MRI pulse sequence

AnMRI pulse sequenceinmagnetic resonance imaging(MRI) is a particular setting of pulse sequences andpulsed field gradients,resulting in a particular image appearance.[1]
A multiparametric MRI is a combination of two or more sequences, and/or includingother specialized MRI configurationssuch asspectroscopy.[2][3]
Overview table
This table does not includeuncommon and experimental sequences.
| Group | Sequence | Abbr. | Physics | Main clinical distinctions | Example |
|---|---|---|---|---|---|
| Spin echo | T1 weighted | T1 | Measuringspin–lattice relaxationby using a shortrepetition time(TR) andecho time(TE). |
Standard foundation and comparison for other sequences |

|
| T2 weighted | T2 | Measuringspin–spin relaxationby using long TR and TE times |
Standard foundation and comparison for other sequences |

| |
| Proton density weighted | PD | LongTR(to reduce T1) and shortTE(to minimize T2).[7] | Joint diseaseand injury.[8]
|

| |
| Gradient echo(GRE) | Steady-state free precession | SSFP | Maintenance of a steady, residual transverse magnetisation over successive cycles.[10] | Creation ofcardiac MRIvideos (pictured).[10] | 
|
| Effective T2 or "T2-star" |
T2* | Spoiled gradient recalled echo (GRE) with a long echo time and small flip angle[11] | Low signal fromhemosiderindeposits (pictured) and hemorrhages.[11] | 
| |
| Susceptibility-weighted | SWI | Spoiled gradient recalled echo (GRE), fully flow compensated, long echo time, combines phase image with magnitude image[12] | Detecting small amounts of hemorrhage (diffuse axonal injurypictured) or calcium.[12] | 
| |
| Inversion recovery | Short tau inversion recovery | STIR | Fat suppression by setting aninversion timewhere the signal of fat is zero.[13] | High signal inedema,such as in more severestress fracture.[14]Shin splintspictured: | 
|
| Fluid-attenuated inversion recovery | FLAIR | Fluid suppression by setting an inversion time that nulls fluids | High signal inlacunar infarction,multiple sclerosis (MS) plaques,subarachnoid haemorrhageandmeningitis(pictured).[15] | 
| |
| Double inversion recovery | DIR | Simultaneous suppression ofcerebrospinal fluidandwhite matterby two inversion times.[16] | High signal ofmultiple sclerosisplaques (pictured).[16] | 
| |
| Diffusion weighted(DWI) | Conventional | DWI | Measure ofBrownian motionof water molecules.[17] | High signal within minutes ofcerebral infarction(pictured).[18] | 
|
| Apparent diffusion coefficient | ADC | Reduced T2 weighting by taking multiple conventional DWI images with different DWI weighting, and the change corresponds to diffusion.[19] | Low signal minutes aftercerebral infarction(pictured).[20] | 
| |
| Diffusion tensor | DTI | Mainlytractography(pictured) by an overall greaterBrownian motionof water molecules in the directions of nerve fibers.[21] |
|

| |
| Perfusion weighted(PWI) | Dynamic susceptibility contrast | DSC | Measures changes over time in susceptibility-induced signal loss due togadolinium contrastinjection.[23] |
|

|
| Arterial spin labelling | ASL | Magnetic labeling of arterial blood below the imaging slab, which subsequently enters the region of interest.[25]It does not need gadolinium contrast.[26] | |||
| Dynamic contrast enhanced | DCE | Measures changes over time in the shortening of thespin–lattice relaxation(T1) induced by agadolinium contrastbolus.[27] | Faster Gd contrast uptake along with other features is suggestive of malignancy (pictured).[28] | 
| |
| Functional MRI(fMRI) | Blood-oxygen-level dependentimaging | BOLD | Changes inoxygen saturation-dependent magnetism ofhemoglobinreflects tissue activity.[29] | Localizing brain activity from performing an assigned task (e.g. talking, moving fingers) before surgery, also used in research of cognition.[30] | 
|
| Magnetic resonance angiography(MRA) and venography | Time-of-flight | TOF | Blood entering the imaged area is not yetmagnetically saturated,giving it a much higher signal when using short echo time and flow compensation. | Detection ofaneurysm,stenosis,ordissection[31] | 
|
| Phase-contrast magnetic resonance imaging | PC-MRA | Two gradients with equal magnitude, but opposite direction, are used to encode a phase shift, which is proportional to the velocity ofspins.[32] | Detection ofaneurysm,stenosis,ordissection(pictured).[31] |  (VIPR) |
Spin echo
[edit]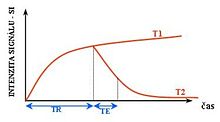

T1 and T2
[edit]Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 (spin-lattice;that is, magnetization in the same direction as the static magnetic field) and T2 (spin-spin;transverse to the static magnetic field). To create a T1-weighted image, magnetization is allowed to recover before measuring the MR signal by changing therepetition time(TR). This image weighting is useful for assessing the cerebral cortex, identifying fatty tissue, characterizing focal liver lesions, and in general, obtaining morphological information, as well as forpost-contrastimaging. To create a T2-weighted image, magnetization is allowed to decay before measuring the MR signal by changing theecho time(TE). This image weighting is useful for detectingedemaand inflammation, revealingwhite matter lesions,and assessing zonal anatomy in theprostateanduterus.
The standard display of MRI images is to represent fluid characteristics inblack and whiteimages, where different tissues turn out as follows:
| Signal | T1-weighted | T2-weighted |
|---|---|---|
| High |
|
|
| Inter- mediate | Grey matterdarker thanwhite matter[35] | White matterdarker thangrey matter[35] |
| Low |
|
|
Proton density
[edit]
Proton density (PD)- weighted images are created by having a long repetition time (TR) and a short echo time (TE).[36]On images of the brain, this sequence has a more pronounced distinction betweengrey matter(bright) andwhite matter(darker grey), but with little contrast between brain and CSF.[36]It is very useful for the detection ofarthropathyand injury.[37]
Gradient echo
[edit]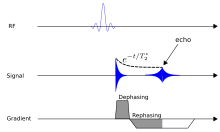
Agradient echo sequencedoes not use a 180 degrees RF pulse to make the spins of particles coherent. Instead, it uses magnetic gradients to manipulate the spins, allowing the spins to dephase and rephase when required. After an excitation pulse, the spins are dephased, no signal is produced because the spins are not coherent. When the spins are rephased, they become coherent, and thus signal (or "echo" ) is generated to form images. Unlike spin echo, gradient echo does not need to wait for transverse magnetisation to decay completely before initiating another sequence, thus it requires very short repetition times (TR), and therefore to acquire images in a short time. After echo is formed, some transverse magnetisations remains. Manipulating gradients during this time will produce images with different contrast. There are three main methods of manipulating contrast at this stage, namely steady-state free-precession (SSFP) that does not spoil the remaining transverse magnetisation, but attempts to recover them (thus producing T2-weighted images); the sequence with spoiler gradient that averages the transverse magnetisations (thus producing mixed T1 and T2-weighted images), and RF spoiler that vary the phases of RF pulse to eliminates the transverse magnetisation, thus producing pure T1-weighted images.[39]
For comparison purposes, the repetition time of a gradient echo sequence is of the order of 3 milliseconds, versus about 30 ms of a spin echo sequence.[citation needed]
Inversion recovery
[edit]Inversion recoveryis an MRI sequence that provides high contrast between tissue and lesion. It can be used to provide high T1 weighted image, high T2 weighted image, and to suppress the signals from fat, blood, orcerebrospinal fluid(CSF).[40]
Diffusion weighted
[edit]
Diffusion MRImeasures thediffusionof water molecules in biological tissues.[41]Clinically, diffusion MRI is useful for the diagnoses of conditions (e.g.,stroke) or neurological disorders (e.g.,multiple sclerosis), and helps better understand the connectivity of white matter axons in the central nervous system.[42]In anisotropicmedium (inside a glass of water for example), water molecules naturally move randomly according toturbulenceandBrownian motion.In biological tissues however, where theReynolds numberis low enough forlaminar flow,the diffusion may beanisotropic.For example, a molecule inside theaxonof a neuron has a low probability of crossing themyelinmembrane. Therefore, the molecule moves principally along the axis of the neural fiber. If it is known that molecules in a particularvoxeldiffuse principally in one direction, the assumption can be made that the majority of the fibers in this area are parallel to that direction.
The recent development ofdiffusion tensor imaging(DTI)[43]enables diffusion to be measured in multiple directions, and the fractional anisotropy in each direction to be calculated for each voxel. This enables researchers to make brain maps of fiber directions to examine the connectivity of different regions in the brain (usingtractography) or to examine areas of neural degeneration and demyelination in diseases like multiple sclerosis.
Another application of diffusion MRI isdiffusion-weighted imaging(DWI). Following an ischemicstroke,DWI is highly sensitive to the changes occurring in the lesion.[44]It is speculated that increases in restriction (barriers) to water diffusion, as a result of cytotoxic edema (cellular swelling), is responsible for the increase in signal on a DWI scan. The DWI enhancement appears within 5–10 minutes of the onset ofstroke symptoms(as compared tocomputed tomography,which often does not detect changes of acute infarct for up to 4–6 hours) and remains for up to two weeks. Coupled with imaging of cerebral perfusion, researchers can highlight regions of "perfusion/diffusion mismatch" that may indicate regions capable of salvage by reperfusion therapy.
Like many other specialized applications, this technique is usually coupled with a fast image acquisition sequence, such asecho planar imagingsequence.
Perfusion weighted
[edit]
Perfusion-weighted imaging(PWI) is performed by 3 main techniques:
- Dynamic susceptibility contrast (DSC):Gadolinium contrastis injected, and rapid repeated imaging (generally gradient-echo echo-planarT2 weighted) quantifies susceptibility-induced signal loss.[45]
- Dynamic contrast enhanced (DCE): Measuring shortening of thespin–lattice relaxation(T1) induced by agadolinium contrastbolus.[46]
- Arterial spin labelling (ASL): Magnetic labeling of arterial blood below the imaging slab, without the need of gadolinium contrast.[47]
The acquired data is then postprocessed to obtain perfusion maps with different parameters, such as BV (blood volume), BF (blood flow), MTT (mean transit time) and TTP (time to peak).
Incerebral infarction,thepenumbrahas decreased perfusion.[24]Another MRI sequence,diffusion-weighted MRI,estimates the amount of tissue that is already necrotic, and the combination of those sequences can therefore be used to estimate the amount of brain tissue that is salvageable bythrombolysisand/orthrombectomy.
Functional MRI
[edit]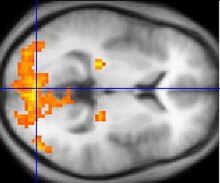
Functional MRI(fMRI) measures signal changes in thebrainthat are due to changingneuralactivity. It is used to understand how different parts of the brain respond to externalstimulior passive activity in a resting state, and has applications inbehavioralandcognitive research,and in planningneurosurgeryofeloquent brain areas.[48][49]Researchers use statistical methods to construct a 3-Dparametric mapof the brain indicating the regions of the cortex that demonstrate a significant change in activity in response to the task. Compared to anatomical T1W imaging, the brain is scanned at lower spatial resolution but at a higher temporal resolution (typically once every 2–3 seconds). Increases in neural activity cause changes in the MR signal viaT*
2changes;[50]this mechanism is referred to as the BOLD (blood-oxygen-level dependent) effect. Increased neural activity causes an increased demand for oxygen, and thevascularsystem actually overcompensates for this, increasing the amount of oxygenatedhemoglobinrelative to deoxygenated hemoglobin. Because deoxygenated hemoglobin attenuates the MR signal, the vascular response leads to a signal increase that is related to the neural activity. The precise nature of the relationship between neural activity and the BOLD signal is a subject of current research. The BOLD effect also allows for the generation of high resolution 3D maps of the venous vasculature within neural tissue.
While BOLD signal analysis is the most common method employed for neuroscience studies in human subjects, the flexible nature of MR imaging provides means to sensitize the signal to other aspects of the blood supply. Alternative techniques employarterial spin labeling(ASL) or weighting the MRI signal by cerebral blood flow (CBF) and cerebral blood volume (CBV). The CBV method requires injection of a class of MRIcontrast agentsthat are now in human clinical trials. Because this method has been shown to be far more sensitive than the BOLD technique in preclinical studies, it may potentially expand the role of fMRI in clinical applications. The CBF method provides more quantitative information than the BOLD signal, albeit at a significant loss of detection sensitivity.[citation needed]
Magnetic resonance angiography
[edit]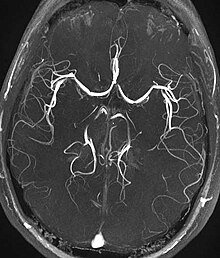
Magnetic resonance angiography(MRA) is a group of techniques based to image blood vessels. Magnetic resonance angiography is used to generate images of arteries (and less commonly veins) in order to evaluate them forstenosis(abnormal narrowing),occlusions,aneurysms(vessel wall dilatations, at risk of rupture) or other abnormalities. MRA is often used to evaluate the arteries of the neck and brain, the thoracic and abdominal aorta, the renal arteries, and the legs (the latter exam is often referred to as a "run-off" ).
Phase contrast
[edit]Phase contrast MRI (PC-MRI) is used to measure flow velocities in the body. It is used mainly to measure blood flow in the heart and throughout the body. PC-MRI may be considered a method ofmagnetic resonance velocimetry.Since modern PC-MRI typically is time-resolved, it also may be referred to as 4-D imaging (three spatialdimensionsplus time).[51]
Susceptibility weighted imaging
[edit]Susceptibility-weighted imaging (SWI) is a new type of contrast in MRI different from spin density,T1,orT2imaging. This method exploits the susceptibility differences between tissues and uses a fully velocity-compensated, three-dimensional, RF-spoiled, high-resolution, 3D-gradient echo scan. This special data acquisition and image processing produces an enhanced contrast magnitude image very sensitive to venous blood,hemorrhageand iron storage. It is used to enhance the detection and diagnosis of tumors, vascular and neurovascular diseases (stroke and hemorrhage), multiple sclerosis,[52]Alzheimer's, and also detects traumatic brain injuries that may not be diagnosed using other methods.[53]
Magnetization transfer
[edit]Magnetization transfer (MT) is a technique to enhance image contrast in certain applications of MRI.
Boundprotonsare associated withproteinsand as they have a very short T2 decay they do not normally contribute to image contrast. However, because these protons have a broad resonance peak they can be excited by a radiofrequency pulse that has no effect on free protons. Their excitation increases image contrast by transfer ofsaturatedspinsfrom the bound pool into the free pool, thereby reducing the signal of free water. This homonuclear magnetization transfer provides an indirect measurement ofmacromolecularcontent in tissue. Implementation of homonuclear magnetization transfer involves choosing suitable frequency offsets and pulse shapes to saturate the bound spins sufficiently strongly, within the safety limits ofspecific absorption ratefor MRI.[54]
The most common use of this technique is for suppression of background signal in time of flight MR angiography.[55]There are also applications in neuroimaging particularly in the characterization of white matter lesions inmultiple sclerosis.[56]
Fat suppression
[edit]Fat suppression is useful for example to distinguish active inflammation in the intestines from fat deposition such as can be caused by long-standing (but possibly inactive)inflammatory bowel disease,but alsoobesity,chemotherapyandceliac disease.[57]Without fat suppression techniques, fat and fluid will have similar signal intensities on fast spin-echo sequences.[58]
Techniques to suppress fat on MRI mainly include:[59]
- Identifying fat by thechemical shiftof its atoms, causing different time-dependent phase shifts compared to water.
- Frequency-selective saturation of the spectral peak of fat by a "fat sat" pulse before imaging.
- Short tau inversion recovery (STIR), aT1-dependent method
- Spectral presaturation with inversion recovery (SPIR)
Neuromelanin imaging
[edit]This method exploits theparamagneticproperties ofneuromelaninand can be used to visualize thesubstantia nigraand thelocus coeruleus.It is used to detect theatrophyof these nuclei inParkinson's diseaseand otherparkinsonisms,and also detects signal intensity changes inmajor depressive disorderandschizophrenia.[60]
Uncommon and experimental sequences
[edit]The following sequences are not commonly used clinically, and/or are at an experimental stage.
T1 rho (T1ρ)
[edit]T1 rho (T1ρ) is an experimental MRI sequence that may be used in musculoskeletal imaging. It does not yet have widespread use.[61]
Molecules have akinetic energythat is a function of the temperature and is expressed as translational and rotational motions, and by collisions between molecules. The moving dipoles disturb the magnetic field but are often extremely rapid so that the average effect over a long time-scale may be zero. However, depending on the time-scale, the interactions between the dipoles do not always average away. At the slowest extreme the interaction time is effectively infinite and occurs where there are large, stationary field disturbances (e.g., a metallic implant). In this case the loss of coherence is described as a "static dephasing". T2* is a measure of the loss of coherence in an ensemble of spins that includes all interactions (including static dephasing). T2 is a measure of the loss of coherence that excludes static dephasing, using an RF pulse to reverse the slowest types of dipolar interaction. There is in fact a continuum of interaction time-scales in a given biological sample, and the properties of the refocusing RF pulse can be tuned to refocus more than just static dephasing. In general, the rate of decay of an ensemble of spins is a function of the interaction times and also the power of the RF pulse. This type of decay, occurring under the influence of RF, is known as T1ρ. It is similar to T2 decay but with some slower dipolar interactions refocused, as well as static interactions, hence T1ρ≥T2.[62]
Others
[edit]- Saturation recovery sequencesare rarely used, but can measurespin-lattice relaxation time(T1) more quickly than an inversion recovery pulse sequence.[63]
- Double-oscillating-diffusion-encoding(DODE) anddouble diffusion encoding(DDE) imaging are specific forms of MRI diffusion imaging, which can be used to measure diameters and lengths ofaxon pores.[64]
References
[edit]- ^Jones J, Gaillard F."MRI sequences (overview)".Radiopaedia.Retrieved2017-10-15.
- ^Marino MA, Helbich T, Baltzer P, Pinker-Domenig K (February 2018)."Multiparametric MRI of the breast: A review".Journal of Magnetic Resonance Imaging.47(2): 301–315.doi:10.1002/jmri.25790.PMID28639300.S2CID206108382.
- ^Tahmassebi A, Wengert GJ, Helbich TH, Bago-Horvath Z, Alaei S, Bartsch R, et al. (February 2019)."Impact of Machine Learning With Multiparametric Magnetic Resonance Imaging of the Breast for Early Prediction of Response to Neoadjuvant Chemotherapy and Survival Outcomes in Breast Cancer Patients".Investigative Radiology.54(2): 110–117.doi:10.1097/RLI.0000000000000518.PMC6310100.PMID30358693.
- ^abcd"Magnetic Resonance Imaging".University of Wisconsin.Archived fromthe originalon 2017-05-10.Retrieved2016-03-14.
- ^abcdJohnson KA."Basic proton MR imaging. Tissue Signal Characteristics".Harvard Medical School.Archived fromthe originalon 2016-03-05.Retrieved2016-03-14.
- ^"MRI Questions, Fast Spin Echo".MRIQuestions.com.Retrieved2021-05-18.
- ^Graham D, Cloke P, Vosper M (2011-05-31).Principles and Applications of Radiological Physics E-Book(6 ed.). Elsevier Health Sciences. p. 292.ISBN978-0-7020-4614-8.}
- ^du Plessis V, Jones J."MRI sequences (overview)".Radiopaedia.Retrieved2017-01-13.
- ^Lefevre N, Naouri JF, Herman S, Gerometta A, Klouche S, Bohu Y (2016)."A Current Review of the Meniscus Imaging: Proposition of a Useful Tool for Its Radiologic Analysis".Radiology Research and Practice.2016:8329296.doi:10.1155/2016/8329296.PMC4766355.PMID27057352.
- ^abLuijkx T, Weerakkody Y."Steady-state free precession MRI".Radiopaedia.Retrieved2017-10-13.
- ^abChavhan GB, Babyn PS, Thomas B, Shroff MM, Haacke EM (2009)."Principles, techniques, and applications of T2*-based MR imaging and its special applications".Radiographics.29(5): 1433–49.doi:10.1148/rg.295095034.PMC2799958.PMID19755604.
- ^abDi Muzio B, Gaillard F."Susceptibility weighted imaging".Retrieved2017-10-15.
- ^Sharma R, Taghi Niknejad M."Short tau inversion recovery".Radiopaedia.Retrieved2017-10-13.
- ^Berger F, de Jonge M, Smithuis R, Maas M."Stress fractures".Radiology Assistant.Radiology Society of the Netherlands.Retrieved2017-10-13.
- ^Hacking C, Taghi Niknejad M, et al."Fluid attenuation inversion recoveryg".radiopaedia.org.Retrieved2015-12-03.
- ^abDi Muzio B, Abd Rabou A."Double inversion recovery sequence".Radiopaedia.Retrieved2017-10-13.
- ^Lee M, Bashir U."Diffusion weighted imaging".Radiopaedia.Retrieved2017-10-13.
- ^Weerakkody Y, Gaillard F."Ischaemic stroke".Radiopaedia.Retrieved2017-10-15.
- ^Hammer M."MRI Physics: Diffusion-Weighted Imaging".XRayPhysics.Retrieved2017-10-15.
- ^An H, Ford AL, Vo K, Powers WJ, Lee JM, Lin W (May 2011)."Signal evolution and infarction risk for apparent diffusion coefficient lesions in acute ischemic stroke are both time- and perfusion-dependent".Stroke.42(5): 1276–81.doi:10.1161/STROKEAHA.110.610501.PMC3384724.PMID21454821.
- ^abSmith D, Bashir U."Diffusion tensor imaging".Radiopaedia.Retrieved2017-10-13.
- ^Chua TC, Wen W, Slavin MJ, Sachdev PS (February 2008). "Diffusion tensor imaging in mild cognitive impairment and Alzheimer's disease: a review".Current Opinion in Neurology.21(1): 83–92.doi:10.1097/WCO.0b013e3282f4594b.PMID18180656.S2CID24731783.
- ^Gaillard F."Dynamic susceptibility contrast (DSC) MR perfusion".Radiopaedia.Retrieved2017-10-14.
- ^abChen F, Ni YC (March 2012)."Magnetic resonance diffusion-perfusion mismatch in acute ischemic stroke: An update".World Journal of Radiology.4(3): 63–74.doi:10.4329/wjr.v4.i3.63.PMC3314930.PMID22468186.
- ^"Arterial spin labeling".University of Michigan.Retrieved2017-10-27.
- ^Gaillard F."Arterial spin labelling (ASL) MR perfusion".Radiopaedia.Retrieved2017-10-15.
- ^Gaillard F."Dynamic contrast enhanced (DCE) MR perfusion".Radiopaedia.Retrieved2017-10-15.
- ^Turnbull LW (January 2009). "Dynamic contrast-enhanced MRI in the diagnosis and management of breast cancer".NMR in Biomedicine.22(1): 28–39.doi:10.1002/nbm.1273.PMID18654999.S2CID5305422.
- ^Chou Ih."Milestone 19: (1990) Functional MRI".Nature.Retrieved9 August2013.
- ^Luijkx T, Gaillard F."Functional MRI".Radiopaedia.Retrieved2017-10-16.
- ^ab"Magnetic Resonance Angiography (MRA)".Johns Hopkins Hospital.Retrieved2017-10-15.
- ^Keshavamurthy J, Ballinger R et al."Phase contrast imaging".Radiopaedia.Retrieved2017-10-15.
- ^abcdefgh"Magnetic Resonance Imaging".University of Wisconsin.Archived fromthe originalon 2017-05-10.Retrieved2016-03-14.
- ^abcdefghijklmnJohnson KA."Basic proton MR imaging. Tissue Signal Characteristics".Harvard Medical School.Archived fromthe originalon 2016-03-05.Retrieved2016-03-14.
- ^abPatil T (2013-01-18)."MRI sequences".Retrieved2016-03-14.
- ^ab"Structural MRI Imaging".UC San Diego School of Medicine.Retrieved2017-01-01.
- ^Jones J, Gaillard F."MRI sequences (overview)".Radiopaedia.Retrieved2017-01-13.
- ^Gebker R, Schwitter J, Fleck E, Nagel E (2007). "How we perform myocardial perfusion with cardiovascular magnetic resonance".Journal of Cardiovascular Magnetic Resonance.9(3): 539–547.CiteSeerX10.1.1.655.7675.doi:10.1080/10976640600897286.PMID17365233.
- ^Hargreaves BA (December 2012)."Rapid gradient-echo imaging".Journal of Magnetic Resonance Imaging.36(6): 1300–1313.doi:10.1002/jmri.23742.PMC3502662.PMID23097185.
- ^Bydder GM,Hajnal JV, Young IR (March 1998). "MRI: use of the inversion recovery pulse sequence".Clinical Radiology.53(3): 159–76.doi:10.1016/s0009-9260(98)80096-2.PMID9528866.
- ^Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (November 1986). "MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders".Radiology.161(2): 401–407.doi:10.1148/radiology.161.2.3763909.PMID3763909.S2CID14420005.
- ^"Diffusion Inaging".Stanford University. Archived fromthe originalon 24 December 2011.Retrieved28 April2012.
- ^Filler A (2009)."The History, Development and Impact of Computed Imaging in Neurological Diagnosis and Neurosurgery: CT, MRI, and DTI".Nature Precedings.doi:10.1038/npre.2009.3267.4.
- ^ Moseley ME, Cohen Y, Mintorovitch J, Chileuitt L, Shimizu H, Kucharczyk J, et al. (May 1990). "Early detection of regional cerebral ischemia in cats: comparison of diffusion- and T2-weighted MRI and spectroscopy".Magnetic Resonance in Medicine.14(2): 330–346.doi:10.1002/mrm.1910140218.PMID2345513.S2CID23754356.
- ^Gaillard F."Dynamic susceptibility contrast (DSC) MR perfusion".Radiopaedia.Retrieved2017-10-14.
- ^Gaillard F, Goel A, Murphy A."Dynamic contrast enhanced (DCE) MR perfusion".Radiopaedia.Retrieved2017-10-15.
- ^Gaillard F."Arterial spin labelling (ASL) MR perfusion".Radiopaedia.Retrieved2017-10-15.
- ^Heeger DJ, Ress D (February 2002)."What does fMRI tell us about neuronal activity?".Nature Reviews. Neuroscience.3(2): 142–151.doi:10.1038/nrn730.PMID11836522.S2CID7132655.
- ^Giussani C, Roux FE, Ojemann J, Sganzerla EP, Pirillo D, Papagno C (January 2010). "Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies".Neurosurgery.66(1): 113–120.doi:10.1227/01.NEU.0000360392.15450.C9.PMID19935438.S2CID207142804.
- ^Thulborn KR, Waterton JC, Matthews PM, Radda GK (February 1982). "Oxygenation dependence of the transverse relaxation time of water protons in whole blood at high field".Biochimica et Biophysica Acta (BBA) - General Subjects.714(2): 265–270.doi:10.1016/0304-4165(82)90333-6.PMID6275909.
- ^Stankovic Z, Allen BD, Garcia J, Jarvis KB, Markl M (April 2014)."4D flow imaging with MRI".Cardiovascular Diagnosis and Therapy.4(2): 173–192.doi:10.3978/j.issn.2223-3652.2014.01.02.PMC3996243.PMID24834414.
- ^Wiggermann V, Hernández Torres E, Vavasour IM, Moore GR, Laule C, MacKay AL, et al. (July 2013)."Magnetic resonance frequency shifts during acute MS lesion formation".Neurology.81(3): 211–218.doi:10.1212/WNL.0b013e31829bfd63.PMC3770162.PMID23761621.
- ^Reichenbach JR, Venkatesan R, Schillinger DJ, Kido DK, Haacke EM (July 1997). "Small vessels in the human brain: MR venography with deoxyhemoglobin as an intrinsic contrast agent".Radiology.204(1): 272–277.doi:10.1148/radiology.204.1.9205259.PMID9205259.[permanent dead link]
- ^McRobbie DW (2007).MRI from picture to proton.Cambridge, UK; New York: Cambridge University Press.ISBN978-0-521-68384-5.
- ^Wheaton AJ, Miyazaki M (August 2012)."Non-contrast enhanced MR angiography: physical principles".Journal of Magnetic Resonance Imaging.36(2): 286–304.doi:10.1002/jmri.23641.PMID22807222.S2CID24048799.
- ^Filippi M, Rocca MA, De Stefano N, Enzinger C, Fisher E, Horsfield MA, et al. (December 2011)."Magnetic resonance techniques in multiple sclerosis: the present and the future".Archives of Neurology.68(12): 1514–1520.doi:10.1001/archneurol.2011.914.PMID22159052.
- ^Gore R, Smithuis R (2014-05-21)."Bowel wall thickening – CT-pattern – Type 4 – Fat target sign".Radiology Assistant.Retrieved2017-09-27.
- ^Bloem JL, Reijnierse M, Huizinga TW, van der Helm-van Mil AH (June 2018)."MR signal intensity: staying on the bright side in MR image interpretation".RMD Open.4(1): e000728.doi:10.1136/rmdopen-2018-000728.PMC6018882.PMID29955387.
- ^Weishaupt D, Koechli VD, Marincek B (2008)."Chapter 9: Fast Suppression Techniques".How does MRI work?: An Introduction to the Physics and Function of Magnetic Resonance Imaging(2nd ed.). Springer Science & Business Media. p. 70.ISBN978-3-540-37845-7.
- ^Sasaki M, Shibata E, Tohyama K, Takahashi J, Otsuka K, Tsuchiya K, et al. (July 2006). "Neuromelanin magnetic resonance imaging of locus ceruleus and substantia nigra in Parkinson's disease".NeuroReport.17(11): 1215–1218.doi:10.1097/01.wnr.0000227984.84927.a7.PMID16837857.S2CID24597825.
- ^Luijkx T, Morgan MA."T1 rho".Radiopaedia.Retrieved2017-10-15.
- ^Borthakur A, Mellon E, Niyogi S, Witschey W, Kneeland JB, Reddy R (November 2006)."Sodium and T1rho MRI for molecular and diagnostic imaging of articular cartilage".NMR in Biomedicine.19(7): 781–821.doi:10.1002/nbm.1102.PMC2896046.PMID17075961.
- ^Jones J, Ballinger JR."Saturation recovery sequences".Radiopaedia.Retrieved2017-10-15.
- ^Andrada I, Ivana D, Noam S, Daniel A (2016)."Advanced diffusion MRI for microstructure imaging".Frontiers in Physics.4.doi:10.3389/conf.FPHY.2016.01.00001.
