Urinary tract infection
| Urinary tract infection | |
|---|---|
| Other names | Acute cystitis, simple cystitis, bladder infection, symptomatic bacteriuria |
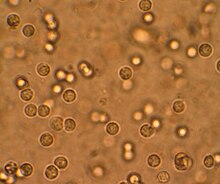 | |
| Multiplewhite cellsseen in the urine of a person with a urinary tract infection usingmicroscopy | |
| Specialty | Infectious disease,Urology |
| Symptoms | Pain withurination,frequent urination, feeling the need to urinate despite having an empty bladder[1] |
| Causes | Most oftenEscherichia coli[2] |
| Risk factors | Catheterisation (foley catheter), female anatomy, sexual intercourse,diabetes,obesity,family history[2] |
| Diagnostic method | Based on symptoms,urine culture[3][4] |
| Differential diagnosis | Vulvovaginitis,urethritis,pelvic inflammatory disease,interstitial cystitis,[5]kidney stone disease[6] |
| Treatment | Antibiotics(nitrofurantoinortrimethoprim/sulfamethoxazole)[7] |
| Frequency | 152million (2015)[8] |
| Deaths | 196,500 (2015)[9] |
Aurinary tract infection(UTI) is aninfectionthat affects a part of theurinary tract.[1]Lower urinary tract infections may involve the bladder (cystitis) or urethra (urethritis) while upper urinary tract infections affect the kidney (pyelonephritis).[10]Symptoms from a lower urinary tract infection includesuprapubicpain, painful urination (dysuria), frequency and urgency of urination despite having an empty bladder.[1]Symptoms of a kidney infection, on the other hand, are more systemic and includefeverorflank painusually in addition to the symptoms of a lower UTI.[10]Rarely, the urine may appearbloody.[7]Symptoms may be vague or non-specific at the extremities of age (i.e. in patients who are very young or old).[1][11]
The most common cause of infection isEscherichia coli,though other bacteria orfungimay sometimes be the cause.[2]Risk factors include female anatomy, sexual intercourse,diabetes,obesity,catheterisation, and family history.[2]Although sexual intercourse is a risk factor, UTIs are not classified assexually transmitted infections(STIs).[12]Pyelonephritisusually occurs due to an ascending bladder infection but may also result from ablood-borne bacterial infection.[13]Diagnosis in young healthy women can be based on symptoms alone.[4]In those with vague symptoms, diagnosis can be difficult because bacteria may be present without there being an infection.[14]In complicated cases or if treatment fails, aurine culturemay be useful.[3]
In uncomplicated cases, UTIs are treated with a short course ofantibioticssuch asnitrofurantoinortrimethoprim/sulfamethoxazole.[7]Resistanceto many of the antibiotics used to treat this condition is increasing.[1]In complicated cases, a longer course orintravenousantibiotics may be needed.[7]If symptoms do not improve in two or three days, further diagnostic testing may be needed.[3]Phenazopyridinemay help with symptoms.[1]In those who have bacteria or white blood cells in their urine but have no symptoms, antibiotics are generally not needed,[15]unless they are pregnant.[16]In those with frequent infections, a short course of antibiotics may be taken as soon as symptoms begin or long-term antibiotics may be used as a preventive measure.[17]
About 150million people develop a urinary tract infection in a given year.[2]They are more common in women than men, but similar between anatomies while carryingindwelling catheters.[7][18]In women, they are the most common form of bacterial infection.[19]Up to 10% of women have a urinary tract infection in a given year, and half of women have at least one infection at some point in their lifetime.[4][7]They occur most frequently between the ages of 16 and 35years.[7]Recurrences are common.[7]Urinary tract infections have been described since ancient times with the first documented description in theEbers Papyrusdated to c. 1550 BC.[20]
Signs and symptoms

Lower urinary tract infection is also referred to as a bladder infection. The most common symptoms areburning with urinationand having to urinate frequently (or an urge to urinate) in the absence ofvaginal dischargeand significant pain.[4]These symptoms may vary from mild to severe[10]and in healthy women last an average of sixdays.[19]Some pain above thepubic boneor in thelower backmay be present. People experiencing an upper urinary tract infection, orpyelonephritis,may experienceflank pain,fever,or nausea andvomitingin addition to the classic symptoms of a lower urinary tract infection.[10]Rarely, the urine may appearbloody[7]or contain visiblepus in the urine.[21]
UTIs have been associated with onset or worsening ofdelirium,dementia,andneuropsychiatric disorderssuch asdepressionandpsychosis.However, there is insufficient evidence to determine whether UTI causes confusion.[22][23][24][25]The reasons for this are unknown, but may involve a UTI-mediatedsystemicinflammatory responsewhich affects the brain.[22][23][26][27]Cytokinessuch asinterleukin-6produced as part of the inflammatory response may produceneuroinflammation,in turn affectingdopaminergicand/orglutamatergicneurotransmissionas well as brainglucosemetabolism.[22][23][26][27]
Children
In young children, the only symptom of a urinary tract infection (UTI) may be a fever.[28]Because of the lack of more obvious symptoms, when females under the age of two or uncircumcised males less than a year exhibit a fever, a culture of the urine is recommended by many medical associations.[28]Infants may feed poorly, vomit, sleep more, or show signs ofjaundice.[28]In older children, new onseturinary incontinence(loss of bladder control) may occur.[28]About 1 in 400 infants of one to three months of age with a UTI also havebacterial meningitis.[29]
Elderly
Urinary tract symptoms are frequently lacking in theelderly.[11]The presentations may be vague with incontinence, achange in mental status,or fatigue as the only symptoms,[10]while some present to a health care provider withsepsis,an infection of the blood, as the first symptoms.[7]Diagnosis can be complicated by the fact that many elderly people have preexisting incontinence ordementia.[11]
It is reasonable to obtain a urine culture in those with signs of systemic infection that may be unable to report urinary symptoms, such as when advanceddementiais present.[30]Systemic signs of infection include afeveror increase in temperature of more than 1.1 °C (2.0 °F) from usual, chills, and anincreased white blood cell count.[30]
Cause
UropathogenicE. colifrom the gut is the cause of 80–85% of community-acquired urinary tract infections,[31]withStaphylococcus saprophyticusbeing the cause in 5–10%.[4]Rarely they may be due toviralorfungalinfections.[32]Healthcare-associated urinary tract infections (mostly related tourinary catheterization) involve a much broader range of pathogens including:E. coli(27%),Klebsiella(11%),Pseudomonas(11%), the fungal pathogenCandida albicans(9%), andEnterococcus(7%) among others.[7][33][34]Urinary tract infections due toStaphylococcus aureustypically occur secondary to blood-borne infections.[10]Chlamydia trachomatisandMycoplasma genitaliumcan infect the urethra but not the bladder.[35]These infections are usually classified as aurethritisrather than urinary tract infection.[36]
Intercourse
In young sexually active women, sexual activity is the cause of 75–90% of bladder infections, with the risk of infection related to the frequency of sex.[4]The term "honeymoon cystitis" has been applied to this phenomenon of frequent UTIs during early marriage. Inpost-menopausalwomen, sexual activity does not affect the risk of developing a UTI.[4]Spermicideuse, independent of sexual frequency, increases the risk of UTIs.[4]Diaphragmuse is also associated.[37]Condom use without spermicide or use ofbirth control pillsdoes not increase the risk of uncomplicated urinary tract infection.[4][38]
Sex
Women are more prone to UTIs than men because, in females, theurethrais much shorter and closer to theanus.[39]As a woman's estrogen levels decrease withmenopause,her risk of urinary tract infections increases due to the loss of protectivevaginal flora.[39]Additionally,vaginal atrophythat can sometimes occur after menopause is associated with recurrent urinary tract infections.[40]
Chronic prostatitis in the forms ofchronic prostatitis/chronic pelvic pain syndromeandchronic bacterial prostatitis(not acute bacterial prostatitis orasymptomatic inflammatory prostatitis) may cause recurrent urinary tract infections in males. Risk of infections increases as males age. While bacteria is commonly present in the urine of older males this does not appear to affect the risk of urinary tract infections.[41]
Urinary catheters
Urinary catheterizationincreases the risk for urinary tract infections. The risk ofbacteriuria(bacteria in the urine) is between three and six percent per day and prophylactic antibiotics are not effective in decreasing symptomatic infections.[39]The risk of an associated infection can be decreased by catheterizing only when necessary, usingaseptic techniquefor insertion, and maintaining unobstructed closed drainage of the catheter.[42][43][44]
Malescuba diversusingcondom cathetersand female divers using external catching devices for theirdry suitsare also susceptible to urinary tract infections.[45]
Others
A predisposition for bladder infections may run in families.[4]This is believed to be related to genetics.[4]Other risk factors includediabetes,[4]beinguncircumcised,[46][47]and having alarge prostate.[10]In children UTIs are associated withvesicoureteral reflux(an abnormal movement ofurinefrom thebladderintouretersorkidneys) andconstipation.[28]
Persons withspinal cord injuryare at increased risk for urinary tract infection in part because of chronic use of catheter, and in part because ofvoidingdysfunction.[48]It is the most common cause of infection in this population, as well as the most common cause of hospitalization.[48]
Pathogenesis
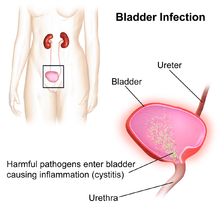
Thebacteriathat cause urinary tract infections typically enter the bladder via the urethra. However, infection may also occur via the blood orlymph.[7]It is believed that the bacteria are usually transmitted to the urethra from the bowel, with females at greater risk due to their anatomy.[7]After gaining entry to the bladder,E. Coliare able to attach to the bladder wall and form abiofilmthat resists the body's immune response.[7]
Escherichia coliis the single most common microorganism, followed byKlebsiellaandProteusspp.,to cause urinary tract infection.KlebsiellaandProteusspp., are frequently associated with stone disease. The presence of Gram positive bacteria such asEnterococcusandStaphylococcusis increased.[49]
The increased resistance of urinary pathogens toquinolone antibioticshas been reported worldwide and might be the consequence of overuse and misuse of quinolones.[49]
Diagnosis
In straightforward cases, a diagnosis may be made and treatment given based on symptoms alone without further laboratory confirmation.[4]In complicated or questionable cases, it may be useful to confirm the diagnosis viaurinalysis,looking for the presence ofurinary nitrites,white blood cells(leukocytes), orleukocyte esterase.[50]Another test,urine microscopy,looks for the presence ofred blood cells,white blood cells, or bacteria. Urinecultureis deemed positive if it shows a bacterial colony count of greater than or equal to 103colony-forming unitsper mL of a typical urinary tract organism. Antibiotic sensitivity can also be tested with these cultures, making them useful in the selection of antibiotic treatment. However, women with negative cultures may still improve with antibiotic treatment.[4]As symptoms can be vague and without reliable tests for urinary tract infections, diagnosis can be difficult in the elderly.[11]
Based on pH
Normal urine pH is slightly acidic, with usual values of 6.0 to 7.5, but the normal range is 4.5 to 8.0. A urine pH of 8.5 or 9.0 is indicative of a urea-splitting organism, such as Proteus, Klebsiella, or Ureaplasma urealyticum; therefore, an asymptomatic patient with a high pH means UTI regardless of the other urine test results. Alkaline pH also can signify struvite kidney stones, which are also known as "infection stones".[6]
Classification
A urinary tract infection may involve only the lower urinary tract, in which case it is known as a bladder infection. Alternatively, it may involve the upper urinary tract, in which case it is known as pyelonephritis. If the urine contains significant bacteria but there are no symptoms, the condition is known asasymptomatic bacteriuria.[10]If a urinary tract infection involves the upper tract, and the person hasdiabetes mellitus,is pregnant, is male, orimmunocompromised,it is considered complicated.[7][19]Otherwise if a woman is healthy andpremenopausalit is considered uncomplicated.[19]In children when a urinary tract infection is associated with a fever, it is deemed to be an upper urinary tract infection.[28]
Children
To make the diagnosis of a urinary tract infection in children, a positive urinary culture is required. Contamination poses a frequent challenge depending on the method of collection used, thus a cutoff of 105CFU/mL is used for a "clean-catch" mid stream sample, 104CFU/mL is used for catheter-obtained specimens, and 102CFU/mL is used forsuprapubic aspirations(a sample drawn directly from the bladder with a needle). The use of "urine bags" to collect samples is discouraged by theWorld Health Organizationdue to the high rate of contamination when cultured, and catheterization is preferred in those not toilet trained. Some, such as theAmerican Academy of Pediatricsrecommendsrenal ultrasoundandvoiding cystourethrogram(watching a person's urethra and urinary bladder with real time x-rays while they urinate) in all children less than two years old who have had a urinary tract infection. However, because there is a lack of effective treatment if problems are found, others such as theNational Institute for Health and Care Excellenceonly recommends routine imaging in those less than six months old or who have unusual findings.[28]
Differential diagnosis
In women withcervicitis(inflammation of thecervix) orvaginitis(inflammation of thevagina) and in young men with UTI symptoms, aChlamydia trachomatisorNeisseria gonorrhoeaeinfection may be the cause.[10][51]These infections are typically classified as aurethritisrather than a urinary tract infection. Vaginitis may also be due to ayeast infection.[52]Interstitial cystitis(chronic pain in the bladder) may be considered for people who experience multiple episodes of UTI symptoms but urine cultures remain negative and not improved with antibiotics.[53]Prostatitis(inflammation of theprostate) may also be considered in the differential diagnosis.[54]
Hemorrhagic cystitis,characterized byblood in the urine,can occur secondary to a number of causes including: infections,radiation therapy,underlying cancer, medications and toxins.[55]Medications that commonly cause this problem include thechemotherapeutic agentcyclophosphamidewith rates of 2–40%.[55]Eosinophilic cystitisis a rare condition whereeosinophilesare present in the bladder wall.[56]Signs and symptoms are similar to a bladder infection.[56]Its cause is not entirely clear; however, it may be linked tofood allergies,infections,and medications among others.[57]
Prevention
A number of measures have not been confirmed to affect UTI frequency including: urinating immediately after intercourse, the type of underwear used, personal hygiene methods used after urinating ordefecating,or whether a person typically bathes or showers.[4]There is similarly a lack of evidence surrounding the effect of holding one's urine,tamponuse, anddouching.[39]In those with frequent urinary tract infections who usespermicideor adiaphragmas a method of contraception, they are advised to use alternative methods.[7]In those withbenign prostatic hyperplasiaurinating in a sitting position appears to improve bladder emptying[58]which might decrease urinary tract infections in this group.[citation needed]
Using urinary catheters as little and as short of time as possible and appropriate care of the catheter when used preventscatheter-associated urinary tract infections.[42]They should be inserted using sterile technique in hospital however non-sterile technique may be appropriate in those who self catheterize.[44]The urinary catheter set up should also be kept sealed.[44]Evidence does not support a significant decrease in risk when silver-alloy catheters are used.[59]
Medications

For those with recurrent infections, taking a short course of antibiotics when each infection occurs is associated with the lowest antibiotic use.[17]A prolonged course of daily antibiotics is also effective.[4]Medications frequently used includenitrofurantoinandtrimethoprim/sulfamethoxazole.[7]Some recommend against prolonged use due to concerns ofantibiotic resistance.[17]Methenamineis another agent used for this purpose as in the bladder where the acidity is low it producesformaldehydeto which resistance does not develop.[60]A UK study showed that methenamine is as effective daily low-dose antibiotics at preventing UTIs among women who experience recurrent UTIs. As methenamine is an antiseptic, it may avoid the issue of antibiotic resistance.[61][62]
In cases where infections are related to intercourse, taking antibiotics afterwards may be useful.[7]In post-menopausal women,topicalvaginalestrogenhas been found to reduce recurrence.[63][64]As opposed to topical creams, the use of vaginal estrogen frompessarieshas not been as useful as low dose antibiotics.[64]Antibiotics following short term urinary catheterization decreases the subsequent risk of a bladder infection.[65]A number ofUTI vaccinesare in development as of 2018.[66][67]
Children
The evidence thatpreventiveantibiotics decrease urinary tract infections in children is poor.[68]However recurrent UTIs are a rare cause of further kidney problems if there are no underlying abnormalities of the kidneys, resulting in less than a third of a percent (0.33%) ofchronic kidney diseasein adults.[69]
Male circumcision
Circumcisionof boys has been observed to exhibit a strong protective effect against UTIs, with some research suggesting as much as a 90% reduction in symptomatic UTI incidence among male infants, if they are circumcised.[70][71]The protective effect is even stronger in boys born with urogenital abnormalities.[71]
Dietary supplements
When used as anadjuvantto antibiotics and other standard treatments,cranberrysupplements decrease the number of UTIs in people who get them frequently.[63][72][73]A 2023 review concluded that cranberry products can reduce the risk of UTIs in certain groups (women with reoccurring UTIs, children, and people having had clinical interventions), but not in pregnant women, the elderly or people withurination disorders.[74]Some evidence suggests that cranberry juice is more effective at UTI control than dehydrated tablets or capsules.[73]Cranberry has not been effective in attempts to replace antibiotics for the treatment of active infections.[75]Cranberry supplements are also high in sugar content, which may worsen the risks associated with UTIs in patients withdiabetes mellitus.[76]
As of 2015,probioticsrequire further study to determine if they are beneficial for UTI.[77]
Treatment
The mainstay of treatment isantibiotics.Phenazopyridineis occasionally prescribed during the first few days in addition to antibiotics to help with the burning and urgency sometimes felt during a bladder infection.[78]However, it is not routinely recommended due to safety concerns with its use, specifically an elevated risk ofmethemoglobinemia(higher than normal level ofmethemoglobinin the blood).[79]Paracetamolmay be used for fevers.[80]There is no good evidence for the use of cranberry products for treating current infections.[81][82]
Fosfomycincan be used as an effective treatment for both UTIs and complicated UTIs including acute pyelonephritis.[83]The standard regimen for complicated UTIs is an oral 3g dose administered once every 48 or 72 hours for a total of 3 doses or a 6 grams every 8 hours for 7 days to 14 days when fosfomycin is given in IV form.[83]
Uncomplicated
Uncomplicated infections can be diagnosed and treated based on symptoms alone.[4]Antibiotics taken by mouth such as trimethoprim/sulfamethoxazole, nitrofurantoin, orfosfomycinare typically first line.[84]Cephalosporins,amoxicillin/clavulanic acid,or afluoroquinolonemay also be used.[85]However,antibiotic resistanceto fluoroquinolones among the bacteria that cause urinary infections has been increasing.[50]TheFood and Drug Administration(FDA) recommends against the use of fluoroquinolones, including aBoxed Warning,when other options are available due to higher risks of serious side effects, such astendinitis,tendon ruptureand worsening ofmyasthenia gravis.[86]These medications substantially shorten the time to recovery with all being equally effective.[85][87]A three-day treatment with trimethoprim/sulfamethoxazole, or a fluoroquinolone is usually sufficient, whereas nitrofurantoin requires 5–7days.[4][88]Fosfomycin may be used as a single dose but is not as effective.[50]
Fluoroquinolones are not recommended as a first treatment.[50][89]TheInfectious Diseases Society of Americastates this due to the concern of generating resistance to this class of medication.[88]Amoxicillin-clavulanateappears less effective than other options.[90]Despite this precaution, some resistance has developed to all of these medications related to their widespread use.[4]Trimethoprim alone is deemed to be equivalent to trimethoprim/sulfamethoxazole in some countries.[88]For simple UTIs, children often respond to a three-day course of antibiotics.[91]Women with recurrent simple UTIs are over 90% accurate in identifying new infections.[4]They may benefit from self-treatment upon occurrence of symptoms with medical follow-up only if the initial treatment fails.[4]
Complicated
Complicated UTIs are more difficult to treat and usually requires more aggressive evaluation, treatment, and follow-up.[92]It may require identifying and addressing the underlying complication.[93]Increasing antibiotic resistance is causing concern about the future of treating those with complicated and recurrent UTI.[94][95][96]
Asymptomatic bacteriuria
Those who have bacteria in the urine but no symptoms should not generally be treated with antibiotics.[97]This includes those who are old, those with spinal cord injuries, and those who have urinary catheters.[98][99]Pregnancy is an exception and it is recommended that women take sevendays of antibiotics.[100][101]If not treated it causes up to 30% of mothers to developpyelonephritisand increases risk oflow birth weightandpreterm birth.[102]Some also support treatment of those withdiabetes mellitus[103]and treatment before urinary tract procedures which will likely cause bleeding.[99]
Pregnant women
Urinary tract infections, even asymptomatic presence of bacteria in the urine, are more concerning in pregnancy due to the increased risk of kidney infections.[39]During pregnancy, highprogesteronelevels elevate the risk of decreased muscle tone of the ureters and bladder, which leads to a greater likelihood of reflux, where urine flows back up the ureters and towards the kidneys.[39]While pregnant women do not have an increased risk of asymptomatic bacteriuria, if bacteriuria is present they do have a 25–40% risk of a kidney infection.[39]Thus if urine testing shows signs of an infection—even in the absence of symptoms—treatment is recommended.[102][101]Cephalexinor nitrofurantoin are typically used because they are generally considered safe in pregnancy.[101]A kidney infection during pregnancy may result inpreterm birthorpre-eclampsia(a state ofhigh blood pressureand kidney dysfunction during pregnancy that can lead toseizures).[39]Some women have UTIs that keep coming back in pregnancy.[104]There is insufficient research on how to best treat these recurrent infections.[104]
Pyelonephritis
Pyelonephritisis treated more aggressively than a simple bladder infection using either a longer course of oral antibiotics orintravenousantibiotics.[3]Seven days of the oral fluoroquinoloneciprofloxacinis typically used in areas where the resistance rate is less than 10%. If the local antibiotic resistance rates are greater than 10%, a dose of intravenousceftriaxoneis often prescribed.[3]Trimethoprim/sulfamethoxazole or amoxicillin/clavulanate orally for 14 days is another reasonable option.[105]In those who exhibit more severe symptoms, admission to a hospital for ongoing antibiotics may be needed.[3]Complications such as ureteral obstruction from akidney stonemay be considered if symptoms do not improve following two or three days of treatment.[10][3]
Prognosis
With treatment, symptoms generally improve within 36hours.[19]Up to 42% of uncomplicated infections may resolve on their own within a few days or weeks.[4][106]
15–25% of adults and children have chronic symptomatic UTIs including recurrent infections, persistent infections (infection with the same pathogen), a re-infection (new pathogen), or a relapsed infection (the same pathogen causes a new infection after it was completely gone).[107]Recurrent urinary tract infections are defined as at least two infections (episodes) in a six-month time period or three infections in twelve months, can occur in adults and in children.[107]
Cystitis refers to a urinary tract infection that involves the lower urinary tract (bladder). An upper urinary tract infection which involves the kidney is calledpyelonephritis.About 10–20% of pyelonephritis will go on and develop scarring of the affected kidney. Then, 10–20% of those develop scarring will have increased risk of hypertension in later life.[108]
Epidemiology
Urinary tract infections are the most frequent bacterial infection in women.[19]They occur most frequently between the ages of 16 and 35years, with 10% of women getting an infection yearly and more than 40–60% having an infection at some point in their lives.[7][4]Recurrences are common, with nearly half of people getting a second infection within a year. Urinary tract infections occur four times more frequently in females than males.[7]Pyelonephritis occurs between 20 and 30 times less frequently.[4]They are the most common cause ofhospital-acquired infectionsaccounting for approximately 40%.[109]Rates of asymptomatic bacteria in the urine increase with age from two to seven percent in women of child-bearing age to as high as 50% in elderly women in care homes.[39]Rates of asymptomatic bacteria in the urine among men over 75 are between 7–10%.[11]2–10% of pregnant women have asymptomatic bacteria in the urine and higher rates are reported in women who live in some underdeveloped countries.[102]
Urinary tract infections may affect 10% of people during childhood.[7]Among children, urinary tract infections are most common in uncircumcised males less than three months of age, followed by females less than one year.[28]Estimates of frequency among children, however, vary widely. In a group of children with a fever, ranging in age between birth and two years, 2–20% were diagnosed with a UTI.[28]
History
Urinary tract infections have been described since ancient times with the first documented description in theEbers Papyrusdated to c. 1550 BC.[20]It was described by the Egyptians as "sending forth heat from the bladder".[110]Effective treatment did not occur until the development and availability of antibiotics in the 1930s before which time herbs,bloodlettingand rest were recommended.[20]
See also
References
- ^abcdef"Urinary Tract Infection".Centers for Disease Control and Prevention(CDC).17 April 2015.Archivedfrom the original on 22 February 2016.Retrieved9 February2016.
- ^abcdeFlores-Mireles AL, Walker JN, Caparon M, Hultgren SJ (May 2015)."Urinary tract infections: epidemiology, mechanisms of infection and treatment options".Nature Reviews. Microbiology.13(5): 269–284.doi:10.1038/nrmicro3432.PMC4457377.PMID25853778.
- ^abcdefgColgan R, Williams M, Johnson JR (September 2011). "Diagnosis and treatment of acute pyelonephritis in women".American Family Physician.84(5): 519–526.PMID21888302.
- ^abcdefghijklmnopqrstuvwxNicolle LE (February 2008). "Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis".The Urologic Clinics of North America.35(1): 1–12, v.doi:10.1016/j.ucl.2007.09.004.PMID18061019.
- ^Caterino JM, Kahan S (2003).In a Page: Emergency medicine.Lippincott Williams & Wilkins. p. 95.ISBN9781405103572.Archivedfrom the original on 24 April 2017.
- ^abBono MJ, Leslie SW, Reygaert WC (2020). "Urinary Tract Infection".Statpearls.PMID29261874.
 Text was copied from this source, which is available under aCreative Commons Attribution 4.0 International LicenseArchived16 October 2017 at theWayback Machine.
Text was copied from this source, which is available under aCreative Commons Attribution 4.0 International LicenseArchived16 October 2017 at theWayback Machine.
- ^abcdefghijklmnopqrstuSalvatore S, Salvatore S, Cattoni E, Siesto G, Serati M, Sorice P, Torella M (June 2011). "Urinary tract infections in women".European Journal of Obstetrics, Gynecology, and Reproductive Biology.156(2): 131–136.doi:10.1016/j.ejogrb.2011.01.028.PMID21349630.
- ^Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (October 2016)."Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015".Lancet.388(10053): 1545–1602.doi:10.1016/S0140-6736(16)31678-6.PMC5055577.PMID27733282.
- ^Wang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (October 2016)."Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015".Lancet.388(10053): 1459–1544.doi:10.1016/S0140-6736(16)31012-1.PMC5388903.PMID27733281.
- ^abcdefghijLane DR, Takhar SS (August 2011). "Diagnosis and management of urinary tract infection and pyelonephritis".Emergency Medicine Clinics of North America.29(3): 539–552.doi:10.1016/j.emc.2011.04.001.PMID21782073.
- ^abcdeWoodford HJ, George J (February 2011)."Diagnosis and management of urinary infections in older people".Clinical Medicine.11(1): 80–83.doi:10.7861/clinmedicine.11-1-80.PMC5873814.PMID21404794.
- ^Study Guide for Pathophysiology(5 ed.). Elsevier Health Sciences. 2013. p. 272.ISBN9780323293181.Archivedfrom the original on 16 February 2016.
- ^Introduction to Medical-Surgical Nursing.Elsevier Health Sciences. 2015. p. 909.ISBN9781455776412.Archivedfrom the original on 11 January 2023.Retrieved17 September2017.
- ^Jarvis WR (2007).Bennett & Brachman's hospital infections(5th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 474.ISBN9780781763837.Archivedfrom the original on 16 February 2016.
- ^Ferroni M, Taylor AK (November 2015). "Asymptomatic Bacteriuria in Noncatheterized Adults".The Urologic Clinics of North America.42(4): 537–545.doi:10.1016/j.ucl.2015.07.003.PMID26475950.
- ^Glaser AP, Schaeffer AJ (November 2015). "Urinary Tract Infection and Bacteriuria in Pregnancy".The Urologic Clinics of North America.42(4): 547–560.doi:10.1016/j.ucl.2015.05.004.PMID26475951.
- ^abc"Recurrent uncomplicated cystitis in women: allowing patients to self-initiate antibiotic therapy".Prescrire International.23(146): 47–49. February 2014.PMID24669389.
- ^Lee JH, Kim SW, Yoon BI, Ha US, Sohn DW, Cho YH (January 2013)."Factors that affect nosocomial catheter-associated urinary tract infection in intensive care units: 2-year experience at a single center".Korean Journal of Urology.54(1): 59–65.doi:10.4111/kju.2013.54.1.59.PMC3556556.PMID23362450.
- ^abcdefColgan R, Williams M (October 2011). "Diagnosis and treatment of acute uncomplicated cystitis".American Family Physician.84(7): 771–776.PMID22010614.
- ^abcAl-Achi A (2008).An introduction to botanical medicines: history, science, uses, and dangers.Westport, Conn.: Praeger Publishers. p. 126.ISBN978-0-313-35009-2.Archivedfrom the original on 28 May 2016.
- ^Arellano RS (19 January 2011).Non-vascular interventional radiology of the abdomen.New York: Springer. p. 67.ISBN978-1-4419-7731-1.Archivedfrom the original on 10 June 2016.
- ^abcChae JH, Miller BJ (November 2015). "Beyond Urinary Tract Infections (UTIs) and Delirium: A Systematic Review of UTIs and Neuropsychiatric Disorders".Journal of Psychiatric Practice.21(6): 402–411.doi:10.1097/PRA.0000000000000105.PMID26554322.S2CID24455646.
- ^abcKrinitski D, Kasina R, Klöppel S, Lenouvel E (November 2021)."Associations of delirium with urinary tract infections and asymptomatic bacteriuria in adults aged 65 and older: A systematic review and meta-analysis".Journal of the American Geriatrics Society.69(11): 3312–3323.doi:10.1111/jgs.17418.PMC9292354.PMID34448496.
- ^Balogun SA, Philbrick JT (March 2014)."Delirium, a Symptom of UTI in the Elderly: Fact or Fable? A Systematic Review".Canadian Geriatrics Journal.17(1): 22–26.doi:10.5770/cgj.17.90.PMC3940475.PMID24596591.
- ^Mayne S, Bowden A, Sundvall PD, Gunnarsson R (February 2019)."The scientific evidence for a potential link between confusion and urinary tract infection in the elderly is still confusing - a systematic literature review".BMC Geriatrics.19(1): 32.doi:10.1186/s12877-019-1049-7.PMC6360770.PMID30717706.
- ^abRashid MH, Sparrow NA, Anwar F, Guidry G, Covarrubias AE, Pang H, et al. (October 2021)."Interleukin-6 mediates delirium-like phenotypes in a murine model of urinary tract infection".Journal of Neuroinflammation.18(1): 247.doi:10.1186/s12974-021-02304-x.PMC8554965.PMID34711238.
- ^abJiang Z, Liang F, Zhang Y, Dong Y, Song A, Zhu X, et al. (September 2022)."Urinary Catheterization Induces Delirium-Like Behavior Through Glucose Metabolism Impairment in Mice".Anesthesia and Analgesia.135(3): 641–652.doi:10.1213/ANE.0000000000006008.PMC9388475.PMID35389369.
- ^abcdefghiBhat RG, Katy TA, Place FC (August 2011). "Pediatric urinary tract infections".Emergency Medicine Clinics of North America.29(3): 637–653.doi:10.1016/j.emc.2011.04.004.PMID21782079.
- ^Nugent J, Childers M, Singh-Miller N, Howard R, Allard R, Eberly M (September 2019). "Risk of Meningitis in Infants Aged 29 to 90 Days with Urinary Tract Infection: A Systematic Review and Meta-Analysis".The Journal of Pediatrics.212:102–110.e5.doi:10.1016/j.jpeds.2019.04.053.PMID31230888.S2CID195327630.
- ^abAMDA – The Society for Post-Acute and Long-Term Care Medicine(February 2014),"Ten Things Physicians and Patients Should Question",Choosing Wisely:an initiative of theABIM Foundation,AMDA – The Society for Post-Acute and Long-Term Care Medicine,archivedfrom the original on 13 September 2014,retrieved20 April2015
- ^Abraham SN, Miao Y (October 2015)."The nature of immune responses to urinary tract infections".Nature Reviews. Immunology.15(10): 655–663.doi:10.1038/nri3887.PMC4926313.PMID26388331.
- ^Amdekar S, Singh V, Singh DD (November 2011). "Probiotic therapy: immunomodulating approach toward urinary tract infection".Current Microbiology.63(5): 484–490.doi:10.1007/s00284-011-0006-2.PMID21901556.S2CID24123416.
- ^Sievert DM, Ricks P, Edwards JR, Schneider A, Patel J, Srinivasan A, et al. (January 2013)."Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2009-2010".Infection Control and Hospital Epidemiology.34(1): 1–14.doi:10.1086/668770.PMID23221186.S2CID7663664.Archivedfrom the original on 16 March 2020.Retrieved2 July2019.
- ^Bagshaw SM, Laupland KB (February 2006). "Epidemiology of intensive care unit-acquired urinary tract infections".Current Opinion in Infectious Diseases.19(1): 67–71.doi:10.1097/01.qco.0000200292.37909.e0.PMID16374221.S2CID23726078.
- ^"Urinary Tract Infections in Adults".Archivedfrom the original on 9 January 2015.Retrieved1 January2015.
- ^Brill JR (April 2010). "Diagnosis and treatment of urethritis in men".American Family Physician.81(7): 873–878.PMID20353145.
- ^Franco AV (December 2005). "Recurrent urinary tract infections".Best Practice & Research. Clinical Obstetrics & Gynaecology.19(6): 861–873.doi:10.1016/j.bpobgyn.2005.08.003.PMID16298166.
- ^Engleberg NC, DiRita V, Dermody TS (2007).Schaechter's Mechanism of Microbial Disease.Baltimore: Lippincott Williams & Wilkins.ISBN978-0-7817-5342-5.
- ^abcdefghiDielubanza EJ, Schaeffer AJ (January 2011)."Urinary tract infections in women".The Medical Clinics of North America.95(1): 27–41.doi:10.1016/j.mcna.2010.08.023.PMID21095409.
- ^Goldstein I, Dicks B, Kim NN, Hartzell R (December 2013)."Multidisciplinary overview of vaginal atrophy and associated genitourinary symptoms in postmenopausal women".Sexual Medicine.1(2): 44–53.doi:10.1002/sm2.17.PMC4184497.PMID25356287.
- ^Holt JD, Garrett WA, McCurry TK, Teichman JM (February 2016). "Common Questions About Chronic Prostatitis".American Family Physician.93(4): 290–296.PMID26926816.
- ^abNicolle LE (May 2001). "The chronic indwelling catheter and urinary infection in long-term-care facility residents".Infection Control and Hospital Epidemiology.22(5): 316–321.doi:10.1086/501908.PMID11428445.S2CID40832193.
- ^Phipps S, Lim YN, McClinton S, Barry C, Rane A, N'Dow J (April 2006). Phipps S (ed.). "Short term urinary catheter policies following urogenital surgery in adults".The Cochrane Database of Systematic Reviews(2): CD004374.doi:10.1002/14651858.CD004374.pub2.PMID16625600.
- ^abcGould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA (April 2010)."Guideline for prevention of catheter-associated urinary tract infections 2009".Infection Control and Hospital Epidemiology.31(4): 319–326.doi:10.1086/651091.PMID20156062.S2CID31266013.Archivedfrom the original on 16 March 2020.Retrieved2 July2019.
- ^Harris R (December 2009)."Genitourinary infection and barotrauma as complications of 'P-valve' use in drysuit divers".Diving and Hyperbaric Medicine.39(4): 210–212.PMID22752741.Archived from the original on 26 May 2013.Retrieved4 April2013.
{{cite journal}}:CS1 maint: unfit URL (link) - ^Jagannath VA, Fedorowicz Z, Sud V, Verma AK, Hajebrahimi S (November 2012). "Routine neonatal circumcision for the prevention of urinary tract infections in infancy".The Cochrane Database of Systematic Reviews.11:CD009129.doi:10.1002/14651858.CD009129.pub2.PMID23152269.
The incidence of urinary tract infection (UTI) is greater in uncircumcised babies
- ^Morris BJ, Wiswell TE (June 2013). "Circumcision and lifetime risk of urinary tract infection: a systematic review and meta-analysis".The Journal of Urology.189(6): 2118–2124.doi:10.1016/j.juro.2012.11.114.PMID23201382.
- ^abEves FJ, Rivera N (April 2010)."Prevention of urinary tract infections in persons with spinal cord injury in home health care".Home Healthcare Nurse.28(4): 230–241.doi:10.1097/NHH.0b013e3181dc1bcb.PMID20520263.S2CID35850310.
- ^abGutierrez-Aceves J (2011). "Preoperative Antibiotics and Prevention of Sepsis in Genitourinary Surgery". In Smith AD, Badlani GH, Preminger GM, Kavoussi LR (eds.).Smith's Textbook of Endourology(3rd ed.). Hoboken, NJ: John Wiley & Sons. p. 39.ISBN978-1-4443-4514-8.
- ^abcdDetweiler K, Mayers D, Fletcher SG (November 2015). "Bacteruria and Urinary Tract Infections in the Elderly".The Urologic Clinics of North America(Review).42(4): 561–568.doi:10.1016/j.ucl.2015.07.002.PMID26475952.
- ^Raynor MC, Carson CC (January 2011). "Urinary infections in men".The Medical Clinics of North America.95(1): 43–54.doi:10.1016/j.mcna.2010.08.015.PMID21095410.
- ^Hui D (15 January 2011). Leung A, Padwal R (eds.).Approach to internal medicine: a resource book for clinical practice(3rd ed.). New York: Springer. p. 244.ISBN978-1-4419-6504-2.Archivedfrom the original on 20 May 2016.
- ^Kursh ED, Ulchaker JC, eds. (2000).Office urology.Totowa, N.J.: Humana Press. p. 131.ISBN978-0-89603-789-2.Archivedfrom the original on 4 May 2016.
- ^Mick NW, Peters JR, Egan D, Nadel ES, Walls R, Silvers S, eds. (2006).Blueprints emergency medicine(2nd ed.). Baltimore, Md.: Lippincott Williams & Wilkins. p. 152.ISBN978-1-4051-0461-6.Archivedfrom the original on 27 May 2016.
- ^abGraham SD, Keane, James TE, Glenn F, eds. (2009).Glenn's urologic surgery(7th ed.). Philadelphia, Pa.: Lippincott Williams & Wilkins. p. 148.ISBN9780781791410.Archivedfrom the original on 24 April 2016.
- ^abBelman AB, King LR, Kramer SA, eds. (2002).Clinical pediatric urology(4. ed.). London: Dunitz. p. 338.ISBN9781901865639.Archivedfrom the original on 15 May 2016.
- ^Popescu OE, Landas SK, Haas GP (February 2009). "The spectrum of eosinophilic cystitis in males: case series and literature review".Archives of Pathology & Laboratory Medicine.133(2): 289–294.doi:10.5858/133.2.289.PMID19195972.
- ^de Jong Y, Pinckaers JH, ten Brinck RM, Lycklama à Nijeholt AA, Dekkers OM (2014)."Urinating standing versus sitting: position is of influence in men with prostate enlargement. A systematic review and meta-analysis".PLOS ONE.9(7): e101320.Bibcode:2014PLoSO...9j1320D.doi:10.1371/journal.pone.0101320.PMC4106761.PMID25051345.
- ^Lam TB, Omar MI, Fisher E, Gillies K, MacLennan S (September 2014)."Types of indwelling urethral catheters for short-term catheterisation in hospitalised adults".The Cochrane Database of Systematic Reviews.2014(9): CD004013.doi:10.1002/14651858.CD004013.pub4.PMC11197149.PMID25248140.
- ^Finkel R, Clark MA, Cubeddu LX (2009).Pharmacology(4th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 397.ISBN9780781771559.Archivedfrom the original on 9 June 2016.
- ^"Methenamine is as good as antibiotics at preventing urinary tract infections".NIHR Evidence.20 December 2022.doi:10.3310/nihrevidence_55378.S2CID254965605.Archivedfrom the original on 20 January 2023.Retrieved20 January2023.
- ^Harding C, Mossop H, Homer T, Chadwick T, King W, Carnell S, et al. (March 2022)."Alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women: multicentre, open label, randomised, non-inferiority trial".BMJ.376:e068229.doi:10.1136/bmj-2021-0068229.PMC8905684.PMID35264408.
- ^abBeerepoot M, Geerlings S (April 2016)."Non-Antibiotic Prophylaxis for Urinary Tract Infections".Pathogens(Review).5(2): 36.doi:10.3390/pathogens5020036.PMC4931387.PMID27092529.
- ^abPerrotta C, Aznar M, Mejia R, Albert X, Ng CW (April 2008). "Oestrogens for preventing recurrent urinary tract infection in postmenopausal women".The Cochrane Database of Systematic Reviews(2): CD005131.doi:10.1002/14651858.CD005131.pub2.PMID18425910.
- ^Marschall J, Carpenter CR, Fowler S, Trautner BW (June 2013)."Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: meta-analysis".BMJ.346:f3147.doi:10.1136/bmj.f3147.PMC3678514.PMID23757735.
- ^Magistro G, Stief CG (January 2019)."Vaccine Development for Urinary Tract Infections: Where Do We Stand?".European Urology Focus.5(1): 39–41.doi:10.1016/j.euf.2018.07.034.PMID30093359.
- ^Huttner A, Gambillara V (October 2018)."The development and early clinical testing of the ExPEC4V conjugate vaccine against uropathogenic Escherichia coli".Clinical Microbiology and Infection.24(10): 1046–1050.doi:10.1016/j.cmi.2018.05.009.PMID29803843.
- ^Dai B, Liu Y, Jia J, Mei C (July 2010). "Long-term antibiotics for the prevention of recurrent urinary tract infection in children: a systematic review and meta-analysis".Archives of Disease in Childhood.95(7): 499–508.doi:10.1136/adc.2009.173112.PMID20457696.S2CID6714180.
- ^Salo J, Ikäheimo R, Tapiainen T, Uhari M (November 2011). "Childhood urinary tract infections as a cause of chronic kidney disease".Pediatrics.128(5): 840–847.doi:10.1542/peds.2010-3520.PMID21987701.S2CID41304559.
- ^Shaikh N, Morone NE, Bost JE, Farrell MH (April 2008)."Prevalence of Urinary Tract Infection in Childhood: A Meta-Analysis".Pediatric Infectious Disease Journal.27(4): 302–308.doi:10.1097/INF.0b013e31815e4122.ISSN0891-3668.PMID18316994.
- ^abDave S, Afshar K, Braga LH, Anderson P (February 2018)."Canadian Urological Association guideline on the care of the normal foreskin and neonatal circumcision in Canadian infants (full version)".Canadian Urological Association Journal.12(2): E76–E99.doi:10.5489/cuaj.5033.ISSN1911-6470.PMC5937400.PMID29381458.
- ^Wang CH, Fang CC, Chen NC, Liu SS, Yu PH, Wu TY, et al. (July 2012). "Cranberry-containing products for prevention of urinary tract infections in susceptible populations: a systematic review and meta-analysis of randomized controlled trials".Archives of Internal Medicine.172(13): 988–996.doi:10.1001/archinternmed.2012.3004.PMID22777630.
- ^abXia Jy, Yang C, Xu Df, Xia H, Yang Lg, Sun Gj (2 September 2021)."Consumption of cranberry as adjuvant therapy for urinary tract infections in susceptible populations: A systematic review and meta-analysis with trial sequential analysis".PLOS ONE.16(9): e0256992.Bibcode:2021PLoSO..1656992X.doi:10.1371/journal.pone.0256992.ISSN1932-6203.PMC8412316.PMID34473789.
- ^Williams G, Stothart CI, Hahn D, Stephens JH, Craig JC, Hodson EM (November 2023). "Cranberries for preventing urinary tract infections".The Cochrane Database of Systematic Reviews.2023(11): CD001321.doi:10.1002/14651858.CD001321.pub7.PMC10636779.PMID37947276.
- ^Kwok M, McGeorge S, Mayer Coverdale J, Graves B, Paterson DL, Harris PN, Esler R, Dowling C, Britton S, Roberts MJ (November 2022)."Guideline of guidelines: management of recurrent urinary tract infections in women".BJU International.130(Suppl 3): 11–22.doi:10.1111/bju.15756.ISSN1464-4096.PMC9790742.PMID35579121.
- ^Jepson RG, Williams G, Craig JC (17 October 2012)."Cranberries for preventing urinary tract infections".The Cochrane Database of Systematic Reviews.2012(10): CD001321.doi:10.1002/14651858.CD001321.pub5.ISSN1469-493X.PMC7027998.PMID23076891.
- ^Schwenger EM, Tejani AM, Loewen PS (December 2015)."Probiotics for preventing urinary tract infections in adults and children".The Cochrane Database of Systematic Reviews.2015(12): CD008772.doi:10.1002/14651858.CD008772.pub2.PMC8720415.PMID26695595.
- ^Gaines KK (June 2004). "Phenazopyridine hydrochloride: the use and abuse of an old standby for UTI".Urologic Nursing.24(3): 207–209.PMID15311491.
- ^Aronson JK, ed. (2008).Meyler's side effects of analgesics and anti-inflammatory drugs.Amsterdam: Elsevier Science. p. 219.ISBN978-0-444-53273-2.Archivedfrom the original on 7 May 2016.
- ^Cash JC, Glass CA (2010).Family practice guidelines(2nd ed.). New York: Springer. p. 271.ISBN978-0-8261-1812-7.Archivedfrom the original on 11 June 2016.
- ^Santillo VM, Lowe FC (January 2007). "Cranberry juice for the prevention and treatment of urinary tract infections".Drugs of Today.43(1): 47–54.doi:10.1358/dot.2007.43.1.1032055.PMID17315052.
- ^Guay DR (2009). "Cranberry and urinary tract infections".Drugs.69(7): 775–807.doi:10.2165/00003495-200969070-00002.PMID19441868.S2CID26916844.
- ^abZhanel GG, Zhanel MA, Karlowsky JA (28 March 2020)."Oral and Intravenous Fosfomycin for the Treatment of Complicated Urinary Tract Infections".The Canadian Journal of Infectious Diseases & Medical Microbiology.2020.Hindawi Limited: 8513405.doi:10.1155/2020/8513405.PMC7142339.PMID32300381.
- ^Grigoryan L, Trautner BW, Gupta K (22 October 2014). "Diagnosis and management of urinary tract infections in the outpatient setting: a review".JAMA.312(16): 1677–1684.doi:10.1001/jama.2014.12842.PMID25335150.
- ^abZalmanovici Trestioreanu A, Green H, Paul M, Yaphe J, Leibovici L (October 2010). Zalmanovici Trestioreanu A (ed.). "Antimicrobial agents for treating uncomplicated urinary tract infection in women".The Cochrane Database of Systematic Reviews.10(10): CD007182.doi:10.1002/14651858.CD007182.pub2.PMID20927755.
- ^"FDA Drug Safety Communication: FDA updates warnings for oral and injectable fluoroquinolone antibiotics due to disabling side effects".Food and Drug Administration(FDA).8 March 2018.Archivedfrom the original on 18 July 2019.Retrieved17 July2019.
- ^Jarvis TR, Chan L, Gottlieb T (February 2014)."Assessment and management of lower urinary tract infection in adults".Australian Prescriber.37(1): 7–9.doi:10.18773/austprescr.2014.002.
- ^abcGupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. (March 2011)."International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases".Clinical Infectious Diseases.52(5): e103–e120.doi:10.1093/cid/ciq257.PMID21292654.
- ^American Urogynecologic Society(5 May 2015),"Five Things Physicians and Patients Should Question",Choosing Wisely:an initiative of theABIM Foundation,American Urogynecologic Society,archivedfrom the original on 2 June 2015,retrieved1 June2015
- ^Knottnerus BJ, Grigoryan L, Geerlings SE, Moll van Charante EP, Verheij TJ, Kessels AG, ter Riet G (December 2012)."Comparative effectiveness of antibiotics for uncomplicated urinary tract infections: network meta-analysis of randomized trials".Family Practice.29(6): 659–670.doi:10.1093/fampra/cms029.PMID22516128.
- ^Afzalnia S (15 December 2006)."BestBets: Is a short course of antibiotics better than a long course in the treatment of UTI in children".www.bestbets.org.Archivedfrom the original on 14 August 2009.
- ^Bryan CS (2002).Infectious diseases in primary care.Philadelphia: W.B. Saunders. p. 319.ISBN978-0-7216-9056-8.Archivedfrom the original on 13 February 2012.
- ^Wagenlehner FM, Vahlensieck W, Bauer HW, Weidner W, Piechota HJ, Naber KG (March 2013). "Prevention of recurrent urinary tract infections".Minerva Urologica e Nefrologica.65(1): 9–20.PMID23538307.
- ^Pallett A, Hand K (November 2010)."Complicated urinary tract infections: practical solutions for the treatment of multiresistant Gram-negative bacteria".The Journal of Antimicrobial Chemotherapy.65(Suppl 3): iii25–iii33.doi:10.1093/jac/dkq298.PMID20876625.
- ^Shepherd AK, Pottinger PS (July 2013). "Management of urinary tract infections in the era of increasing antimicrobial resistance".The Medical Clinics of North America.97(4): 737–57, xii.doi:10.1016/j.mcna.2013.03.006.PMID23809723.
- ^Karlović K, Nikolić J, Arapović J (November 2018)."Ceftriaxone treatment of complicated urinary tract infections as a risk factor for enterococcal re-infection and prolonged hospitalization: A 6-year retrospective study".Bosnian Journal of Basic Medical Sciences.18(4): 361–366.doi:10.17305/bjbms.2018.3544.PMC6252101.PMID29750894.
- ^Ariathianto Y (October 2011). "Asymptomatic bacteriuria - prevalence in the elderly population".Australian Family Physician.40(10): 805–809.PMID22003486.
- ^Colgan R, Nicolle LE, McGlone A, Hooton TM (September 2006). "Asymptomatic bacteriuria in adults".American Family Physician.74(6): 985–990.PMID17002033.
- ^abAmerican Geriatrics Society,"Five Things Physicians and Patients Should Question",Choosing Wisely: an initiative of the ABIM Foundation,American Geriatrics Society,archivedfrom the original on 1 September 2013,retrieved1 August2013
- ^Widmer M, Lopez I, Gülmezoglu AM, Mignini L, Roganti A (November 2015)."Duration of treatment for asymptomatic bacteriuria during pregnancy".The Cochrane Database of Systematic Reviews.2015(11): CD000491.doi:10.1002/14651858.CD000491.pub3.PMC7043273.PMID26560337.
- ^abcGuinto VT, De Guia B, Festin MR, Dowswell T (September 2010)."Different antibiotic regimens for treating asymptomatic bacteriuria in pregnancy".The Cochrane Database of Systematic Reviews(9): CD007855.doi:10.1002/14651858.CD007855.pub2.PMC4033758.PMID20824868.
- ^abcSmaill FM, Vazquez JC (November 2019)."Antibiotics for asymptomatic bacteriuria in pregnancy".The Cochrane Database of Systematic Reviews.2019(11): CD000490.doi:10.1002/14651858.CD000490.pub4.PMC6953361.PMID31765489.
- ^Julka S (October 2013)."Genitourinary infection in diabetes".Indian Journal of Endocrinology and Metabolism.17(Suppl 1): S83–S87.doi:10.4103/2230-8210.119512.PMC3830375.PMID24251228.
- ^abSchneeberger C, Geerlings SE, Middleton P, Crowther CA (July 2015)."Interventions for preventing recurrent urinary tract infection during pregnancy".The Cochrane Database of Systematic Reviews.2015(7): CD009279.doi:10.1002/14651858.CD009279.pub3.PMC6457953.PMID26221993.
- ^The Sanford Guide to Antimicrobial Therapy 2011 (Guide to Antimicrobial Therapy (Sanford)).Antimicrobial Therapy. 2011. pp.30.ISBN978-1-930808-65-2.
- ^Long B, Koyfman A (November 2018). "The Emergency Department Diagnosis and Management of Urinary Tract Infection".Emergency Medicine Clinics of North America.36(4): 685–710.doi:10.1016/j.emc.2018.06.003.PMID30296999.S2CID52942247.
- ^abCooper TE, Teng C, Howell M, Teixeira-Pinto A, Jaure A, Wong G (August 2022)."D-mannose for preventing and treating urinary tract infections".The Cochrane Database of Systematic Reviews.2022(8): CD013608.doi:10.1002/14651858.CD013608.pub2.PMC9427198.PMID36041061.
- ^MacKenzie JR (March 1996). "A review of renal scarring in children".Nuclear Medicine Communications.17(3): 176–190.doi:10.1097/00006231-199603000-00002.PMID8692483.S2CID22331470.
- ^Smeltzer SC, Bare BG, Hinkle JL, Cheever KH (2010)."Management of Patients with Urinary Disorders".Brunner & Suddarth's textbook of medical-surgical nursing(12th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1359.ISBN978-0-7817-8589-1.Archivedfrom the original on 28 April 2016.
- ^Whiteman W, Topley C (1990).Topley and Wilson's Principles of bacteriology, virology and immunity: in 4 volumes(8th ed.). London: Arnold. p. 198.ISBN978-0-7131-4591-5.
