, Freeman AM (2022).Glargine Insulin.Treasure Island (FL): StatPearls Publishing.PMID32491688.Retrieved4 January2023.
- ^"Insulin detemir".PubChem.U.S. National Library of Medicine.Retrieved4 January2023.
- ^"DailyMed - NOVOLOG MIX 70/30- insulin aspart injection, suspension".dailymed.nlm.nih.gov.Retrieved4 January2023.
- ^Fonte P, Araújo F, Reis S, Sarmento B (March 2013)."Oral insulin delivery: how far are we?".Journal of Diabetes Science and Technology.7(2): 520–531.doi:10.1177/193229681300700228.PMC3737653.PMID23567010.
- ^American Diabetes Association (January 2004)."Insulin administration".Diabetes Care.27(suppl_1): S106–S109.doi:10.2337/diacare.27.2007.s106.PMID14693942.
- ^abBerget C, Messer LH, Forlenza GP (August 2019)."A Clinical Overview of Insulin Pump Therapy for the Management of Diabetes: Past, Present, and Future of Intensive Therapy".Diabetes Spectrum.32(3): 194–204.doi:10.2337/ds18-0091.PMC6695255.PMID31462873.
- ^"Early definitions of a unit of insulin were based on a rabbit's physiological response. – Treating Diabetes".Treating Diabetes.Archived fromthe originalon 8 September 2017.Retrieved18 June2017.
- ^"Mission statement".WHO Expert Committee on Biological Standardization.Archived fromthe originalon 27 January 2012.
- ^Thota S, Akbar A (2022)."Insulin".StatPearls.Treasure Island (FL): StatPearls Publishing.PMID32809523.Retrieved4 January2023.
- ^Bird SR, Hawley JA (March 2017)."Update on the effects of physical activity on insulin sensitivity in humans".BMJ Open Sport & Exercise Medicine.2(1): e000143.doi:10.1136/bmjsem-2016-000143.PMC5569266.PMID28879026.
- ^Scheiner G, Boyer BA (July 2005). "Characteristics of basal insulin requirements by age and gender in Type-1 diabetes patients using insulin pump therapy".Diabetes Research and Clinical Practice.69(1): 14–21.doi:10.1016/j.diabres.2004.11.005.PMID15955383.
- ^Munguia C, Correa R (2022).Regular Insulin.Treasure Island (FL): StatPearls Publishing.PMID31971734.Archivedfrom the original on 17 June 2024.Retrieved5 January2023.
- ^Joslin EP (1934).A Diabetic Manual for the Mutual Use of Doctor and Patient.Philadelphia, PA: Lea & Febiger. pp.108.
- ^abMunshi MN, Florez H, Huang ES, Kalyani RR, Mupanomunda M, Pandya N, et al. (February 2016)."Management of Diabetes in Long-term Care and Skilled Nursing Facilities: A Position Statement of the American Diabetes Association".Diabetes Care.39(2): 308–18.doi:10.2337/dc15-2512.PMC5317234.PMID26798150.
- ^McDonnell ME, Umpierrez GE (March 2012)."Insulin therapy for the management of hyperglycemia in hospitalized patients".Endocrinology and Metabolism Clinics of North America.41(1): 175–201.doi:10.1016/j.ecl.2012.01.001.PMC3738170.PMID22575413.
- ^Corsino L, Dhatariya K, Umpierrez G (2000)."Management of Diabetes and Hyperglycemia in Hospitalized Patients".In De Groot LJ, Chrousos G, Dungan K, Feingold KR, Grossman A, Hershman JM, Koch C, Korbonits M, McLachlan R, New M, Purnell J, Rebar R, Singer F, Vinik A (eds.).Endotext.South Dartmouth (MA): MDText.com, Inc.PMID25905318.Archivedfrom the original on 28 August 2021.Retrieved23 August2018.
- ^Zaman Huri H, Permalu V, Vethakkan SR (2 September 2014)."Sliding-scale versus basal-bolus insulin in the management of severe or acute hyperglycemia in type 2 diabetes patients: a retrospective study".PLOS ONE.9(9): e106505.Bibcode:2014PLoSO...9j6505Z.doi:10.1371/journal.pone.0106505.PMC4152280.PMID25181406.
- ^Umpierrez GE, Palacio A, Smiley D (July 2007). "Sliding scale insulin use: myth or insanity?".The American Journal of Medicine.120(7): 563–7.doi:10.1016/j.amjmed.2006.05.070.PMID17602924.
- ^Hirsch IB (January 2009)."Sliding scale insulin—time to stop sliding"(PDF).JAMA.301(2): 213–4.doi:10.1001/jama.2008.943.PMID19141770.Archived(PDF)from the original on 3 November 2019.Retrieved4 November2019.
- ^abAMDA – The Society for Post-Acute and Long-Term Care Medicine(February 2014),"Five Things Physicians and Patients Should Question",Choosing Wisely:an initiative of theABIM Foundation,AMDA – The Society for Post-Acute and Long-Term Care Medicine, archived fromthe originalon 13 September 2014,retrieved10 February2013,which cites:
- American Geriatrics Society 2012 Beers Criteria Update Expert Panel (April 2012)."American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults".Journal of the American Geriatrics Society.60(4): 616–31.doi:10.1111/j.1532-5415.2012.03923.x.PMC3571677.PMID22376048.
- American Medical Directors Association (2010)."National Guideline Clearinghouse | Diabetes management in the long term care setting".guideline.gov.Archived fromthe originalon 20 August 2014.Retrieved11 September2014.
- Pandya N, Thompson S, Sambamoorthi U (November 2008). "The prevalence and persistence of sliding scale insulin use among newly admitted elderly nursing home residents with diabetes mellitus".Journal of the American Medical Directors Association.9(9): 663–9.doi:10.1016/j.jamda.2008.06.003.PMID18992699.
- ^Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH (October 2018)."The Pathophysiology of Gestational Diabetes Mellitus".International Journal of Molecular Sciences.19(11): 3342.doi:10.3390/ijms19113342.PMC6274679.PMID30373146.
- ^Subiabre M, Silva L, Toledo F, Paublo M, López MA, Boric MP, et al. (September 2018)."Insulin therapy and its consequences for the mother, foetus, and newborn in gestational diabetes mellitus".Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.1864(9 Pt B): 2949–2956.doi:10.1016/j.bbadis.2018.06.005.PMID29890222.S2CID48362789.
- ^abAlexopoulos AS, Blair R, Peters AL (May 2019)."Management of Preexisting Diabetes in Pregnancy: A Review".JAMA.321(18): 1811–1819.doi:10.1001/jama.2019.4981.PMC6657017.PMID31087027.
- ^Dotinga R (24 August 2001)."Athletes Turn to Insulin to Boost Performance Experts warn of danger to non-diabetics".HealthDayNews.Archivedfrom the original on 23 August 2018.Retrieved22 August2018.
- ^Sonksen PH (July 2001)."Insulin, growth hormone and sport".The Journal of Endocrinology.170(1): 13–25.doi:10.1677/joe.0.1700013.PMID11431133.
- ^abEvans PJ, Lynch RM (August 2003)."Insulin as a drug of abuse in body building".British Journal of Sports Medicine.37(4): 356–357.doi:10.1136/bjsm.37.4.356.PMC1724679.PMID12893725.
- ^Kakutani M (23 March 2006)."Barry Bonds and Baseball's Steroids Scandal".The New York Times.Archivedfrom the original on 28 November 2018.Retrieved22 August2018.
- ^"Barry Bonds steroids timeline".ESPN.com.7 December 2007.Archivedfrom the original on 2 December 2018.Retrieved22 August2018.
- ^Holt RI, Sönksen PH (June 2008)."Growth hormone, IGF-I and insulin and their abuse in sport".British Journal of Pharmacology.154(3): 542–56.doi:10.1038/bjp.2008.99.PMC2439509.PMID18376417.
- ^Reitman V (8 September 2003)."Bodybuilders and insulin Some weightlifters are using the hormone to gain muscle, a practice that poses serious risks, doctors warn".Los Angeles Times.Archivedfrom the original on 27 November 2018.Retrieved22 August2018.
- ^Crosbie J (21 November 2017)."35-Year-Old Bodybuilder's Sudden Death Raises Questions About Insulin Use Ghent Wakefield was an aspiring WWE wrestler".Men's Health.Archivedfrom the original on 23 August 2018.Retrieved22 August2018.
- ^abcGraham MR, Evans P, Davies B, Baker JS (June 2008)."AAS, growth hormone, and insulin abuse: psychological and neuroendocrine effects".Therapeutics and Clinical Risk Management.4(3): 587–597.doi:10.2147/tcrm.s2495.PMC2500251.PMID18827854.
- ^Lim VS, Yarasheski KE, Crowley JR, Fangman J, Flanigan M (September 2003)."Insulin is protein-anabolic in chronic renal failure patients".Journal of the American Society of Nephrology.14(9): 2297–2304.doi:10.1097/01.ASN.0000085590.83005.A0.PMID12937306.S2CID20467179.
- ^abKlein-Schwartz W, Stassinos GL, Isbister GK (March 2016)."Treatment of sulfonylurea and insulin overdose".British Journal of Clinical Pharmacology.81(3): 496–504.doi:10.1111/bcp.12822.PMC4767194.PMID26551662.
- ^De León DD, Stanley CA (December 2013)."Determination of insulin for the diagnosis of hyperinsulinemic hypoglycemia".Best Practice & Research. Clinical Endocrinology & Metabolism.27(6): 763–9.doi:10.1016/j.beem.2013.06.005.PMC4141553.PMID24275188.
- ^Thomas A, Thevis M, Delahaut P, Bosseloir A, Schänzer W (March 2007). "Mass spectrometric identification of degradation products of insulin and its long-acting analogues in human urine for doping control purposes".Analytical Chemistry.79(6): 2518–24.doi:10.1021/ac062037t.PMID17300174.
- ^R. Baselt,Disposition of Toxic Drugs and Chemicals in Man,8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 775–779.
- ^abScheen AJ, Castillo MJ, Lefèbvre PJ (1993). "Combination of oral antidiabetic drugs and insulin in the treatment of non-insulin-dependent diabetes".Acta Clinica Belgica.48(4): 259–68.doi:10.1080/17843286.1993.11718317.PMID8212978.
- ^Luo J,Avorn J,Kesselheim AS (October 2015). "Trends in Medicaid Reimbursements for Insulin From 1991 Through 2014".JAMA Internal Medicine.175(10): 1681–6.doi:10.1001/jamainternmed.2015.4338.PMID26301721.
- ^Zargar AH, Kalra S, K M PK, Murthy S, Negalur V, Rajput R, et al. (June 2022)."Rising cost of insulin: A deterrent to compliance in patients with diabetes mellitus".Diabetes & Metabolic Syndrome: Clinical Research & Reviews.16(8): 102528.doi:10.1016/j.dsx.2022.102528.PMID35863268.S2CID249329716.
{{cite journal}}:CS1 maint: overridden setting (link) - ^abcThomas K (30 January 2017)."Drug Makers Accused of Fixing Prices on Insulin".The New York Times.Archivedfrom the original on 8 September 2017.Retrieved9 July2023.
full text available via archive link without subscription - ^Abutaleb Y (30 January 2019)."U.S. lawmakers request info from insulin makers on rising prices".Reuters.Archivedfrom the original on 31 January 2019.Retrieved1 February2019.
- ^ab"Here's Why Insulin and Other Drugs Are Cheaper in Canada".28 July 2019.Archivedfrom the original on 25 February 2021.Retrieved13 January2021.
- ^"California To Make Its Own Insulin In Fight Against Inflated Drug Prices".IFLScience.8 July 2022.Archivedfrom the original on 9 July 2022.Retrieved11 July2022.
- ^"Free prescriptions (England)".Diabetes UK.Retrieved21 November2022.
If you use insulin or medicine to manage your diabetes,... you don't pay for any item you're prescribed.
- ^ab"Definition of the Term" Biological Product "".Federal Register.21 February 2020.Archivedfrom the original on 8 August 2022.Retrieved8 August2022.
- ^"Labeling Requirements for Human Prescription Drug and Biological Products – OMB 0910-0572".OMB.31 January 2022.Archivedfrom the original on 13 August 2022.Retrieved8 August2022.
- ^"Drug Approval Package: Semglee".U.S.Food and Drug Administration(FDA).2 September 2021.Archivedfrom the original on 27 May 2022.Retrieved8 August2022.
- ^"Drug Approval Package: Lantus (Insulin Glargine [rDNA Origin]) NDA #21-081".U.S.Food and Drug Administration(FDA).20 November 2001.Archivedfrom the original on 13 August 2022.Retrieved8 August2022.
- ^Misbin, RI (2022),Insulin – History from an FDA Insider,Washington, DC: Politics and Prose Publishing
- ^"FDA approval ofExuberainhaled insulin ".U.S.Food and Drug Administration(FDA).Archived fromthe originalon 26 December 2008.
- ^abNICE(21 June 2006)."Diabetes (type 1 and 2), Inhaled Insulin – Appraisal Consultation Document (second)".Archived fromthe originalon 7 July 2006.Retrieved26 July2006.
- ^Cefalu WT,Skyler JS,Kourides IA, Landschulz WH, Balagtas CC, Cheng S, et al. (February 2001). "Inhaled human insulin treatment in patients with type 2 diabetes mellitus".Annals of Internal Medicine.134(3): 203–7.doi:10.7326/0003-4819-134-3-200102060-00011.PMID11177333.S2CID25294223.
- ^"Novo Nordisk refocuses its activities within inhaled insulin and discontinues the development of AERx".14 January 2008. Archived fromthe originalon 7 September 2012.
- ^"Lilly Ends Effort to Develop an Inhaled Insulin Product".The New York Times.8 March 2008.Archivedfrom the original on 12 September 2017.Retrieved22 February2017.
- ^abMohanty RR, Das S (April 2017)."Inhaled Insulin - Current Direction of Insulin Research".Journal of Clinical and Diagnostic Research.11(4): OE01–OE02.doi:10.7860/JCDR/2017/23626.9732.PMC5449846.PMID28571200.
- ^Klonoff DC (November 2014)."Afrezza inhaled insulin: the fastest-acting FDA-approved insulin on the market has favorable properties".Journal of Diabetes Science and Technology.8(6): 1071–1073.doi:10.1177/1932296814555820.PMC4455463.PMID25355710.
- ^Arora A, Hakim I, Baxter J, Rathnasingham R, Srinivasan R, Fletcher DA, et al. (March 2007)."Needle-free delivery of macromolecules across the skin by nanoliter-volume pulsed microjets".Proceedings of the National Academy of Sciences of the United States of America.104(11): 4255–60.Bibcode:2007PNAS..104.4255A.doi:10.1073/pnas.0700182104.PMC1838589.PMID17360511.
- ^Guo L, Xiao X, Sun X, Qi C (January 2017)."Comparison of jet injector and insulin pen in controlling plasma glucose and insulin concentrations in type 2 diabetic patients".Medicine.96(1): e5482.doi:10.1097/MD.0000000000005482.PMC5228650.PMID28072690.
- ^Dixit N, Bali V, Baboota S, Ahuja A, Ali J (January 2007)."Iontophoresis – an approach for controlled drug delivery: a review".Current Drug Delivery.4(1): 1–10.doi:10.2174/156720107779314802.PMID17269912.Archivedfrom the original on 28 August 2021.Retrieved4 November2019.
- ^Yu J, Zhang Y, Ye Y, DiSanto R, Sun W, Ranson D, et al. (July 2015)."Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery".Proceedings of the National Academy of Sciences of the United States of America.112(27): 8260–5.Bibcode:2015PNAS..112.8260Y.doi:10.1073/pnas.1505405112.PMC4500284.PMID26100900.
- ^Zhang Y, Yu J, Kahkoska AR, Wang J, Buse JB, Gu Z (January 2019)."Advances in transdermal insulin delivery".Advanced Drug Delivery Reviews.139:51–70.doi:10.1016/j.addr.2018.12.006.PMC6556146.PMID30528729.
- ^Hallschmid M (April 2021)."Intranasal insulin".Journal of Neuroendocrinology.33(4): e12934.doi:10.1111/jne.12934.PMID33506526.S2CID231770007.
- ^"Oral Insulin – Fact or Fiction? – Resonance – May 2003".Archivedfrom the original on 9 September 2007.Retrieved23 September2007.
- ^Kalra S, Kalra B, Agrawal N (November 2010)."Oral insulin".Diabetology & Metabolic Syndrome.2:66.doi:10.1186/1758-5996-2-66.PMC2987915.PMID21059246.
- ^Card JW, Magnuson BA (December 2011). "A review of the efficacy and safety of nanoparticle-based oral insulin delivery systems".American Journal of Physiology. Gastrointestinal and Liver Physiology.301(6): G956–G967.doi:10.1152/ajpgi.00107.2011.PMID21921287.
- ^Chen MC, Sonaje K, Chen KJ, Sung HW (December 2011). "A review of the prospects for polymeric nanoparticle platforms in oral insulin delivery".Biomaterials.32(36): 9826–38.doi:10.1016/j.biomaterials.2011.08.087.PMID21925726.
- ^Fonte P, Araújo F, Reis S, Sarmento B (March 2013)."Oral insulin delivery: how far are we?".Journal of Diabetes Science and Technology.7(2): 520–31.doi:10.1177/193229681300700228.PMC3737653.PMID23567010.
- ^Iyer H, Khedkar A, Verma M (March 2010)."Oral insulin – a review of current status".Diabetes, Obesity & Metabolism.12(3): 179–85.doi:10.1111/j.1463-1326.2009.01150.x.PMID20151994.S2CID24632760.Archivedfrom the original on 12 July 2021.Retrieved4 November2019.
- ^Pozzilli P, Raskin P, Parkin CG (February 2010)."Review of clinical trials: update on oral insulin spray formulation".Diabetes, Obesity & Metabolism.12(2): 91–6.doi:10.1111/j.1463-1326.2009.01127.x.PMID19889002.S2CID36965357.Archivedfrom the original on 28 August 2021.Retrieved23 August2018.
- ^"First Oral Insulin For Diabetics Takes Major Step Towards FDA Approval".Oramed.com.16 May 2018.Archivedfrom the original on 23 August 2018.Retrieved23 August2018.
- ^Gangemi A, Salehi P, Hatipoglu B, Martellotto J, Barbaro B, Kuechle JB, et al. (June 2008)."Islet transplantation for brittle type 1 diabetes: the UIC protocol".American Journal of Transplantation.8(6): 1250–61.doi:10.1111/j.1600-6143.2008.02234.x.PMID18444920.
- ^Zhu YL, Abdo A, Gesmonde JF, Zawalich KC, Zawalich W, Dannies PS (August 2004)."Aggregation and lack of secretion of most newly synthesized proinsulin in non-beta-cell lines".Endocrinology.145(8): 3840–9.doi:10.1210/en.2003-1512.PMID15117881.
