Hysterosalpingography
This article has multiple issues.Please helpimprove itor discuss these issues on thetalk page.(Learn how and when to remove these messages)
|
| Hysterosalpingography | |
|---|---|
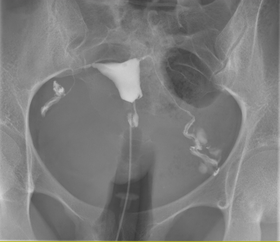 A normal hysterosalpingogram.Note the catheter entering at the bottom of the screen, and thecontrast mediumfilling the uterine cavity (small triangle in the center). | |
| Other names | Uterosalpingography |
| ICD-9-CM | 87.8 |
| MeSH | D007047 |
| MedlinePlus | 003404 |
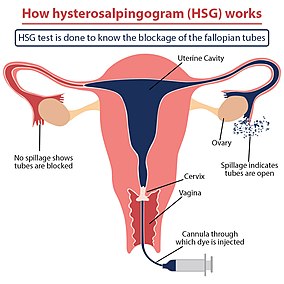
Hysterosalpingography(HSG), also known asuterosalpingography,[1]is aradiologicprocedure to investigate the shape of the uterine cavity and the shape and patency of thefallopian tubes.It is a special x-ray procedure usingdyeto look at the womb (uterus) and fallopian tubes.[2]In this procedure, aradio-opaquematerial is injected into thecervicalcanal, and radiographs are taken. A normal result shows the filling of theuterine cavityand the bilateral filling of the fallopian tube with the injection material. To demonstrate tubal patency, spillage of the material into theperitoneal cavityneeds to be observed. Hysterosalpingography has vital role in treatment of infertility, especially in the case of fallopian tube blockage.
Uses
[edit]HSG is considered adiagnostic procedure.It is used in the workup ofinfertilefemales to assess the patency offallopian tubes,assess the competency of the cervix or congenital abnormality of the uterus in multiplemiscarriages,assess the patency of fallopian tubes after surgery ortubal ligation,or before reversal of tubal ligation. Rarely, HSG is used to assess the integrity of aCaesarean scar.[3]
Occasionally, HSG may also havetherapeuticbenefits forinfertility treatment.When oil-based contrast is used, rates of pregnancy increase by about 10% compared to water-based contrast.[4]A meta-analysis revealed 3.6 times greaterodds(OR = 3.6) of pregnancy with oil-based contrast compared to no hysterosalpingography.[5]This effect is thought to be due to the flushing action of the contrast into the uterus that causes dislodgement of mucus plug, debris, or opening of mild adhesions in the fallopian tubes.[6]
HSG is contraindicated during menstruation, suspected cancer, pregnancy, unprotected sexual intercourse during themenstrual cycle,any purulent discharge from the vagina, or if the individual was diagnosed withpelvic inflammatory diseasesix months previously. For those with hypersensitivity to contrast, HSG is relatively contraindicated.
Procedure
[edit]Either high osmolar contrast material (HOCM) or low osmolar contrast material (LOCM) can be used. 10 to 20 ml of LOCM can be used at a concentration of 270 to 300 mg/ml. The contrast media should be prewarmed to room temperature before administered into the cervix, so as to prevent spasm offallopian tubes.5Fr to 7Fr hysterosalpingogram balloon catheter can be used. Margolin HSG cannula is used if the cervix is narrow orstenosed.[3]HSG appointment is usually made during the 4th to 10th days of regular menstrual cycle (follicular phase).[7]The subject should not undergone any sexual intercourse before HSG. Anxious subjects may need painkillers or other medications.Informed consentshould be taken before the procedure.[3]
The subject lies down on table in supine position with legs flexed andabducted.Vulvais cleaned withchlorhexidineornormal saline.A speculum is inserted to thevaginawith the help of sterile jelly, and thecervixis exposed. The cervical opening is identified using a bright light. The HSG catheter is then inserted into thecervical canal.Occasionally, Vulsellum forceps may be used to hold the cervical lips open. Ifcervical weaknessis suspected, the catheter should be left inside the lower cervical canal.[3]Air bubbles should be expelled from the syringe and the catheter, otherwise it will cause confusion of interpretations on HSG. Contrast medium is injected slowly into the uterine cavity with intermittentfluoroscopicscreening. If there are no spills from bilateral fallopian tubes bilaterally, intravenousbuscopanandglucagoncan be given to relieve spasm of fallopian tubes.[3]Opiatesshould not be given, as it may increase pain because of increased smooth muscle contractions.[3]
The procedure involves x-rays (fluoroscopy).[7]Images are taken to demonstrate the filling ofendometrial cavity,which shows full view of the fallopian tubes demonstrating the spillage of contrast material intoperitoneum,the extent of the block if no spillage is present, or a delayed view in the case of abnormal cavities (locule) within. Subject may have vaginal spotting for one to two days, accompanied with pain that may persist for up to two weeks. Some medical centres routinely giveprophylacticantibiotics before subject is allowed home.[3]
Complications
[edit]Possible complications of the procedure includeinfection,[2]allergicreactions to the materials used,[2]intravasationof the contrast material, pain during the procedure, nausea, vomiting, and headache. Some subjects may developvasovagal syncopeduring the inflation of balloon in the cervical canal.[3]
History
[edit]For the first HSG, Carey usedcollargolin 1914.Lipiodolwas introduced by Sicard and Forestier in 1924, and remained a popular contrast medium for many decades.[8]Later, water-soluble contrast material was generally preferred as it avoided the possible complication of oil embolism.
Follow up
[edit]If the HSG indicates further investigations are warranted, alaparoscopy,assisted byhysteroscopy,may be advised to visualize the area in three dimensions, with the potential to resolve minor issues within the same procedure.[citation needed]
See also
[edit]References
[edit]- ^"Hysterosalpingography (Uterosalpingography)".RadiologyInfo. June 8, 2016.
- ^abc"Hysterosalpingography: MedlinePlus Medical Encyclopedia".medlineplus.gov.Retrieved2019-05-06.
- ^abcdefghWatson N, Jones H (2018).Chapman and Nakielny's Guide to Radiological Procedures.Elsevier. pp. 163–166.ISBN9780702071669.
- ^Dreyer, Kim; Rijswijk, Joukje van; Mijatovic, Velja; Goddijn, Mariëtte; Verhoeve, Harold R.; Rooij, Ilse A.J. van; Hoek, Annemieke; Bourdrez, Petra; Nap, Annemiek W. (2017-05-18)."Oil-Based or Water-Based Contrast for Hysterosalpingography in Infertile Women".New England Journal of Medicine.376(21): 2043–2052.doi:10.1056/nejmoa1612337.PMID28520519.
- ^Wang, Rui; Watson, Andrew; Johnson, Neil; Cheung, Karen; Fitzgerald, Cheryl; Mol, Ben Willem J.; Mohiyiddeen, Lamiya (October 15, 2020)."Tubal flushing for subfertility".The Cochrane Database of Systematic Reviews.2020(10): CD003718.doi:10.1002/14651858.CD003718.pub5.ISSN1469-493X.PMC9508794.PMID33053612.S2CID222421134.
- ^Grigovich, Maria; Kacharia, Vidhi S.; Bharwani, Nishat; Hemingway, Anne; Mijatovic, Velja; Rodgers, Shuchi K. (October 2021)."Evaluating Fallopian Tube Patency: What the Radiologist Needs to Know".RadioGraphics.41(6): 1876–18961.doi:10.1148/rg.2021210033.ISSN0271-5333.PMID34597232.S2CID238249552.
- ^abBaramki T (2005)."Hysterosalpingography".Fertil Steril.83(6): 1595–606.doi:10.1016/j.fertnstert.2004.12.050.PMID15950625.
- ^Bendick A. J. (1947). "Present Status of Hysterosalpingography".Journal of the Mount Sinai Hospital, New York.14(3): 739–742.PMID20265114.
External links
[edit]- HSG TestArchived2018-12-21 at theWayback Machine- HSG Test: Cost, Results, Expert Advice, Preparation
- HSGArchived2020-10-27 at theWayback Machine- HSG Test -HSG Film Advice, Preparation
