Iobenguane
 | |
| Clinical data | |
|---|---|
| Trade names | Adreview, Azedra |
| Other names | meta-iodobenzylguanidine mIBG, MIBG |
| License data | |
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number |
|
| PubChemCID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard(EPA) | |
| Chemical and physical data | |
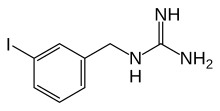
| Formula | C8H10IN3 |
| Molar mass | 275.093g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Iobenguane,orMIBG,is an aralkylguanidine analog of theadrenergic neurotransmitternorepinephrine(noradrenaline), typically used as aradiopharmaceutical.[3]It acts as a blocking agent foradrenergic neurons.Whenradiolabeled,it can be used innuclear medicinaldiagnostic and therapy techniques as well as inneuroendocrinechemotherapytreatments.
It localizes to adrenergic tissue and thus can be used to identify the location oftumorssuch aspheochromocytomasandneuroblastomas.[4]Withiodine-131it can also be used to treat tumor cells that take up and metabolize norepinephrine.
Usage and mechanism
[edit]MIBG is absorbed by and accumulated in granules of adrenal medullarychromaffin cells,as well as in pre-synaptic adrenergic neurongranules.The process in which this occurs is closely related to the mechanism employed by norepinephrine and its transporterin vivo.[5][6]Thenorepinephrine transporter(NET) functions to provide norepinephrineuptakeat thesynaptic terminalsand adrenal chromaffin cells. MIBG, by bonding to NET, finds its roles in imaging and therapy.
Metabolites and excretion
[edit]Less than 10% of the administered MIBG getsmetabolizedinto m-iodohippuric acid (MIHA), and the mechanism for how this metabolite is produced is unknown.[7]
Diagnostic imaging
[edit]

MIBG concentrates inendocrine tumors,most commonly neuroblastoma,paraganglioma,andpheochromocytoma.It also accumulates in norepinephrine transporters in adrenergic nerves in theheart,lungs,adrenal medulla,salivary glands,liver,andspleen,as well as in tumors that originate in theneural crest.When labelled withiodine-123it serves as a whole-body, non-invasivescintigraphicscreening forgerm-line,somatic,benign, and malignantneoplasmsoriginating in the adrenal glands. It can detect both intra and extra-adrenal disease. The imaging is highly sensitive and specific.[8][9]
Iobenguane concentrates in presynaptic terminals of the heart and otherautonomically innervatedorgans. This enables the possiblenon-invasiveuse as an in vivo probe to study these systems.[10][11]
Alternatives to imaging with123I-MIBG, for certain indications and under clinical and research use, include thepositron-emittingisotopeiodine-124,and other radiopharmaceuticals such as68Ga-DOTAand18F-FDOPAforpositron emission tomography(PET).[9][12][13]123I-MIBG imaging on agamma cameracan offer significantly higher cost-effectiveness and availability compared to PET imaging, and is particularly effective where131I-MIBG therapy is subsequently planned, due to their directly comparable uptake.[14][9][15]
Side effects
[edit]Side effects post imaging are rare but can includetachycardia,pallor,vomiting, and abdominal pain.[9]
Radionuclide therapy
[edit]MIBG can be radiolabelled with thebeta emittingradionuclide131I for the treatment of certain pheochromocytomas, paragangliomas,carcinoid tumors,neuroblastomas, andmedullary thyroid cancer.[16]
Thyroid precautions
[edit]Thyroid blockade with (nonradioactive) potassium iodide is indicated for nuclear medicine scintigraphy with iobenguane/mIBG. This competitively inhibits radioiodine uptake, preventing excessive radioiodine levels in the thyroid and minimizing risk of thyroid ablation (in treatment with131I). The minimal risk of thyroid cancer is also reduced as a result.[9][17]
The dosing regime for theFDA-approved commercial123I-MIBG product Adreview ispotassium iodideorLugol's solutioncontaining 100 mg iodide, weight adjusted for children and given an hour before injection.[18]EANMguidelines, endorsed by theSNMMI,suggest a variety of regimes in clinical use, for both children and adults.[9][12]
Product labeling for diagnostic131I iobenguane recommends giving potassium iodide one day before injection and continuing 5 to 7 days following.[19]131I iobenguane used for therapeutic purposes requires a different pre-medication duration, beginning 24–48 hours before iobenguane injection and continuing 10–15 days after injection.[16]
Clinical trials
[edit]Iobenguane I 131 for cancers
[edit]Iobenguane I 131, marketed under the trade nameAzedra,has had a clinical trial as a treatment for malignant, recurrent or unresectable pheochromocytoma and paraganglioma, and theFDAapprovedit on July 30, 2018. The drug is developed by Progenics Pharmaceuticals.[20][21]
References
[edit]- ^"Adreview- iobenguane i-123 injection".DailyMed.10 March 2020.Retrieved21 May2022.
- ^"Azedra- iobenguane i-131 injection, solution".DailyMed.8 April 2021.Retrieved21 May2022.
- ^Olecki E, Grant CN (December 2019). "MIBG in neuroblastoma diagnosis and treatment".Seminars in Pediatric Surgery.28(6): 150859.doi:10.1016/j.sempedsurg.2019.150859.PMID31931960.S2CID210191760.
- ^Scarsbrook AF, Ganeshan A, Statham J, Thakker RV, Weaver A, Talbot D, et al. (2007). "Anatomic and functional imaging of metastatic carcinoid tumors".Radiographics.27(2): 455–477.doi:10.1148/rg.272065058.PMID17374863.
- ^Beylergil V, Perez JA, Osborne JR (2016)."Molecular Imaging of Merkel Cell Carcinoma".In Hamblin MR, Avci P, Gupta GK (eds.).Imaging in dermatology.London. pp. 467–470.doi:10.1016/B978-0-12-802838-4.00033-9.ISBN978-0-12-802838-4.
Metaiodobenzylguanidine (MIBG) is a radiolabeled analogue of guanethidine that enters the cells via the norepinephrine transporter and is either stored in the cytoplasm or in secretory granules
{{cite book}}:CS1 maint: location missing publisher (link) - ^Davidoff AM (2010)."Neuroblastoma".In Holcomb GW, Murphy JP, Ostlie DJ (eds.).Ashcraft's pediatric surgery(5th ed.). Philadelphia: Saunders/Elsevier. pp. 872–894.doi:10.1016/B978-1-4160-6127-4.00068-9.ISBN978-1-4160-6127-4.
Metaiodobenzylguanidine (MIBG) is transported to and stored in the distal storage granules of chromaffin cells in the same way as norepinephrine.
- ^"Iobenguane".DrugBank Online.Retrieved19 August2021.fromWishart DS,Feunang YD, Guo AC, Lo EJ, Marcu A, Grant JR, et al. (January 2018)."DrugBank 5.0: a major update to the DrugBank database for 2018".Nucleic Acids Research.46(D1): D1074–D1082.doi:10.1093/nar/gkx1037.PMC5753335.PMID29126136.
- ^Vlachou FJ (2018)."SPECT in Adrenal Glands".In Gouliamos AD, Andreou JA, Kosmidis PA (eds.).Imaging in Clinical Oncology.Cham: Springer. p. 481.doi:10.1007/978-3-319-68873-2_70.ISBN978-3-319-68872-5.S2CID52922868.
- ^abcdefTaïeb D, Hicks RJ, Hindié E, Guillet BA, Avram A, Ghedini P, et al. (September 2019)."European Association of Nuclear Medicine Practice Guideline/Society of Nuclear Medicine and Molecular Imaging Procedure Standard 2019 for radionuclide imaging of phaeochromocytoma and paraganglioma".European Journal of Nuclear Medicine and Molecular Imaging.46(10): 2112–2137.doi:10.1007/s00259-019-04398-1.PMC7446938.PMID31254038.
- ^Das S, Gordián-Vélez WJ, Ledebur HC, Mourkioti F, Rompolas P, Chen HI, et al. (December 2020)."Innervation: the missing link for biofabricated tissues and organs".npj Regenerative Medicine.5(1): 11.doi:10.1038/s41536-020-0096-1.PMC7275031.PMID32550009.
- ^Sisson JC, Shapiro B, Meyers L, Mallette S, Mangner TJ, Wieland DM, et al. (October 1987)."Metaiodobenzylguanidine to map scintigraphically the adrenergic nervous system in man".Journal of Nuclear Medicine.28(10): 1625–1636.PMID3655915.
- ^abBar-Sever Z, Biassoni L, Shulkin B, Kong G, Hofman MS, Lopci E, et al. (October 2018)."Guidelines on nuclear medicine imaging in neuroblastoma".European Journal of Nuclear Medicine and Molecular Imaging.45(11): 2009–2024.doi:10.1007/s00259-018-4070-8.PMID29938300.S2CID49410438.
- ^Rufini V, Treglia G, Castaldi P, Perotti G, Giordano A (June 2013)."Comparison of metaiodobenzylguanidine scintigraphy with positron emission tomography in the diagnostic work-up of pheochromocytoma and paraganglioma: a systematic review".The Quarterly Journal of Nuclear Medicine and Molecular Imaging.57(2): 122–133.PMID23822989.
- ^Čtvrtlík F, Koranda P, Schovánek J, Škarda J, Hartmann I, Tüdös Z (April 2018)."Current diagnostic imaging of pheochromocytomas and implications for therapeutic strategy".Experimental and Therapeutic Medicine.15(4): 3151–3160.doi:10.3892/etm.2018.5871.PMC5840941.PMID29545830.
- ^Ballinger JR (November 2018)."Theranostic radiopharmaceuticals: established agents in current use".The British Journal of Radiology.91(1091): 20170969.doi:10.1259/bjr.20170969.PMC6475961.PMID29474096.
- ^abGiammarile F, Chiti A, Lassmann M, Brans B, Flux G (May 2008). "EANM procedure guidelines for 131I-meta-iodobenzylguanidine (131I-mIBG) therapy".European Journal of Nuclear Medicine and Molecular Imaging.35(5): 1039–1047.doi:10.1007/s00259-008-0715-3.PMID18274745.S2CID6884201.
- ^Van Vickle SS, Thompson RC (June 2015)."123I-MIBG Imaging: Patient Preparation and Technologist's Role".Journal of Nuclear Medicine Technology.43(2): 82–86.doi:10.2967/jnmt.115.158394.PMID25956690.
- ^"Drug Approval Package: AdreView (Iobenguane I 123) NDA # 022290".U.S. Food and Drug Administration.2008.Retrieved19 August2021.
- ^"Iobenguane Sulfate I 131 Injection Diagnostic package insert".Bedford, MA: CIS-US, Inc. July 1999 – via Drugs.com.
- ^"AZEDRA® (iobenguane I 131".Billerica, MA: Progenics Pharmaceuticals Inc., a Lantheus company. July 2018. Archived fromthe originalon 2019-08-17.Retrieved2018-08-03.
- ^"FDA approves first treatment for rare adrenal tumors".U.S. Food and Drug Administration.30 July 2018.
External links
[edit]- "iobenguane I 131".NCI Drug Dictionary.
- "Iobenguane I 131".National Cancer Institute.15 August 2018.
