Chylomicron
This articleneeds additional citations forverification.(December 2009) |

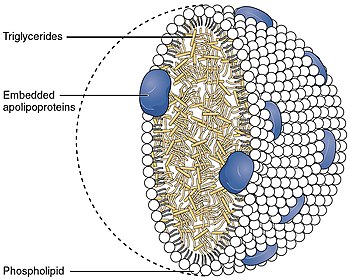
Chylomicrons(from the Greek χυλός,chylos,meaningjuice(of plants or animals), andmicron,meaningsmall),[1]also known asultra low-density lipoproteins(ULDL), arelipoprotein particlesthat consist oftriglycerides(85–92%),phospholipids(6–12%),cholesterol(1–3%), andproteins(1–2%). They transport dietarylipids,such asfatsand cholesterol, from theintestinesto other locations in the body, within the water-based solution of thebloodstream.[2]ULDLs are one of the five major groups lipoproteins are divided into based on theirdensity.A protein specific to chylomicrons isApoB48.
There is an inverse relationship in the density and size of lipoprotein particles: fats have a lower density than water or smaller protein molecules, and the larger particles have a higher ratio of internal fat molecules with respect to the outeremulsifyingprotein molecules in the shell. ULDLs, if in the region of 1,000 nm or more, are the only lipoprotein particles that can be seen using a light microscope, at maximum magnification. All the other classes are submicroscopic.
Function
[edit]
ApoA, ApoB, ApoC, ApoE(apolipoproteins);T(triacylglycerol);C(cholesterol); green (phospholipids)
Chylomicrons transport lipids absorbed from the intestine toadipose,cardiac, and skeletal muscle tissue, where their triglyceride components are hydrolyzed by the activity of thelipoprotein lipase,allowing the releasedfree fatty acidsto be absorbed by the tissues. When a large portion of the triglyceride core has been hydrolyzed, chylomicron remnants are formed and are taken up by the liver, thereby also transferring dietary fat to the liver.
Stages
[edit]Nascent chylomicrons
[edit]In the small intestine, dietarytriglyceridesare emulsified by bile and digested bypancreatic lipases,resulting in the formation ofmonoglyceridesandfatty acids.These lipids are absorbed intoenterocytesviapassive diffusion.Inside these cells, monoglycerides and fatty acids are transported to thesmooth endoplasmic reticulum(smooth ER), where they are re-esterified to form triglycerides.[3]These triglycerides, along with phospholipids and cholesterol, are added toapolipoprotein B48to form nascent chylomicrons[4](also referred to asimmature chylomicronsorpre-chylomicrons).
After synthesis in the smooth ER, nascent chylomicrons are transported to theGolgi apparatusbySAR1Bproteins.[5]The transport of nascent chylomicrons within the secretory pathway is facilitated by protein transport vesicles (PCTVs). PCTVs are uniquely equipped withv-SNAREandVAMP-7proteins, which aid in their fusion with the cis-Golgi compartment. This transport is facilitated byCOPIIproteins, including Sec23/24, which select cargo and facilitate vesicle budding from the ER membrane.[6]
During transit through the Golgi, nascent chylomicrons undergo enzymatic modification and lipidation processes, resulting in the formation ofmature chylomicrons.
Mature chylomicrons
[edit]Mature chylomicrons are released through thebasolateral membraneofenterocytes(via thesecretory pathway) intolacteals,[7]lymphatic capillariesin thevilliof thesmall intestine.Lymphthat contains chylomicrons (and other emulsified fats) is referred to aschyle.Thelymphatic circulationcarries chyle to thelymphatic ductsbefore it enters thevenous returnof the systemiccirculationviasubclavian veins.From here, chylomicrons can supply tissue throughout the body with fat absorbed from the diet.[8]Because they enter the bloodstream in this way, digested lipids (in the form of chylomicrons) bypass thehepatic portal systemand thus avoidfirst pass metabolism,unlike digestedcarbohydrates(in the form ofmonosaccharides) andproteins(in the form ofamino acids).
While circulating in blood,high-density lipoproteins(HDLs) donate essential components includingapolipoprotein C-II(APOC2) andapolipoprotein E(APOE) to the mature chylomicron. APOC2 is a crucial coenzyme for the activity oflipoprotein lipase(LPL), which hydrolyzes triglycerides within chylomicrons.
Chylomicron remnants
[edit]Once triglyceride stores are distributed, chylomicrons return APOC2 toHDLswhile retaining APOE, transforming into a chylomicron remnant. ApoB48 and APOE are important to identify the chylomicron remnant in the liver for endocytosis and breakdown.
Pathology
[edit]Hyperchylomicronemia
[edit]Hyperchylomicronemia is characterized by an excessive presence of chylomicrons in the blood, leading to extremehypertriglyceridemia.Clinical manifestations of this disorder includeeruptive xanthomas,lipaemia retinalis,hepatosplenomegaly,recurrentabdominal pain,andacute pancreatitis.This condition can be caused by genetic mutations (see below) or secondary factors such asuncontrolled diabetesoralcohol use disorder.[9]
Hypochylomicronemia
[edit]Hypochylomicronemia refers to abnormally low levels or complete absence of chylomicrons in the blood, particularly after a meal (postprandial). This condition can result from genetic mutations (see below), as well as certain malabsorption syndromes or deficiencies in dietary fat intake.[9]
Related disorders
[edit]Chylomicron remnants and cardiovascular disease
[edit]Chylomicron remnants are the lipoprotein particles left after chylomicrons have delivered triglycerides to tissues. Elevated levels of these remnants contribute tohyperlipidemia,which is considered an important risk factor forcardiovascular disease.[9]
Recent studies have demonstrated that chylomicron remnants can penetrate thetunica intimaand become trapped in the subendothelial space. This process enhances the deposition of cholesterol in the arterial wall, which is a critical step in the formation ofatherosclerotic plaques.The retention and modification of these remnants within the arterial wall triggerinflammatory responses,further accelerating the development ofatherosclerosis.[10]
Related genetic disorders
[edit]Abetalipoproteinemia (ABL)
[edit]Abetalipoproteinemia(ABL; OMIM 200100) is a rareautosomal recessivedisorder caused by mutations in both alleles of theMTP gene.This genetic defect leads to nearly undetectable levels of ApoB and very low plasma cholesterol levels. Patients with ABL exhibit fat malabsorption,steatorrhea,and fat accumulation in enterocytes and hepatocytes. The condition also results in multiple vitamin deficiencies (E, A, K, and D) due to impaired lipoprotein assembly and transport. If untreated, ABL can cause neurological disturbances such as spinal-cerebellar degeneration,peripheral neuropathies,andretinitis pigmentosa.Early supplementation of fat-soluble vitamins can prevent these complications.[11]
Homozygous hypobetalipoproteinemia (Ho-HBL)
[edit]Homozygous hypobetalipoproteinemia(Ho-HBL; OMIM 107730) is an extremely rare inherited disorder characterized by improper packaging and secretion of apoB-containing lipoproteins due to mutations in both alleles of theAPOB gene.These mutations lead to apoB truncations or amino acid substitutions, resulting in the formation of short, abnormal apoBs that are unable to bind lipids and form chylomicrons. Clinical manifestations vary, ranging from lack of symptoms to features overlapping with those of ABL, including fat malabsorption and vitamin deficiencies.[11]
Chylomicron retention disease (CMRD)
[edit]Chylomicron retention disease(CMRD; OMIM #607689) is a rareautosomal recessivedisorder caused by mutations in theSAR1B gene.Patients with CMRD present with chronic diarrhea, failure to thrive, hypocholesterolemia, and low levels of fat-soluble vitamins. The enterocytes of these patients fail to secrete chylomicrons into the lymph, leading to lipid accumulation and characteristic mucosal changes in the small intestine. Unlike ABL and Ho-HBL, CMRD does not cause acanthocytosis, retinitis pigmentosa, or severe neurological symptoms.[11]
Familial chylomicronemia syndrome (FCS)
[edit]Familial chylomicronemia syndrome(FCS), also known asType I hyperlipoproteinemia,is characterized by massivehypertriglyceridemia,abdominal pain, pancreatitis,eruptive xanthomas,andhepatosplenomegaly.This condition is caused by mutations in genes such as LPL, APOC-II, APOA-V, LMF1, and GPIHBP1, which are involved in the regulation of triglyceride-rich lipoprotein catabolism. Patients with FCS show significantly elevated fasting concentrations of chylomicrons and do not typically develop premature atherosclerosis due to the large size of chylomicrons preventing their traversal through the vascular endothelial barrier. Diagnosis is confirmed by DNA sequencing for pathogenic mutations in these genes.[11]
References
[edit]- ^"Definition of CHYLOMICRONS".www.merriam-webster.com.Retrieved2024-04-26.
- ^Gofman, John W.; Jones, Hardin B.; Lindgren, Frank T.; Lyon, Thomas P.; Elliott, Harold A.; Strisower, Beverly (1950)."Blood Lipids and Human Atherosclerosis"(PDF).Circulation.2(2): 161–178.doi:10.1161/01.cir.2.2.161.PMID15427204.S2CID402420.
- ^Schwenk, Robert W.; Holloway, Graham P.; Luiken, Joost J. F. P.; Bonen, Arend; Glatz, Jan F. C. (2010-04-01)."Fatty acid transport across the cell membrane: Regulation by fatty acid transporters".Prostaglandins, Leukotrienes and Essential Fatty Acids.82(4): 149–154.doi:10.1016/j.plefa.2010.02.029.ISSN0952-3278.PMID20206486.
- ^Kiani, Reza (2018-01-01), Maleki, Majid; Alizadehasl, Azin; Haghjoo, Majid (eds.),"Chapter 18 - Dyslipidemia",Practical Cardiology,Elsevier, pp. 303–309,doi:10.1016/b978-0-323-51149-0.00018-3,ISBN978-0-323-51149-0,retrieved2022-12-06
- ^"SAR1B gene: MedlinePlus Genetics".medlineplus.gov.Retrieved2022-12-06.
- ^Giammanco, Antonina; Cefalù, Angelo B.; Noto, Davide; Averna, Maurizio R. (2015-03-20)."The pathophysiology of intestinal lipoprotein production".Frontiers in Physiology.6:61.doi:10.3389/fphys.2015.00061.ISSN1664-042X.PMC4367171.PMID25852563.
- ^Bodewes, Frank A.J.A.; Wouthuyzen-Bakker, Marjan; Verkade, Henkjan J. (2015),"Persistent Fat Malabsorption in Cystic Fibrosis",Diet and Exercise in Cystic Fibrosis,Elsevier, pp. 373–381,doi:10.1016/b978-0-12-800051-9.00041-9,ISBN978-0-12-800051-9,retrieved2024-06-29
- ^Smith, Sareen S. Gropper, Jack L.; Smith, Jack S. (2013).Advanced nutrition and human metabolism(6th ed.). Belmont, CA: Wadsworth/Cengage Learning.ISBN978-1133104056.
{{cite book}}:CS1 maint: multiple names: authors list (link) - ^abcJulve, Josep; Martín-Campos, Jesús M.; Escolà-Gil, Joan Carles; Blanco-Vaca, Francisco (2016)."Chylomicrons: Advances in biology, pathology, laboratory testing, and therapeutics".Clinica Chimica Acta.455:134–148.doi:10.1016/j.cca.2016.02.004.PMID26868089.
- ^Tomkin, Gerald H.; Owens, Daphne (2012)."The Chylomicron: Relationship to Atherosclerosis".International Journal of Vascular Medicine.2012:1–13.doi:10.1155/2012/784536.ISSN2090-2824.PMC3189596.PMID22007304.
- ^abcdGiammanco, Antonina; Cefalù, Angelo B.; Noto, Davide; Averna, Maurizio R. (2015-03-20)."The pathophysiology of intestinal lipoprotein production".Frontiers in Physiology.6:61.doi:10.3389/fphys.2015.00061.ISSN1664-042X.PMC4367171.PMID25852563.