Nonspecific immune cell
Anon-specific immune cellis animmune cell(such as amacrophage,neutrophil,ordendritic cell) that responds to manyantigens,not just one antigen. Non-specific immune cells function in the first line of defense against infection or injury. The innate immune system is always present at the site of infection and ready to fight the bacteria; it can also be referred to as the "natural" immune system. The cells of the innate immune system do not have specific responses and respond to each foreign invader using the same mechanism.[1]
The innate immune system
[edit]There are two categories to which parts of theimmune systemare assigned: the non-specific, orinnate immune systemand theadaptive immune system.The non-specific response is a generalized response to pathogen infections involving the use of several white blood cells and plasma proteins. Non-specific immunity, or innate immunity, is the immune system with which you were born, made up of phagocytes and barriers.Phagocytosis,derived from the Greek wordsphagein,meaning to eat,kytosor cell, and “osis” meaning process, was first described byÉlie Metchnikoff,who won the Nobel Prize 100 years ago. Phagocytosis involves the internalization of solids, such as bacteria, by an organism.
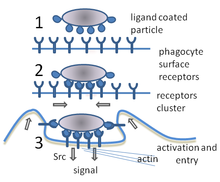
Macrophages, neutrophils, and dendritic cells are all cells of the innate immune system that utilizephagocytosisand are equipped withToll-like receptors (TLR).Toll-like receptors are present on each of these cells and recognize a variety of microbial products resulting in the induction of more specific immune responses.[2]When a phagocytic cell engulfs bacteria, a phagosome is formed around it and the entire complex is ultimately trafficked to the lysosome for degradation. These cells that participate in the non-specific immune system response do not differentiate between types of microorganisms but do have the ability to discern between what is self and what is non-self. The cells of this system are known as non-specific immune cells.[3]
Cells of the innate immune system
[edit]Neutrophilsare a type of phagocyte, abundant in blood, that phagocytize pathogens in acute inflammation. Neutrophils, along witheosinophilsandbasophils,make up the category ofgranulocytes.Macrophages,also known as monocytes, will phagocytize a wide range of molecules.Dendritic cellsare tree-like cells that bindantigensand alert thelymphocytesof infection, essentially directingT cellsto make an immune response. Complement proteins are proteins that play a role in the non-specific immune responses alongside these non-specific immune cells to make up the first line of immune defense.[4]
The non-specific immune response is an immediate antigen-independent response, however it is not antigen-specific. Non-specific immunity results in no immunologic memory. There are mechanical, chemical, and biological factors affecting the effectiveness and results of the non-specific immune response. These factors include the epithelial surfaces forming a physical barrier, fatty acids that inhibit the growth of bacteria, and themicrofloraof the gastrointestinal tract serving to prevent the colonization of pathogenic bacteria. The non-specific immune system involves cells to which antigens are not specific in regards to fighting infection. The non-specific immune cells mentioned above (macrophages, neutrophils, and dendritic cells) will be discussed regarding their immediate response to infection.[5]
Macrophages
[edit]
Macrophagesdisplay a plasticity that allows them to respond to numerous types of infections, permitting them to change their physiology, while serving as a common “janitorial cell” to the immune system.[6]Macrophages are produced through the differentiation ofmonocytes,and after ingestion of bacteria, secrete enzymes to destroy the ingested particle. These cells reside in every tissue of the body, and upon infected tissue, are recruited to the tissue. Once recruited, macrophages will differentiate into specific tissue macrophages. The receptors of macrophages consist of a broad specificity that allows them to discern between self and non-self in the non-specific recognition of foreign substances. There are type I and type II receptors present on macrophages, which are trimeric membraneglycoproteinseach containing anNH2-terminalintracellulardomain, an extracellular domain with a spacer region and an alpha-helical domain.[7]Contrary to the structure of type II, type I receptors have a cysteine-rich COOH-terminal domain. These characteristics of macrophage receptors confer the broad specificity, which allow them to function as a general non-specific immune cell.
Neutrophils
[edit]
Neutrophilsare some of the first immune cells to travel to sites of infection that aid in fighting infection by ingestingmicroorganismsand providing the enzymes to kill them. This process characterizes neutrophils as a type ofphagocyte.[8]Neutrophils containneutrophil extracellular traps(NETs), composed of granule and nuclear constituents, which play a role in breaking up and killing bacteria that has invaded the immune system. NETs, composed of activated neutrophils, are fragile structures consisting of smooth stretches and globular domains, as shown viahigh-resolution scanning electron microscopy.[9]
After stimulation of the neutrophil response, neutrophils lose their shape, allowingeuchromatinandheterochromatinto homogenize, later resulting in the mixing of NET components. The formation of NETs happens once thenuclear envelopeand granule membrane of the neutrophils disintegrates. The NETs are released as the cell membrane breaks, resulting in a unique process of cell death. These NET structures of neutrophils bindGram-positiveandGram-negative bacteria,as well as fungi, which confers broad specificity of neutrophils, explaining their role in the first line of defense once microbes have invaded.[10]
Dendritic cells
[edit]
The classification ofdendritic cellsas another type of white blood cell occurred over thirty-five years ago byRalph SteinmannandZanvil A. Cohnand has provided an essential link in the innate immune system.[11]Dendritic cells line airways and intestines, participate in a rich network making up part of theepidermal layerof the skin, and play a unique role in initiating a primary immune response. Dendritic cells are named after their structure that resembles that of a dendrite of anaxon,and they have two vital functions: displayantigens,which are recognized byT cellsand alert lymphocytes of the presence of an injury or infection. When the body is introduced to infection or injury, dendritic cells migrate to immune orlymphoid tissues.These two types of tissues are rich in T cells, the cells whose actions are induced by dendritic cells. Dendritic cells will capture antigens and engulf them through the process of phagocytosis. Dendritic cells containToll-like receptors(TLR) that will recognize a broad variety of microorganisms in the case of invasion.[12]The activation of these receptors stimulates specific antigen responses and development of antigen-specific adaptive immunity. A unique feature of dendritic cells is that they are able to open up thetight junctionsbetween epithelial cells and sample invaders themselves, all while maintaining the integrity of theepithelial barrierwith expression of their own tight-junction proteins. A real life example of dendritic cell functions is displayed in the rejection oforgan transplants.
References
[edit]- ^Alberts B. et al. Molecular Biology of the Cell. 4th edition. New York: Garland Science; 2002. Innate Immunity. Available from:https://www.ncbi.nlm.nih.gov/books/NBK26846/
- ^Lien, Egil; Ingalls, Robin (January 2002)."Toll-like Receptors".Society of Critical Care Medicine.30(1).
- ^Lodish, Harvey; Berk, Arnold; Kaiser, Chris; Krieger, Monty; Bretscher, Anthony; Ploegh, Hidde; Amon, Angelika; Scott, Matthew.Molecular Cell Biology(Seventh ed.). W.H. Freeman and Company. pp. 1062–1065.
- ^Muller, Michael."The Immune System".Retrieved15 November2015.
- ^Mayer, Gene."Innate (Non-specific) Immunity".Microbiology and Immunology Online.
- ^Mosser DM, Edwards JP (2008)."Exploring the full spectrum of macrophage activation".Nature Reviews Immunology.8(12): 958–969.doi:10.1038/nri2448.PMC2724991.PMID19029990.
- ^Elomaa, Outi; Sankala, Marko; Pikkarainen, Timo; Bergmann, Ulrich; Tuuttila, Ari; Sariola, Hannu; Trggvason, Karl; Raatikainen- Ahokas, Anne (20 February 1998)."Structure of the Human Macrophage MARCO Receptor and Characterization of its Bacteria-Binding Region".Journal of Biological Chemistry.273(8): 4530–4538.doi:10.1074/jbc.273.8.4530.PMID9468508.
- ^"Neutrophils".PubMed Health.National Cancer Institute.
- ^Brinkman, Volker; Reichard, Ulrike; Goosmann, Christian; Fauler, Beatrix; Uhlemann, Yvonne; Weiss, David; Weinrauch, Yvette; Zychlinsky, Arturo (24 December 2003). "Neutrophil Extracellular Traps Kill Bacteria".Science.303(5663): 1532–1535.Bibcode:2004Sci...303.1532B.doi:10.1126/science.1092385.PMID15001782.S2CID21628300.
- ^Fuchs Tobias A.; Abed Ulrike; Goosmann Christian; Hurwitz Robert; Schulze Ilka; Wahn Volker; Weinrauch Yvette; Brinkmann Volker; Zychlinsky Arturo (2007)."Novel cell death program leads to neutrophil extracellular traps".J Cell Biol.176(2): 231–241.doi:10.1083/jcb.200606027.PMC2063942.PMID17210947.
- ^"Laboratory of Cellular Biology and Physiology".The Rockefeller University.The Rockefeller University.Retrieved16 November2015.
- ^Takeda, Kiyoshi; Kaisho, Tsuneyasu; Akira, Shizuo (April 2003). "Toll-Like Receptors".Annual Review of Immunology.21:335–376.doi:10.1146/annurev.immunol.21.120601.141126.PMID12524386.
External links
[edit]- Nonspecific immune cellentry in the public domain National Cancer Institute Dictionary of Cancer Terms
![]() This article incorporatespublic domain materialfromDictionary of Cancer Terms.U.S. National Cancer Institute.
This article incorporatespublic domain materialfromDictionary of Cancer Terms.U.S. National Cancer Institute.
