Arteriole
| Arteriole | |
|---|---|
 Types of blood vessels, including an arteriole and artery, as well as capillaries. | |
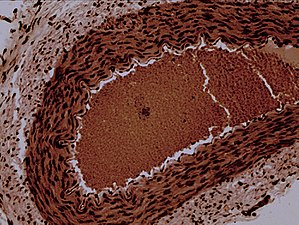 Rabbit arteriole at 100X | |
| Details | |
| Pronunciation | /ɑːrˈtɪəri.oʊl/ |
| Identifiers | |
| Latin | arteriola |
| MeSH | D001160 |
| TA98 | A12.0.00.005 |
| TA2 | 3900 |
| FMA | 63182 |
| Anatomical terminology | |
Anarterioleis a small-diameterblood vesselin themicrocirculationthat extends and branches out from anarteryand leads tocapillaries.[1]
Arterioles havemuscularwalls (usually only one to two layers ofsmooth muscle cells) and are the primary site ofvascular resistance.The greatest change in blood pressure and velocity of blood flow occurs at the transition of arterioles to capillaries. This function is extremely important because it prevents the thin, one-layer capillaries from exploding upon pressure. The arterioles achieve this decrease in pressure, as they are the site with the highest resistance (a large contributor to total peripheral resistance) which translates to a large decrease in the pressure.[2]
Structure
[edit]In a healthy vascular system, theendotheliumlines all blood-contacting surfaces, including arteries, arterioles, veins, venules, capillaries, and heart chambers. This healthy condition is promoted by the ample production ofnitric oxideby the endothelium, which requires a biochemical reaction regulated by a complex balance ofpolyphenols,variousnitric oxide synthaseenzymesand L-arginine.In addition, there is direct electrical and chemical communication viagap junctionsbetween the endothelial cells and the vascular smooth muscle.
Physiology
[edit]Blood pressure
[edit]Blood pressurein the arteries supplying the body is a result of the work needed to pump thecardiac output(the flow of blood pumped by the heart) through thevascular resistance,sometimes termedtotal peripheral resistance.An increase in thetunica mediato luminal diameter ratio has been observed in hypertensive arterioles (arteriolosclerosis) as the vascular wall thickens and/or luminal diameter decreases.
The up and down fluctuation of thearterialblood pressure is due to the pulsatile nature of thecardiac outputand determined by the interaction of thestroke volumeversus the volume and elasticity of the major arteries.
The decreased velocity of flow in the capillaries increases the blood pressure, due toBernoulli's principle.This induces gas and nutrients to move from the blood to the cells, due to the lowerosmotic pressureoutside the capillary. The opposite process occurs when the blood leaves the capillaries and enters thevenules,where the blood pressure drops due to an increase in flow rate. Arterioles receiveautonomic nervous systeminnervation and respond to various circulatinghormonesin order to regulate their diameter. Retinal vessels lack a functional sympathetic innervation.[3]
Autoregulation
[edit]Arteriole diameter varies according to autoregulation of organs or tissues to maintain sufficient blood flow despite changes in pressure via metabolic ormyogenic factorswhich include stretch, carbon dioxide, and oxygen among other factors.[4]Generally, norepinephrine and epinephrine (hormones produced by sympathetic nerves and the adrenal gland medulla) are vasoconstrictive acting on alpha 1-adrenergic receptors. However, the arterioles of skeletal muscle, cardiac muscle, and pulmonary circulation vasodilate in response to these hormones when they act on beta-adrenergic receptors. Generally, stretch and high oxygen tension increase tone, and carbon dioxide and low pH promote vasodilation. Pulmonary arterioles are a noteworthy exception as they vasodilate in response to high oxygen. Brain arterioles are particularly sensitive to pH with reduced pH promoting vasodilation. A number of hormones influence arteriole tone such as angiotensin II (vasoconstrictive), endothelin (vasoconstrictive), bradykinin (vasodilation), atrial natriuretic peptide (vasodilation), and prostacyclin (vasodilation).
Clinical significance
[edit]Arteriole diameters decrease with age and with exposure toair pollution.[5] [6]
Disease
[edit]
Any pathology which constricts blood flow, such asstenosis,will increase total peripheral resistance and lead tohypertension.
Arteriosclerosis
[edit]Arteriolosclerosis is the term specifically used for the hardening of arteriole walls. This can be due to decreased elastic production from fibrinogen, associated withageing,orhypertensionor pathological conditions such asatherosclerosis.
Arteritis
[edit]Arteritis of the arterioles occurs when the arteriole walls becomeinflamedas a result of either an immune response to infection or anautoimmuneresponse.
This sectionneeds expansion.You can help byadding to it.(December 2013) |
Medication
[edit]The muscular contraction of arterioles is targeted by drugs that lower blood pressure (antihypertensives), for example thedihydropyridines(nifedipineandnicardipine), which block thecalcium conductancein the muscular layer of the arterioles, causing relaxation.
This decreases the resistance to flow into peripheral vascular beds, lowering overall systemic pressure.
Metarterioles
[edit]A "metarteriole"is an arteriole which bypasses capillary circulation.[7]
See also
[edit]References
[edit]- ^Maton, Anthea; Jean Hopkins; Charles William McLaughlin; Susan Johnson; Maryanna Quon Warner; David LaHart; Jill D. Wright (1993).Human Biology and Health.Englewood Cliffs, New Jersey: Prentice Hall.ISBN0-13-981176-1.
- ^Rahman, Masum; Abu Bakar, Siddik (4 December 2021).StatPearls [Internet](Updated ed.). Treasure Island (FL): StatPearls Publishing. pp. 2–5.PMID32310381.Retrieved17 November2022.
- ^Riva, CE; Grunwald, JE; Petrig, BL (1986). "Autoregulation of human retinal blood flow. An investigation with laser Doppler velocimetry".Invest Ophthalmol Vis Sci.27(12): 1706–1712.PMID2947873.
- ^Johnson, P. C. (1986). Autoregulation of blood flow. In Circulation Research (Vol. 59, Issue 5, pp. 483–495). Ovid Technologies (Wolters Kluwer Health).https://doi.org/10.1161/01.res.59.5.483
- ^Adar, SD; Klein, R; Klein, BE; Szpiro, AA; Cotch, MF (2010)."Air Pollution and the microvasculature: a crosssectional assessment of in vivo retinal images in the population based multiethnic study of atherosclerosis (MESA)".PLOS Med.7(11): e1000372.doi:10.1371/journal.pmed.1000372.PMC2994677.PMID21152417.
- ^Louwies, T; Int Panis, L; Kicinski, M; De Boever, P; Nawrot, Tim S (2013)."Retinal Microvascular Responses to Short-Term Changes in Particulate Air Pollution in Healthy Adults".Environmental Health Perspectives.121(9): 1011–6.doi:10.1289/ehp.1205721.PMC3764070.PMID23777785.Archived fromthe originalon 2013-11-02.Retrieved2013-06-26.
- ^Nosek, Thomas M."Section 3/3ch9/s3ch9_2".Essentials of Human Physiology.Archived fromthe originalon 2016-03-24.
