Haldane effect
TheHaldane effectis a property ofhemoglobinfirst described byJohn Scott Haldane,within which oxygenation of blood in the lungs displaces carbon dioxide from hemoglobin, increasing the removal of carbon dioxide. Consequently, oxygenated blood has a reduced affinity for carbon dioxide. Thus, the Haldane effect describes the ability of hemoglobin to carry increased amounts of carbon dioxide (CO2) in the deoxygenated state as opposed to the oxygenated state. Vice versa, it is true that a high concentration of CO2facilitates dissociation of oxyhemoglobin, though this is the result of two distinct processes (Bohr effect and Margaria-Green effect) and should be distinguished from Haldane effect.
Carbaminohemoglobin[edit]
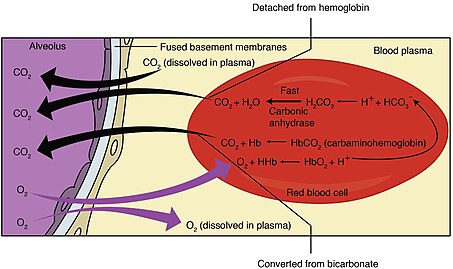
Carbon dioxide travels through thebloodin three different ways. One of these ways is by binding toaminogroups, creatingcarbaminocompounds. Amino groups are available for binding at the N-terminals and at side-chains ofarginineandlysineresidues in hemoglobin. When carbon dioxide binds to these residuescarbaminohemoglobinis formed.[1]This amount ofcarbaminohemoglobinformed is inversely proportional to the amount of oxygen attached to hemoglobin. Thus, at lower oxygen saturation, morecarbaminohemoglobinis formed. These dynamics explain the relative difference in hemoglobin's affinity for carbon dioxide depending on oxygen levels known as the Haldane effect.[2]
Buffering[edit]
Histidineresidues in hemoglobin can accept protons and act asbuffers.Deoxygenated hemoglobin is a betterproton acceptorthan the oxygenated form.[1]
In red blood cells, the enzymecarbonic anhydrasecatalyzes the conversion of dissolved carbon dioxide tocarbonic acid,which rapidly dissociates tobicarbonateand a freeproton:
ByLe Chatelier's principle,anything that stabilizes the proton produced will cause the reaction to shift to the right, thus the enhanced affinity of deoxyhemoglobin for protons enhances synthesis of bicarbonate and accordingly increases capacity of deoxygenated blood for carbon dioxide. The majority of carbon dioxide in the blood is in the form of bicarbonate. Only a very small amount is actually dissolved as carbon dioxide, and the remaining amount of carbon dioxide is bound to hemoglobin.
In addition to enhancing removal of carbon dioxide from oxygen-consuming tissues, the Haldane effect promotes dissociation ofcarbon dioxidefrom hemoglobin in the presence ofoxygen.In the oxygen-rich capillaries of the lung, this property causes the displacement of carbon dioxide to plasma as low-oxygen blood enters thealveolusand is vital foralveolar gas exchange.
The general equation for the Haldane Effect is:
- H++ HbO2⇌ H+Hb + O2;
However, this equation is confusing as it reflects primarily theBohr effect.The significance of this equation lies in realizing that oxygenation of Hb promotes dissociation of H+from Hb, which shifts the bicarbonate buffer equilibrium towards CO2formation; therefore, CO2is released from RBCs.[3]
Clinical significance[edit]
In patients with lung disease, lungs may not be able to increasealveolar ventilationin the face of increased amounts of dissolved CO2.
This partially explains the observation that some patients withemphysemamight have an increase in PaCO2(partial pressure of arterial dissolved carbon dioxide) following administration of supplemental oxygen even if content of CO2stays equal.[4]
See also[edit]
References[edit]
- ^abLumb, AB (2000).Nunn's Applied Respiratory Physiology(5th ed.). Butterworth Heinemann. pp. 227–229.ISBN0-7506-3107-4.
- ^Teboul, Jean-Louis; Scheeren, Thomas (2017-01-01)."Understanding the Haldane effect".Intensive Care Medicine.43(1): 91–93.doi:10.1007/s00134-016-4261-3.ISSN1432-1238.PMID26868920.S2CID31191748.
- ^Siggaard, O; Garby L (1973). "The Bohr Effect and the Haldane Effect".Scandinavian Journal of Clinical and Laboratory Investigation.31(1): 1–8.doi:10.3109/00365517309082411.PMID4687773.
- ^Hanson, CW; Marshall BE; Frasch HF; Marshall C (January 1996). "Causes of hypercarbia with oxygen therapy in patients with chronic obstructive pulmonary disease".Critical Care Medicine.24(1): 23–28.doi:10.1097/00003246-199601000-00007.PMID8565533.
External links[edit]
- Nosek, Thomas M."Section 4/4ch5/s4ch5_31".Essentials of Human Physiology.Archived fromthe originalon 2015-12-09.