Epithelium
| Epithelium | |
|---|---|
 Types of epithelium | |
| Identifiers | |
| MeSH | D004848 |
| TH | H2.00.02.0.00002 |
| FMA | 9639 |
| Anatomical terms of microanatomy | |
| This article is part of a series on |
| Epithelia |
|---|
| Squamous epithelial cell |
| Columnar epithelial cell |
| Cuboidal epithelial cell |
| Specialised epithelia |
|
| Other |
Epitheliumorepithelial tissueis a thin, continuous, protective layer of compactly packedcellswith littleextracellular matrix.Epithelial tissues line the outer surfaces oforgansandblood vesselsthroughout the body, as well as the inner surfaces ofcavitiesin many internal organs. An example is theepidermis,the outermost layer of theskin.Epithelial tissue is one of the four basic types ofanimaltissue,along withconnective tissue,muscle tissueandnervous tissue.These tissues also lack blood or lymph supply. The tissue is supplied by nerves.
There are three principal shapes of epithelial cell: squamous (scaly), columnar, and cuboidal. These can be arranged in a singular layer of cells as simple epithelium, either simple squamous, simple columnar, or simple cuboidal, or in layers of two or more cells deep as stratified (layered), orcompound,either squamous, columnar or cuboidal. In some tissues, a layer of columnar cells may appear to be stratified due to the placement of the nuclei. This sort of tissue is called pseudostratified. Allglandsare made up of epithelial cells. Functions of epithelial cells includediffusion,filtration,secretion,selectiveabsorption,germination,andtranscellular transport.Compound epithelium has protective functions.
Epithelial layers contain no blood vessels (avascular), so they must receive nourishment viadiffusionof substances from the underlying connective tissue, through thebasement membrane.[1][2]: 3 Cell junctionsare especially abundant in epithelial tissues.
Classification[edit]
Simple epithelium[edit]
Simple epitheliumis a single layer of cells with every cell in direct contact with thebasement membranethat separates it from the underlying connective tissue. In general, it is found where absorption and filtration occur. The thinness of the epithelial barrier facilitates these processes.[3]
In general, epithelial tissues are classified by the number of their layers and by theshapeand function of the cells.[1][3][4]The basic cell types are squamous, cuboidal, and columnar, classed by their shape.
| Type | Description |
|---|---|
| Squamous | Squamous cells have the appearance of thin, flat plates that can look polygonal when viewed from above.[5]Their name comes fromsquāma,Latin for "scale" – as on fish or snake skin. The cells fit closely together in tissues, providing a smooth, low-friction surface over which fluids can move easily. The shape of the nucleus usually corresponds to the cell form and helps to identify the type of epithelium. Squamous cells tend to have horizontally flattened, nearly oval-shaped nuclei because of the thin, flattened form of the cell. Squamous epithelium is found lining surfaces such asskinoralveoliin thelung,enabling simple passive diffusion as also found in thealveolar epitheliumin the lungs. Specialized squamous epithelium also forms the lining of cavities such as in blood vessels (asendothelium), in thepericardium(asmesothelium), and in otherbody cavities. |
| Cuboidal | Cuboidal epithelial cells have a cube-like shape and appear square in cross-section. The cell nucleus is large, spherical and is in the center of the cell. Cuboidal epithelium is commonly found in secretive tissue such as theexocrine glands,or in absorptive tissue such as the pancreas, the lining of the kidney tubules as well as in the ducts of the glands. Thegerminal epitheliumthat covers the femaleovary,and thegerminal epitheliumthat lines the walls of the seminferous tubules in the testes are also of the cuboidal type. Cuboidal cells provide protection and may be active in pumping material in or out of the lumen, or passive depending on their location and specialisation. Simple cuboidal epithelium commonly differentiates to form the secretory and duct portions of glands.[6]Stratified cuboidal epithelium protects areas such as the ducts ofsweat glands,[7]mammary glands,andsalivary glands. |
| Columnar | Columnar epithelial cells are elongated and column-shaped and have a height of at least four times their width. Their nuclei are elongated and are usually located near the base of the cells. Columnar epithelium forms the lining of the stomach and intestines. The cells here may possessmicrovillifor maximizing the surface area for absorption, and these microvilli may form abrush border.Other cells may beciliatedto move mucus in the function ofmucociliary clearance.Other ciliated cells are found in thefallopian tubes,the uterus andcentral canalof thespinal cord.Some columnar cells are specialized for sensory reception such as in the nose, ears and thetaste buds.Hair cellsin theinner earshavestereociliawhich are similar to microvilli.Goblet cellsare modified columnar cells and are found between the columnar epithelial cells of the duodenum. They secrete mucus, which acts as a lubricant. Single-layered non-ciliated columnar epithelium tends to indicate an absorptive function. Stratified columnar epithelium is rare but is found inlobar ductsin thesalivary glands,theeye,thepharynx,andsex organs.This consists of a layer of cells resting on at least one other layer of epithelial cells, which can be squamous, cuboidal, or columnar. |
| Pseudostratified | These are simple columnar epithelial cells whose nuclei appear at different heights, giving the misleading (hence "pseudo" ) impression that the epithelium is stratified when the cells are viewed in cross section.Ciliatedpseudostratified epithelial cells have cilia. Cilia are capable of energy-dependent pulsatile beating in a certain direction through interaction of cytoskeletal microtubules and connecting structural proteins and enzymes. In therespiratory tract,the wafting effect produced causes mucus secreted locally by the goblet cells (to lubricate and to trap pathogens and particles) to flow in that direction (typically out of the body). Ciliated epithelium is found in the airways (nose, bronchi), but is also found in the uterus andfallopian tubes,where the cilia propel the ovum to the uterus. |
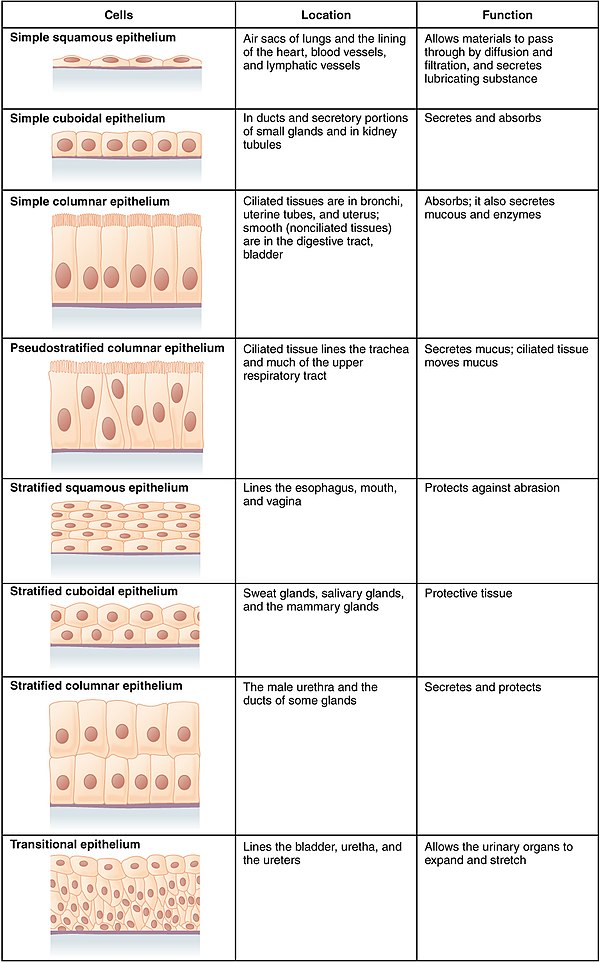
By layer, epithelium is classed as either simple epithelium, only one cell thick (unilayered), or stratified epithelium having two or more cells in thickness, or multi-layered – asstratified squamous epithelium,stratified cuboidal epithelium,andstratified columnar epithelium,[8]: 94, 97 and both types of layering can be made up of any of the cell shapes.[3]However, when taller simple columnar epithelial cells are viewed in cross section showing several nuclei appearing at different heights, they can be confused with stratified epithelia. This kind of epithelium is therefore described aspseudostratified columnar epithelium.[9]
Transitional epitheliumhas cells that can change from squamous to cuboidal, depending on the amount of tension on the epithelium.[10]
Stratified epithelium[edit]
Stratified or compound epithelium differs from simple epithelium in that it is multilayered. It is therefore found where body linings have to withstand mechanical or chemical insult such that layers can be abraded and lost without exposing subepithelial layers. Cells flatten as the layers become more apical, though in their most basal layers, the cells can be squamous, cuboidal, or columnar.[11]
Stratified epithelia (of columnar, cuboidal, or squamous type) can have the following specializations:[11]
| Specialization | Description |
|---|---|
| Keratinized | In this particular case, the most apical layers (exterior) of cells are dead and lose their nucleus and cytoplasm, instead contain a tough, resistant protein called keratin. This specialization makes the epithelium somewhat water-resistant, so is found in the mammalian skin. The lining of the oesophagus is an example of a non-keratinized or "moist" stratified epithelium.[11] |
| Parakeratinized | In this case, the most apical layers of cells are filled with keratin, but they still retain their nuclei. These nuclei arepyknotic,meaning that they are highly condensed. Parakeratinized epithelium is sometimes found in theoral mucosaand in the upper regions of the oesophagus.[12] |
| Transitional | Transitional epithelia are found in tissues that stretch, and it can appear to be stratified cuboidal when the tissue is relaxed, or stratified squamous when the organ is distended and the tissue stretches. It is sometimes calledurotheliumsince it is almost exclusively found in thebladder,uretersandurethra.[11] |
Structure[edit]
Epithelial tissue cells can adopt shapes of varying complexity frompolyhedraltoscutoidalto punakoidal.[13]They are tightly packed and form a continuous sheet with almost no intercellular spaces. All epithelia is usually separated from underlying tissues by an extracellular fibrous basement membrane. The lining of the mouth, lung alveoli and kidney tubules are all made of epithelial tissue. The lining of the blood and lymphatic vessels are of a specialised form of epithelium calledendothelium.
Location[edit]

Epithelium lines both the outside (skin) and the inside cavities andluminaof bodies. The outermost layer ofhuman skinis composed of deadstratified squamous,keratinizedepithelial cells.[14]
Tissues that line the inside of the mouth, theesophagus,thevagina,and part of therectumare composed ofnonkeratinizedstratified squamous epithelium. Other surfaces that separate body cavities from the outside environment are lined by simple squamous, columnar, or pseudostratified epithelial cells. Other epithelial cells line the insides of thelungs,thegastrointestinal tract,the reproductive and urinary tracts, and make up theexocrineandendocrine glands.The outer surface of thecorneais covered with fast-growing, easily regenerated epithelial cells. A specialised form of epithelium,endothelium,forms the inner lining ofblood vesselsand theheart,and is known as vascular endothelium, and lininglymphatic vesselsas lymphatic endothelium. Another type,mesothelium,forms the walls of thepericardium,pleurae,andperitoneum.[citation needed]
In arthropods, theintegument,or external "skin", consists of a single layer of epithelial ectoderm from which arises thecuticle,[15]an outer covering ofchitin,the rigidity of which varies as per its chemical composition.
Basement membrane[edit]
The basal surface of epithelial tissue rests on abasement membraneand the free/apical surface faces body fluid or outside. The basement membrane acts as a scaffolding on which epithelium can grow and regenerate after injuries.[16]Epithelial tissue has anerve supply,but noblood supplyand must be nourished by substances diffusing from the blood vessels in the underlying tissue. The basement membrane acts as a selectively permeable membrane that determines which substances will be able to enter the epithelium.[2]: 3
Thebasal laminais made up of laminin (glycoproteins) secreted by epithelial cells. Thereticular laminabeneath the basal lamina is made up of collagen proteins secreted byconnective tissue.
Cell junctions[edit]
Cell junctionsare especially abundant in epithelial tissues. They consist of protein complexes and provide contact between neighbouring cells, between a cell and theextracellular matrix,or they build up the paracellular barrier of epithelia and control theparacellular transport.[17]
Cell junctions are the contact points between plasma membrane and tissue cells. There are mainly 5 different types of cell junctions:tight junctions,adherens junctions,desmosomes,hemidesmosomes,andgap junctions. Tight junctions are a pair of trans-membrane protein fused on outer plasma membrane. Adherens junctions are a plaque (protein layer on the inside plasma membrane) which attaches both cells' microfilaments. Desmosomes attach to the microfilaments of cytoskeleton made up of keratin protein. Hemidesmosomes resemble desmosomes on a section. They are made up of the integrin (a transmembrane protein) instead of cadherin. They attach the epithelial cell to the basement membrane. Gap junctions connect the cytoplasm of two cells and are made up of proteins calledconnexins(six of which come together to make a connexion).[citation needed]
Development[edit]
Epithelial tissues are derived from all of the embryologicalgerm layers:[citation needed]
- fromectoderm(e.g., theepidermis);
- fromendoderm(e.g., the lining of thegastrointestinal tract);
- frommesoderm(e.g., the inner linings ofbody cavities).
However,pathologistsdo not considerendotheliumandmesothelium(both derived from mesoderm) to be true epithelium. This is because such tissues present very different pathology. For that reason, pathologists label cancers in endothelium and mesotheliumsarcomas,whereas true epithelial cancers are calledcarcinomas.Additionally, the filaments that support these mesoderm-derived tissues are very distinct. Outside of the field of pathology, it is generally accepted that the epithelium arises from all three germ layers.[citation needed]
Cell turnover[edit]
Epithelia turn over at some of the fastest rates in the body. For epithelial layers to maintain constant cell numbers essential to their functions, the number of cells that divide must match those that die. They do this mechanically. If there are too few the cells the stretch that they experience rapidly activates cell division.[18]Alternatively, when too many cells accumulate, crowding triggers their death by activation epithelialcell extrusion.[19][20]Here, cells fated for elimination are seamlessly squeezed out by contracting a band of actin and myosin around and below the cell, preventing any gaps from forming that could disrupt their barriers. Failure to do so can result in aggressive tumors and their invasion by aberrant basal cell extrusion.[21][22]
Functions[edit]

Epithelial tissues have as their primary functions:
- to protect the tissues that lie beneath fromradiation,desiccation,toxins,invasion by pathogens, and physicaltrauma
- the regulation and exchange of chemicals between the underlying tissues and abody cavity
- the secretion of hormones into thecirculatory system,as well as the secretion of sweat, mucus, enzymes, and other products that are delivered by ducts[8]: 91
- to provide sensation[23]
- Absorb water and digested food in the lining of digestive canal.
Glandular tissue[edit]
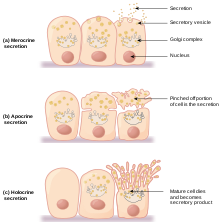
Glandular tissue is the type of epithelium that forms theglandsfrom the infolding of epithelium and subsequent growth in the underlying connective tissue. They may be specialized columnar or cuboidal tissues consisting ofgoblet cells,which secretemucus.There are two major classifications of glands:endocrine glandsandexocrine glands:
- Endocrine glands secrete their product into the extracellular space where it is rapidly taken up by the circulatory system.
- Exocrine glands secrete their products into a duct that then delivers the product to thelumenof an organ or onto the free surface of the epithelium. Their secretions includetears,saliva,oil(sebum),enzyme,digestive juices,sweat,etc.
Sensing the extracellular environment[edit]
Some epithelial cells areciliated,especially inrespiratory epithelium,and they commonly exist as a sheet ofpolarised cellsforming a tube or tubule with cilia projecting into thelumen."Primary ciliaon epithelial cells provide chemosensation,thermoception,andmechanosensationof the extracellular environment by playing "a sensory role mediating specific signalling cues, including soluble factors in the external cell environment, a secretory role in which a soluble protein is released to have an effect downstream of the fluid flow, and mediation of fluid flow if the cilia aremotile.[24]
Host immune response[edit]
Epithelial cells express many genes that encodeimmune mediatorsand proteins involved incell-cell communicationwith hematopoietic immune cells.[25]The resulting immune functions of these non-hematopoietic, structural cells contribute to the mammalian immune system ( "structural immunity" ).[26][27]Relevant aspects of the epithelial cell response to infections are encoded in theepigenomeof these cells, which enables a rapid response to immunological challenges.
Clinical significance[edit]

The slide shows at (1) an epithelial cell infected byChlamydia pneumoniae;theirinclusion bodiesshown at (3); an uninfected cell shown at (2) and (4) showing the difference between an infectedcell nucleusand an uninfected cell nucleus.
Epithelium grown in culture can be identified by examining its morphological characteristics. Epithelial cells tend to cluster together, and have a "characteristic tight pavement-like appearance". But this is not always the case, such as when the cells are derived from a tumor. In these cases, it is often necessary to use certain biochemical markers to make a positive identification. The intermediate filament proteins in thecytokeratingroup are almost exclusively found in epithelial cells, so they are often used for this purpose.[2]: 9
Cancers originating from the epithelium are classified ascarcinomas.In contrast,sarcomasdevelop inconnective tissue.[28]
When epithelial cells or tissues are damaged fromcystic fibrosis,sweat glands are also damaged, causing a frosty coating of the skin.[citation needed]
Etymology and pronunciation[edit]
The wordepitheliumuses the Greek roots ἐπί (epi), "on" or "upon", and θηλή (thēlē), "nipple". Epithelium is so called because the name was originally used to describe the translucent covering of small "nipples" of tissue on thelip.[29]The word has bothmassandcountsenses; the plural form isepithelia.
Additional images[edit]
-
Squamous epithelium 100×
-
Human cheek cells (nonkeratinized stratified squamous epithelium) 500×
-
Histology of female urethra showing transitional epithelium
-
Histology of sweat gland showing stratified cuboidal epithelium
See also[edit]
- Dark cell
- Epithelial-mesenchymal transition
- Epithelial polarity
- Glycocalyx
- Innerandouter enamel epithelium
- Iris pigment epithelium
- Neuroepithelial cell
- Retinal pigment epithelium
- Skin cancer
- Sulcular epithelium
- List of distinct cell types in the adult human body
References[edit]
- ^abEurell JA, Frappier BL, eds. (2006).Dellmann's Textbook of Veterinary Histology.Wiley-Blackwell. p. 18.ISBN978-0-7817-4148-4.
- ^abcFreshney RI (2002). "Introduction". In Freshney RI, Freshney M (eds.).Culture of epithelial cells.John Wiley & Sons.ISBN978-0-471-40121-6.
- ^abcMarieb EM (1995).Human Anatomy and Physiology(3rd ed.). Benjamin/Cummings. pp.103–104.ISBN0-8053-4281-8.
- ^Platzer W (2008).Color atlas of human anatomy: Locomotor system.Thieme. p. 8.ISBN978-3-13-533306-9.
- ^Kühnel W (2003).Color atlas of cytology, histology, and microscopic anatomy.Thieme. p. 102.ISBN978-3-13-562404-4.
- ^Pratt R."Simple Cuboidal Epithelium".AnatomyOne.Amirsys, Inc.Retrieved28 September2012.
- ^Eroschenko VP (2008). "Integumentary System".DiFiore's Atlas of Histology with Functional Correlations.Lippincott Williams & Wilkins. pp.212–234.ISBN9780781770576.
- ^abvan Lommel AT (2002).From cells to organs: a histology textbook and atlas.Springer.ISBN978-1-4020-7257-4.
- ^Melfi RC, Alley KE, eds. (2000).Permar's oral embryology and microscopic anatomy: a textbook for students in dental hygiene.Lippincott Williams & Wilkins. p.9.ISBN978-0-683-30644-6.
- ^Pratt R."Epithelial Cells".AnatomyOne.Amirsys, Inc. Archived fromthe originalon 19 December 2012.Retrieved28 September2012.
- ^abcdJenkins GW, Tortora GJ (2013).Anatomy and Physiology from Science to Life(3rd ed.). John Wiley & Sons. pp. 110–115.ISBN978-1-118-12920-3.
- ^Ross MH, Pawlina W (2015).Histology: A Text and Atlas: With Correlated Cell and Molecular Biology(7th ed.). Lippincott Williams & Wilkins. pp. 528, 604.ISBN978-1451187427.
- ^Iber, Dagmar; Vetter, Roman (12 May 2022)."3D Organisation of Cells in Pseudostratified Epithelia".Frontiers in Physics.10.Bibcode:2022FrP....10.8160I.doi:10.3389/fphy.2022.898160.hdl:20.500.11850/547113.
- ^Marieb E (2011).Anatomy & Physiology.Boston: Benjamin Cummings. p. 133.ISBN978-0321616401.
- ^Kristensen NP, Georges C (1 December 2003)."Integument".Lepidoptera, Moths and Butterflies: Morphology, Physiology, and Development: Teilband.Walter de Gruyter. p. 484.ISBN978-3-11-016210-3.Retrieved10 January2013.
- ^McConnell TH (2006).The nature of disease: pathology for the health professions.Lippincott Williams & Wilkins. p. 55.ISBN978-0-7817-5317-3.
- ^Alberts B (2002).Molecular biology of the cell(4th ed.). New York [u.a.]: Garland. p. 1067.ISBN0-8153-4072-9.
- ^Gudipaty SA, Lindblom J, Loftus PD, Redd MJ, Edes K, Davey CF, et al. (March 2017)."Mechanical stretch triggers rapid epithelial cell division through Piezo1".Nature.543(7643): 118–121.Bibcode:2017Natur.543..118G.doi:10.1038/nature21407.PMC5334365.PMID28199303.
- ^Rosenblatt J, Raff MC, Cramer LP (November 2001)."An epithelial cell destined for apoptosis signals its neighbors to extrude it by an actin- and myosin-dependent mechanism".Current Biology.11(23): 1847–1857.Bibcode:2001CBio...11.1847R.doi:10.1016/S0960-9822(01)00587-5.PMID11728307.S2CID5858676.
- ^Eisenhoffer GT, Loftus PD, Yoshigi M, Otsuna H, Chien CB, Morcos PA, Rosenblatt J (April 2012)."Crowding induces live cell extrusion to maintain homeostatic cell numbers in epithelia".Nature.484(7395): 546–549.Bibcode:2012Natur.484..546E.doi:10.1038/nature10999.PMC4593481.PMID22504183.
- ^Fadul J, Zulueta-Coarasa T, Slattum GM, Redd NM, Jin MF, Redd MJ, et al. (December 2021)."KRas-transformed epithelia cells invade and partially dedifferentiate by basal cell extrusion".Nature Communications.12(1): 7180.Bibcode:2021NatCo..12.7180F.doi:10.1038/s41467-021-27513-z.PMC8664939.PMID34893591.
- ^Gu Y, Shea J, Slattum G, Firpo MA, Alexander M, Mulvihill SJ, et al. (January 2015)."Defective apical extrusion signaling contributes to aggressive tumor hallmarks".eLife.4:e04069.doi:10.7554/eLife.04069.PMC4337653.PMID25621765.
- ^Alberts B (2002).Molecular Biology of the Cell(4th ed.). New York [u.a.]: Garland. p. 1267.ISBN0-8153-4072-9.
- ^Adams M, Smith UM, Logan CV, Johnson CA (May 2008)."Recent advances in the molecular pathology, cell biology and genetics of ciliopathies".Journal of Medical Genetics.45(5): 257–267.doi:10.1136/jmg.2007.054999.PMID18178628.
- ^Armingol E, Officer A, Harismendy O, Lewis NE (February 2021)."Deciphering cell-cell interactions and communication from gene expression".Nature Reviews. Genetics.22(2): 71–88.doi:10.1038/s41576-020-00292-x.PMC7649713.PMID33168968.
- ^Krausgruber T, Fortelny N, Fife-Gernedl V, Senekowitsch M, Schuster LC, Lercher A, et al. (July 2020)."Structural cells are key regulators of organ-specific immune responses".Nature.583(7815): 296–302.Bibcode:2020Natur.583..296K.doi:10.1038/s41586-020-2424-4.PMC7610345.PMID32612232.S2CID220295181.
- ^Minton K (September 2020)."A gene atlas of 'structural immunity'".Nature Reviews. Immunology.20(9): 518–519.doi:10.1038/s41577-020-0398-y.PMID32661408.S2CID220491226.
- ^"Types of cancer".Cancer Research UK.28 October 2014.Retrieved13 October2016.
- ^Van Blerkom J, Gregory L (2004).Essential IVF: basic research and clinical applications.Boston: Kluwer Academic Publishers. p. 3.ISBN978-1-4020-7551-3.
Further reading[edit]
- Green H (September 2008). "The birth of therapy with cultured cells".BioEssays.30(9): 897–903.doi:10.1002/bies.20797.PMID18693268.
- Kefalides NA, Borel JP, eds. (2005).Basement membranes: cell and molecular biology.Gulf Professional Publishing.ISBN978-0-12-153356-4.
- Nagpal R, Patel A, Gibson MC (March 2008). "Epithelial topology".BioEssays.30(3): 260–266.doi:10.1002/bies.20722.PMID18293365.
- Yamaguchi Y, Brenner M, Hearing VJ (September 2007)."The regulation of skin pigmentation".The Journal of Biological Chemistry.282(38): 27557–27561.doi:10.1074/jbc.R700026200.PMID17635904.
External links[edit]
- Epithelium Photomicrographs
- Histology at KUMCepithel-epith02Simple squamous epithelium of theglomerulus(kidney)
- Diagrams of simple squamous epithelium
- Histology at KUMCepithel-epith12Stratified squamous epithelium of the vagina
- Histology at KUMCepithel-epith14Stratified squamous epithelium of the skin (thin skin)
- Histology at KUMCepithel-epith15Stratified squamous epithelium of the skin (thick skin)
- Stratified squamous epithelium of the esophagus
- Microanatomy Web Atlas




