Anaplasma phagocytophilum
| Anaplasma phagocytophilum | |
|---|---|
| |
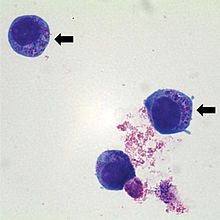
| HumanHL60cells containingAnaplasma phagocytophilum(indicated by arrows) which are basophilic intracytoplasmic inclusions when stained withWright-Giemsa stain | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Pseudomonadota |
| Class: | Alphaproteobacteria |
| Order: | Rickettsiales |
| Family: | Ehrlichiaceae |
| Genus: | Anaplasma |
| Species: | A. phagocytophilum
|
| Binomial name | |
| Anaplasma phagocytophilum (Foggie 1949) Dumler et al. 2001[1]
| |
| Synonyms | |
|
Rickettsia phagocytophila ovis | |
Anaplasma phagocytophilum(formerlyEhrlichia phagocytophilum)[2]is a Gram-negative bacterium that is unusual in its tropism toneutrophils.It causesanaplasmosisin sheep and cattle, also known astick-borne feverandpasture fever,and also causes thezoonoticdiseasehuman granulocytic anaplasmosis.[3]
A. phagocytophilumis aGram-negative,obligate bacterium of neutrophils. It causes human granulocytic anaplasmosis, which is a tick-borne rickettsial disease. Because this bacterium invades neutrophils, it has a unique adaptation and pathogenetic mechanism.[4]
Biology[edit]
A. phagocytophilumis a small, obligate, intracellular bacterium with a Gram-negative cell wall. It is 0.2–1.0 μm and lacks a lipopolysaccharide biosynthetic machinery. The bacterium first resides in an earlyendosome,where it acquires nutrients for binary fission and grows into small groups called morulae. This bacterium prefers to grow within myeloid or granulocytic cells.[4]
Hosts[edit]
Hosts includegoat,cattle,horseanddog.Cattle infections had been suspected but were only first confirmed by Nieder et al. 2012.[5]
Role in human disease[edit]
A. phagocytophilumcauses human granulocyticanaplasmosis(HGA). This disease was first identified in 1990, although this pathogen was known to cause veterinary disease since 1932. Since 1990, incidence of HGA has increased, and it is now recognized in Europe. This disease was first identified due to a Wisconsin patient who died with a severe febrile illness two weeks after a tick bite. During the last stage of the infection, a group of small bacteria was seen within the neutrophils in the blood. Other symptoms include fever, headache, absence of skin rash,leucopenia,thrombocytopenia,and mild injury to the liver.[4]
Clinical signs in animals[edit]
The disease is multisystemic, but the most severe changes areanaemiaandleukopenia.This organism causeslameness,which can be confused with symptoms ofLyme disease,another tick-borne illness. It is a vector-bornezoonotic diseasewhose morula can be visualized withinneutrophils(a type of white blood cell) from the peripheral blood and synovial fluid. It can causelethargy,ataxia,loss of appetite,and weak or painful limbs.[3]
Bacterial mechanism[edit]
A. phagocytophilumbinds to fucosylated and sialylated scaffold proteins on neutrophil and granulocyte surfaces. Atype IV secretion apparatusis known to help in the transfer of molecules between the bacterium and the host. The most studied ligand is PSGL-1 (CD162). The bacterium adheres to PSGL-1 (CD162) through the 44-kDa major surface protein-2 (Msp2). After the bacterium enters the cell, the endosome stops maturation and does not accumulate markers of late endosomes orphagolysosomes.Because of this, the vacuole does not become acidified or fused tolysosomes.A. phagocytophilumthen divides untilcell lysisor when the bacteria leave to infect other cells.[4]
This bacterium has the ability to affect neutrophils by altering their function. It can survive the first encounter with the host cell by detoxifyingsuperoxideproduced byneutrophil phagocyte oxidaseassembly. It also disrupts normal neutrophil function, such as endothelial cell adhesion, transmigration, motility, degranulation, respiratory burst, and phagocytosis.[4]It causes an increase in the secretion ofIL-8,a chemoattractant that increases the phagocytosis of neutrophils. The purpose of this is to increase bacterial dissemination into the neutrophil.[6]
Laboratory diagnosis[edit]
These tests can be performed to determine anA. phagocytophiluminfection:
- Indirect immunofluorescence assay is the principal test used to detect infection. The acute and convalescent phase serum samples can be evaluated to look for a four-fold change in antibody titer toA. phagocytophilum.
- Intracellular Inclusions (morulae) are visualized in granulocytes on Wright- orGiemsa-stained blood smears.
- Polymerase chain reaction assays are used to detectA. phagocytophilumDNA.[7]
Antibiotic therapy[edit]
Patients with HGA undergodoxycyclinetherapy, 100 mg twice daily until the patient's fever subsides for at least 3 days. This drug has been the most beneficial to those patients infected with the bacteria. Some othertetracyclinedrugs are also effective. In general, patients with symptoms of HGA and unexplained fever after a tick exposure should receive empiric doxycycline therapy while their diagnostic tests are pending, especially if they experienceleukopeniaand/orthrombocytopenia.[7]
In animals, antibiotics such asoxytetracycline,sulphamethazine,sulphadimidine,doxycycline,andtrimethoprim-sulphonamideshave been used.[3]
References[edit]
- ^Page Anaplasma on lpsn.dsmz.de
- ^Dumler JS, Barbet AF, Bekker CP, et al. (2001)."Reorganization of genera in the families Rickettsiaceae and Anaplasmataceae in the order Rickettsiales: unification of some species of Ehrlichia with Anaplasma, Cowdria with Ehrlichia and Ehrlichia with Neorickettsia, descriptions of six new species combinations and designation of Ehrlichia equi and 'HGE agent' as subjective synonyms of Ehrlichia phagocytophila".Int. J. Syst. Evol. Microbiol.51(Pt 6): 2145–65.doi:10.1099/00207713-51-6-2145.PMID11760958.
- ^abcTick-Borne Feverreviewed and published byWikiVet,accessed 12 October 2011.
- ^abcdeDumler JS, Choi KS, Garcia-Garcia JC, et al. (December 2005)."Human granulocytic anaplasmosis andAnaplasma phagocytophilum".Emerging Infect. Dis.11(12): 1828–34.doi:10.3201/eid1112.050898.PMC3367650.PMID16485466.
- ^Brown, Wendy C.; Barbet, Anthony F. (2016-02-15). "Persistent Infections and Immunity in Ruminants to Arthropod-Borne Bacteria in the Family Anaplasmataceae".Annual Review of Animal Biosciences.4(1).Annual Reviews:177–197.doi:10.1146/annurev-animal-022513-114206.ISSN2165-8102.PMID26734888.
- ^Thomas V, Fikrig E (July 2007). "Anaplasma phagocytophilumspecifically induces tyrosine phosphorylation of ROCK1 during infection ".Cell. Microbiol.9(7): 1730–7.doi:10.1111/j.1462-5822.2007.00908.x.PMID17346310.S2CID20043230.
- ^ab"Human Anaplasmosis Information for Health Professionals: Diagnostic tests".Diseases.Minnesota Department of Health. Archived fromthe originalon 2019-02-13.Retrieved2011-04-27.
External links[edit]
- Anaplasmaphagocytophilum HZ Genome Page
- Anaplasma+phagocytophilumat the U.S. National Library of MedicineMedical Subject Headings(MeSH)
- Zhang L, Liu Y, Ni D, et al. (November 2008)."Nosocomial transmission of human granulocytic anaplasmosis in China".JAMA.300(19): 2263–70.doi:10.1001/jama.2008.626.PMID19017912.
