Maprotiline
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Ludiomil, others |
| Other names | Maprotiline hydrochloride; Maprotiline methanesulfonate; Ba 34276[1][2][3] |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682158 |
| Routes of administration | Oral,intramuscular,intravenous |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokineticdata | |
| Bioavailability | 66–70% |
| Protein binding | 88% |
| Metabolism | hepatic |
| Onset of action | 6 hours |
| Eliminationhalf-life | 27–58 hours |
| Excretion | Urine(57%) andbile(30%) asglucuronides,3–4% as unchanged drug |
| Identifiers | |
| |
| CAS Number |
|
| PubChemCID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard(EPA) | |
| ECHA InfoCard | 100.030.532 |
| Chemical and physical data | |
| Formula | C20H23N |
| Molar mass | 277.411g·mol−1 |
| 3D model (JSmol) | |
| |
| |
Maprotiline,sold under the brand nameLudiomilamong others, is atetracyclic antidepressant(TeCA) that is used in the treatment ofdepression.[5]It may alternatively be classified as atricyclic antidepressant(TCA), specifically asecondary amine.[5]In terms of itschemistryandpharmacology,maprotiline is closely related to such-other secondary-amine TCAs asnortriptylineandprotriptylineand has similar effects to them,[6][5]albeit with more distinctanxiolyticeffects.[7][8][9]Additionally, whereasprotriptylinetends to be somewhat more stimulating and in any case is distinctly more-or-less non-sedating,[10]mild degrees of sedation may be experienced with maprotiline.[11]
Medical uses
[edit]Maprotiline is used in the treatment of depression, such as depression associated with agitation or anxiety and has similar efficacy to the antidepressant drugmoclobemide.[12]This finding has also been validated by a group ofgeneral practitionerswho compared the respective efficacy and tolerability of maprotiline andmoclobemide.[13]
- Treatment ofdepressionof all forms and severities (endogenous,psychotic,involutional,andneurotic), especially depression associated with agitation or anxiety
- Panic disorder
- Neuropathic pain,including painfulpolyneuropathyin diabetics and non-diabetics alike.[14]
- Treatment of the depressive phase ofbipolar affective disorder
- For the symptomatic relief ofanxiety,tensionorinsomnia
The use of maprotiline in the treatment ofenuresisinpediatricpatients has so far not been systematically explored and its use is not recommended.[15]Safety and effectiveness in the pediatric population in general have not been established. Anyone considering the use of maprotiline in a child or adolescent must balance the potential risks with the clinical need.
A very small body of research has also explored the potential of maprotiline in treatingdiabetic kidney disease[16]and it has been measured againstamitriptylinein this regard.[17]
Maprotiline andfluoxetinehave also been found, among certain lines of research, to have quite potent anti-profilerative effects against certain forms of cancer of theBurkitt lymphomatype.[18][19]One study also bore ought a certain level of evidence regarding maprotiline’s ability to suppress bothcholesterolbiosynthesis andhepatocellular carcinomaliver-cancer progression.
Maprotiline was also measured againstimipramine,fluoxetineandketaminein an experiment-model involving two different kinds ofchickendifferently-conditioned againststress,including (black)Australorpsin the proposed treatment of treatment-resistant depression in humans.[20]
In general, lower dosages are recommended for patients over 60 years of age. Dosages of 50 mg to 75 mg daily are usually satisfactory as maintenance therapy for elderly patients who do not tolerate higher amounts.[21][22]In any case, 225 m.g./d. is the absolute-maximum highest recommended dose for this drug, as any more can predispose more significantly to seizures. 150 m.g. is the average optimal daily dose for otherwise-healthy patients who can tolerate a full dose.
Available forms
[edit]- Coated tablets: 10 mg, 25 mg, 50 mg, and 75 mg
- Injectable concentrate, 25 mg
Contraindications
[edit]In generalised theory, maprotiline (as with other tricyclic antidepressants, besidestrimipramine[23][24][25]and possiblyclomipramine) may somewhat worsen certain features of schizophrenia, necessitating caution in prescribing them to someone with it and continuation of the antipsychotic treatment (e.g., withrisperidoneorolanzapine). However, certain bodies of evidence have found maprotiline a useful augment in treating some of thenegative,or "anaesthetic", symptoms of schizophrenia and in probable extension pronouncedschizoidia(including the characteristic deterioration in personal grooming/appearance).[26][27]It has also been weighed againstfluvoxaminein this overall regard (i.e., treating thenegative symptomsof schizophrenia),[28]withfluvoxamineevidencing clear superiority therein. Maprotiline, however, may be specifically useful for the "negative symptom" ofalogia(poverty of thought and/or speech) and in this regard was found demonstrably superior to the other control-drugs (alprazolam,bromocriptine,citalopram,fluoxetine,fluvoxamine,nortriptyline) in one study.[29]Citalopram,clomipramineandfluvoxamineappeared particularly useful in the study for reducingaffective blunting,withalprazolam(Xanax) and maprotiline ranking joint-next.
Patients withbipolar affective disordershould not receive antidepressants whilst in a manic phase (includinghypomania) under any circumstances whatsoever. (By the same analogy, people withschizoaffective disorder,bipolar type should not be taking maprotiline or other antidepressants while manic.) This is because antidepressants are known to come with the risk of worsening acute mania or precipitating it in so vulnerably-predisposed people.[30][31]
They (antidepressants) may also negatively interfere with the treatment of mixed bipolar states (pure orschizo-affective), whereelectro-convulsive therapy[32][33](generally bilateral),valproate[34]andantipsychoticsprove more beneficial (lithium should not be administered concurrently withE.C.T.treatment, as it may induce severe confusion[35]).[36]However, maprotiline (at a high dose) was put to good use in one particular case, of one young man presenting with what was very-possibly amixed-manic episodewith a heavy preponderance of depressive symptoms (appearing as depression with significantnarcissistictraits; includingextrapunitivetendencies/blame-shifting, entitlement and interpersonal exploitation; and provisionally considerednarcissistic depression).[37]The maprotiline was combined withmirtazapine(low-dose),sodium valproateandaripiprazole.
Absolute
[edit]- Hypersensitivity to maprotiline or to other TCAs and TeCAs
- Hypertrophyof theprostate glandwith urine hesitancy
- Closed angleglaucoma
Special caution needed
[edit]- Concomitant treatment with aMAO inhibitor
- Serious impairment of liver and kidney function
- Epilepsyand other conditions that lower the seizure threshold (activebrain tumors,alcohol withdrawal,other medications)
- Serious cardiovascular conditions (arrhythmias,heart insufficiency, state aftermyocardial infarctionetc.)
- Treatment of patients under age 18[38]
Suicidal patients
[edit]As with other antidepressants, maprotiline increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of maprotiline or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Maprotiline is not approved for use in pediatric patients.[39]
Pregnancy and lactation
[edit]Reproduction studies have been performed in female laboratory rabbits, mice, and rats at doses up to 1.3, 7, and 9 times the maximum daily human dose respectively and have revealed no evidence of impaired fertility or harm to the fetus due to maprotiline. There are, however, no adequate and well controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Maprotiline is excreted in breast milk. At steady-state, the concentrations in milk correspond closely to the concentrations in whole blood. Caution should be exercised when maprotiline hydrochloride is administered to a nursing woman.
Side effects
[edit]The side-effect profile is comparable to other TCAs and TeCAS and many of the following are due toanticholinergic(which are less prominent than those of most TCAs) andantihistamineeffects.[15]Most often seen are:
- Dizziness
- Drowsiness
- Somnolence
- Fatigue
- Dry mouth(and complications of long-term uncontrolled dry mouth such asdental caries)
- Constipation
- Vertigo
- Nausea(rare, incidence of ~2%) and vomiting
- Increased appetite and weight gain
- Orthostatic hypotension,hypertension,sinus tachycardia,heart-block,arrhythmiasand other cardiac effects
- Sexual dysfunctionin men:impotence,priapism,delayed ejaculation,anejaculation,decreased libido
- Sexual dysfunction in women: decreased libido,vaginal dryness,painful sexual intercourse,anorgasmia
- Allergic skin reactions such asrashorurticaria(more often than with other antidepressants). Rarely, severe skin reactions such aserythema multiformecan occur.
- Photosensitivity
- Agitation, confusion
- Induction ofhypomaniaormaniain patients with underlyingbipolar affective disorder
- Psychoticsymptoms
- Tremor
- Extrapyramidal symptoms
- Headache
- Seizures(at high doses)
- Rare haematological complications:leukopeniaandagranulocytosis(dangerous fall in white blood cells)
- Fever
- Urinary retention
Maprotiline causes a strong initial sedation (first 2 to 3 weeks of therapy) and is therefore indicated to treat agitated patients or those with suicidal risks. It causesanticholinergicside effects (dry mouth, constipation, urinary hesitancy, etc.) with much lower incidence thanamitriptyline.Originally, the manufacturer claimed that maprotiline is better tolerated than other TCAs and TeCAs. However, seizures, leukopenia and skin reactions occur more often with maprotiline than with comparable drugs (e.g., amitriptyline, protriptyline,mirtazapine). Indeed,seizuresare greater risk for concern with maprotiline than with all other tricyclic antidepressants[40](rising from 75 mg, becoming significant at daily doses ≥ 200 m.g.), includingclomipramine.It should thus be prescribed with particular, if not extreme, caution to people with a history ofepilepsy/seizures of any other kind. In any case, the total daily dose should be kept to ≤ 225 milligrams.
Maprotiline has no known potential for abuse and psychological dependence.
Withdrawal
[edit]Withdrawal symptoms frequently seen when treatment with maprotiline is stopped abruptly (agitation, anxiety, insomnia, sometimes activation of mania or rebound depression) can be avoided by reducing the daily dose of maprotiline gradually by approximately 25% each week. If treatment has to be stopped at once for medical reasons, the use of a benzodiazepine (e.g., lorazepam, clonazepam, diazepam) for a maximum of 4 weeks as needed will usually suppress withdrawal symptoms.
Interactions
[edit]Maprotiline does have a wide range of possible interactions. Some are typical for TCAs and TeCAs, others are caused by specific metabolic effects (e.g., high plasma-protein-binding) of maprotiline:
Increased drug actions:
- Other antidepressants, barbiturates, narcotics, sedating antihistamines, anticonvulsive drugs,alcohol– resulting in increased central depression and necessitating some caution when using any of these drugs alongside maprotiline
- Drugs with potential anti-muscarinic/anti-cholinergic activity (antiparkinsonian agents,atropine,amantadine,clozapineandtricyclic antidepressantsbesides maprotiline) – resulting in increased anti-muscarinic effects (dry mouth, constipation, etc.)
- Sympathomimetics (also those used in local anesthetics like noradrenaline) – sympathomimetic effects increased (increased blood-pressure, pulse-rate, paleness of skin, etc.)
- Nitrates and antihypertensives (e.g., beta-blockers) – increased antihypertensive action with pronounced fall in blood pressure
Although concurrent administration of tricyclic antidepressants (likewise withSSRIs) and MAOIs has been considered particularly dangerous, even fatal, across various medical and pharmaceutical lines across the decades, the premise for this line of thinking, although commonly accepted, may be erroneous. Specialist-research into this[41]and practical clinical experience involving the co-administration of tricyclics and MAOIs have suggested that it is only tricyclics with strong specific serotonin-reuptake inhibitory action (clomipramineand, to a lesser extent,imipramine) that are dangerous to give in combination with MAOIs. Other antidepressants; which may or may not have a significant serotoninergic background otherwise but either way lack in particularly appreciable reuptake-inhibition therein specifically (e.g.,mirtazapine,amitriptyline,trazodone,lofepramine,nortriptyline); may be safe to take alongside MAOIs, where the likes ofvenlafaxine,SSRIsandclomipramineare not. With maprotiline, this has been demonstrated to be the case withmoclobemide,[42]a drug it is often compared and considered somewhat analogous (along certain lines) to, and, tentatively,brofaromine[43](a research-agent MAOI which was never brought to full marketing development). Moclobemide specifically, however, may increase maprptiline plasma-levels[44]and may necessitate dose-modification(s).
In any case, however, it is very-strongly advised that an MAOI is added to the (compatible) tricyclic and not the other way around, as adding a tricyclic to an existing treatment-regime involving an MAOI may significantly increase the risk of going into hypertensive crisis.
Decreased drug actions:
- Guanethidine,reserpine,guanfacine:anti-hypertensive effects decreased
- Clonidine:anti-hypertensive effects decreased and risk of (massive) rebound hypertension.
Other types of interaction:
- Drugs which induce certain enzymes in the liver, e.g., barbiturates,phenytoin,carbamazepineand oral anti-conceptive drugs, enhance the elimination of maprotiline and decrease its antidepressant effects. Additionally the blood-concentrations of phenytoin or carbamazepine may be increased, leading to a higher incidents of side effects.
- The concomitant use of maprotiline andneurolepticscan lead to increased maprotiline blood-levels and to seizures. Combining maprotiline and thioridazine could induce severe arrhythmias.
- Additionally, increased blood-levels of maprotiline are possible, if certain beta-blocking agents (e.g.,propranolol) are given concomitantly.
- Maprotiline may amplify the actions ofcoumarin-type anticoagulants (e.g.,warfarin,phenprocoumon). The plasma-prothrombin-activity must be assessed closely in order to avoid overt bleedings.
- Maprotiline can increase the actions of oral antidiabetic drugs (sulfonylureas) andinsulin.Diabetic patients should have regular assessments of their blood-glucose-levels.
- The concomitant application with fluoxetine or fluvoxamine may lead to significantly increased plasma-levels of maprotiline, with a correspondingly (and substantially) incidence of maprotiline side effects. Owing to the long half-lives of fluoxetine and fluvoxamine, this effect may persist for quite-some time.
Pharmacology
[edit]Pharmacodynamics
[edit]| Site | Ki(nM) | Species | Ref | |
|---|---|---|---|---|
| SERT | 5,800 | Human | [46] | |
| NET | 11–12 | Human | [46][47] | |
| DAT | 1,000 | Human | [46] | |
| 5-HT2A | 51 | Rat | [48] | |
| 5-HT2C | 122 | Rat | [48] | |
| 5-HT6 | ND | ND | ND | |
| 5-HT7 | 50 | Guinea pig | [49] | |
| α1 | 90 | Human | [50] | |
| α2 | 9,400 | Human | [50] | |
| D1 | 402 | Human | [51] | |
| D2 | 350–665 | Human | [51][50] | |
| D3 | 504 | Human | [51] | |
| D4 | ND | ND | ND | |
| D5 | 429 | Human | [51] | |
| H1 | 0.79–2.0 | Human | [52][51][53][50] | |
| H2 | 776 | Human | [52] | |
| H3 | 66,100 | Human | [51] | |
| H4 | 85,100 | Human | [52] | |
| mACh | 570 | Human | [54][50] | |
| Values are Ki(nM). The smaller the value, the more strongly the drug binds to the site. | ||||
Maprotiline exhibits strong effects as anorepinephrine reuptake inhibitorwith only weak actions the reuptake ofserotoninanddopamine.[55][15]It is also a strongantagonistof theH1receptor,a moderate antagonist of the5-HT2andα1-adrenergic receptors,and a weak antagonist of theD2andmuscarinic acetylcholine receptors.Maprotiline has also more recently been identified as a potent antagonist of the5-HT7receptor,with this action potentially playing an important role in its antidepressant effectiveness.[56]The drug is a strongantihistamine,but unlike most TCAs, has minimalanticholinergiceffects.[57]
The pharmacological profile of maprotiline explains itsantidepressant,sedative,anxiolytic,andsympathomimeticactivities. In accordance to the pharmacological characteristics it is used in the treatment of depression, such as depression associated with agitation or anxiety. Additionally, it shows strong antagonism againstreserpine-induced effects in animal studies, as do the other 'classical' antidepressants. Although maprotiline behaves in most regards as a 'first-generation antidepressant' it is commonly referred to as 'second-generation antidepressant'.
The postulated mechanism of maprotiline is that it acts primarily by potentiation of central adrenergic synapses by blocking reuptake of norepinephrine at nerve endings. This pharmacological action is thought to be primarily responsible for the drug's antidepressant and anxiolytic effects. It is a strong norepinephrine reuptake inhibitor with only weak effects on serotonin and dopamine reuptake. At higher doses, however, maprotiline increases serotonergic transmission and increases the level of serotonin available.[58]
Pharmacokinetics
[edit]After oral use absorption is good. It binds to plasma proteins 80–90%. Maximal plasma concentration is reached 6 hours after use. The mean time to peak is 12 hours. Theterminal half-lifeof averages 51 hours.
Chemistry
[edit]

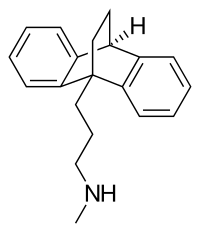
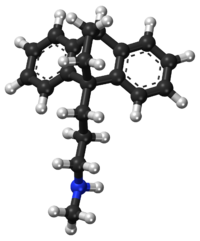
Maprotiline is atetracyclic compoundand is grouped with the TeCAs.[6][5]Itschemical nameisN-methyl-9,10-ethanoanthracen-9(10H)-propylamine.[59]The drug has a dibenzobicyclo[2.2.2]octadiene (9,10-dihydro-9,10-ethanoanthracene)ring system;that is, atricyclicanthracenering system with anethylenebridgeacross the centralring.[6][5]This results in it having a unique three-dimensional central ring (a bicyclo[2.2.2]octane or 1,4-endoethylenecyclohexane ring) and being a tetracyclic rather than a tricyclic compound.[6]However, it could also or alternatively be considered to be a tricyclic and hence a TCA.[5]In addition to itsheterocyclicring system, maprotiline has analkylamineside chainattached similarly to other TCAs (but notably unlike other TeCAs).[6][5]In terms of the side chain, it is asecondary amine,[5]and itschemical structure,aside from the ethylene link in the central ring, is similar to that of secondary amine TCAs likenortriptylineandprotriptyline.[6][59]In accordance, the pharmacology of maprotiline is very similar to that of secondary amine TCAs.[6][5]
Maprotiline is very similar in structure to theanxiolytic,sedative,andmuscle relaxantdrugbenzoctamine(Tacitin).[6][60]The only structural difference between the two compounds is in the length of their side chain.[6][60]However, this modification results in considerable differences in their pharmacological and therapeutic effects.[6][60]
History
[edit]Maprotiline was developed byCiba(now operated byNovartis).[61]It was patented in 1966 and was first described in the literature in 1969.[61]The drug was introduced for medical use in 1974.[61][62]Genericsare now widely available. It was introduced after most of the other TCAs but was the first TeCA to be developed and marketed, with the TeCAsmianserinandamoxapinefollowing shortly thereafter andmirtazapinebeing introduced later on.[61][62]
Society and culture
[edit]
Generic names
[edit]Maprotilineis theEnglishandFrenchgeneric nameof the drug and itsINN,USAN,BAN,andDCF,whilemaprotiline hydrochlorideis itsUSAN,USP,BANMandJAN.[1][2][63][3]Its generic name inSpanishandItalianand itsDCITaremaprotilina,inGermanismaprotilin,and inLatinismaprotilinum.[2][3]Themethanesulfonate(mesylate)saltis known unofficially asmaprotiline methanesulfonate.[2][3]
Brand names
[edit]Maprotiline is marketed throughout the world, mainly under the brand name Ludiomil.[2][3]It is also available under a variety of other brand names including Deprilept, Maprolu, and Psymion among others.[2][3]
Although it remains available across the world, it was discontinued in theUnited Kingdomin July 2006. Mylan, a key manufacturer of maprotiline in theUnited States,discontinued production in June 2021.[64]
References
[edit]- ^abElks J (14 November 2014).The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies.Springer. pp. 752–.ISBN978-1-4757-2085-3.
- ^abcdefIndex Nominum 2000: International Drug Directory.Taylor & Francis. 2000. pp. 630–.ISBN978-3-88763-075-1.
- ^abcdef"Maprotiline - Drugs.com".drugs.com.Retrieved28 March2018.
- ^Anvisa(2023-03-31)."RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial"[Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese).Diário Oficial da União(published 2023-04-04).Archivedfrom the original on 2023-08-03.Retrieved2023-08-16.
- ^abcdefghiWilliams DA (24 January 2012)."Antidepressants".In Lemke TL, Williams DA (eds.).Foye's Principles of Medicinal Chemistry.Lippincott Williams & Wilkins. pp. 591–.ISBN978-1-60913-345-0.
- ^abcdefghijZhou Y (22 October 2013)."New Generation of Antidepressants: Maprotiline".Drugs in Psychiatric Practice.Elsevier. pp. 222–.ISBN978-1-4831-9193-5.
- ^Guimarães FS, Zuardi AW, Graeff FG (January 1987). "Effect of chlorimipramine and maprotiline on experimental anxiety in humans".Journal of Psychopharmacology.1(3): 184–192.doi:10.1177/026988118700100305.PMID22158980.S2CID8444656.
- ^Vinader-Caerols C, Martos AJ, Monleón S, Arenas MC, Parra A (2006)."Acute effects of maprotiline on learning, anxiety, activity and analgesia in male and female mice".Acta Neurobiologiae Experimentalis.66(1): 23–31.doi:10.55782/ane-2006-1584.PMID16617674.
- ^Pecknold JC, Familamiri P, McClure DJ, Elie R, Chang H (May 1985). "Trimipramine and maprotiline: antidepressant, anxiolytic, and cardiotoxic comparison".The Journal of Clinical Psychiatry.46(5): 166–171.PMID2859273.
- ^Brownell LG, Perez-Padilla R, West P, Kryger MH (1983). "The role of protriptyline in obstructive sleep apnea".Bulletin Européen de Physiopathologie Respiratoire.19(6): 621–4.PMID6360257.
- ^Holmberg G (May 1988). "Sedative effects of maprotiline and amitriptyline".Acta Psychiatrica Scandinavica.77(5): 584–6.doi:10.1111/j.1600-0447.1988.tb05171.x.PMID3044007.S2CID41977086.
- ^Delini-Stula A, Mikkelsen H, Angst J (October 1995). "Therapeutic efficacy of antidepressants in agitated anxious depression--a meta-analysis of moclobemide studies".Journal of Affective Disorders.35(1–2): 21–30.doi:10.1016/0165-0327(95)00034-K.PMID8557884.
- ^Gachoud JP, Dick P, Köhler M (1994). "Comparison of the efficacy and tolerability of moclobemide and maprotiline in depressed patients treated by general practitioners".Clinical Neuropharmacology.17(Suppl 1): S29–37.doi:10.1097/00002826-199417001-00005.PMID7954482.S2CID260560762.
- ^Vrethem M, Boivie J, Arnqvist H, Holmgren H, Lindström T, Thorell LH (December 1997). "A comparison a amitriptyline and maprotiline in the treatment of painful polyneuropathy in diabetics and nondiabetics".The Clinical Journal of Pain.13(4): 313–23.doi:10.1097/00002508-199712000-00009.PMID9430812.
- ^abc"DRUGDEX Evaluations - Maprotiline".Retrieved25 April2013.
- ^Zhou, Z. and Liu, S., 2022. Maprotiline Ameliorates High Glucose-Induced Dysfunction in Renal Glomerular Endothelial Cells. Experimental and Clinical Endocrinology & Diabetes, 130(09), pp.596-603.
- ^Singh R, Kishore L, Kaur N (February 2014). "Diabetic peripheral neuropathy: current perspective and future directions".Pharmacological Research.80:21–35.doi:10.1016/j.phrs.2013.12.005.PMID24373831.S2CID6097534.
- ^Cloonan SM, Drozgowska A, Fayne D, Williams DC (March 2010). "The antidepressants maprotiline and fluoxetine have potent selective antiproliferative effects against Burkitt lymphoma independently of the norepinephrine and serotonin transporters".Leukemia & Lymphoma.51(3): 523–39.doi:10.3109/10428190903552112.PMID20141432.S2CID33104465.
- ^Cloonan SM, Williams DC (April 2011). "The antidepressants maprotiline and fluoxetine induce Type II autophagic cell death in drug-resistant Burkitt's lymphoma".International Journal of Cancer.128(7): 1712–23.doi:10.1002/ijc.25477.PMID20503272.S2CID24955263.
- ^Sufka KJ, White SW (November 2013). "Identification of a treatment-resistant, ketamine-sensitive genetic line in the chick anxiety-depression model".Pharmacology, Biochemistry, and Behavior.113:63–7.doi:10.1016/j.pbb.2013.10.013.PMID24157688.S2CID23648185.
- ^"Maprotiline: MedlinePlus Drug Information".www.nlm.nih.gov.Retrieved29 September2013.
- ^"Maprotiline - FDA prescribing information, side effects and uses".www.drugs.com.Archived fromthe originalon 30 December 2019.Retrieved29 September2013.
- ^Berger M, Gastpar M (1996). "Trimipramine: a challenge to current concepts on antidepressives".European Archives of Psychiatry and Clinical Neuroscience.246(5): 235–9.doi:10.1007/BF02190274.PMID8863001.S2CID29596291.
- ^Eikmeier G, Muszynski K, Berger M, Gastpar M (September 1990). "High-dose trimipramine in acute schizophrenia. Preliminary results of an open trial".Pharmacopsychiatry.23(5): 212–4.doi:10.1055/s-2007-1014510.PMID1979173.S2CID5719177.
- ^Eikmeier G, Berger M, Lodemann E, Muszynski K, Kaumeier S, Gastpar M (1991). "Trimipramine--an atypical neuroleptic?".International Clinical Psychopharmacology.6(3): 147–53.doi:10.1097/00004850-199100630-00003.PMID1806621.S2CID41564511.
- ^Yamagami S, Soejima K (1989). "Effect of maprotiline combined with conventional neuroleptics against negative symptoms of chronic schizophrenia".Drugs Under Experimental and Clinical Research.15(4): 171–6.PMID2570687.
- ^Waehrens J, Gerlach J (May 1980). "Antidepressant drugs in anergic schizophrenia. A double-blind cross-over study with maprotiline and placebo".Acta Psychiatrica Scandinavica.61(5): 438–44.doi:10.1111/j.1600-0447.1980.tb00882.x.PMID6105762.S2CID40809634.
- ^Silver H, Shmugliakov N (June 1998). "Augmentation with fluvoxamine but not maprotiline improves negative symptoms in treated schizophrenia: evidence for a specific serotonergic effect from a double-blind study".Journal of Clinical Psychopharmacology.18(3): 208–11.doi:10.1097/00004714-199806000-00005.PMID9617979.
- ^Shafti SS, Rey A, Abad A (2005)."Drug – Specific Responsiveness of Negative Symptoms".International Journal of Psychosocial Rehabilitation. pp. 10 (1), 43–51. Archived fromthe originalon 2012-07-12.Retrieved2012-04-29.
- ^Benazzi F, Mazzoli M, Rossi E (July 1992). "Severe mania after maprotiline-induced coma".Pharmacopsychiatry.25(4): 207.doi:10.1055/s-2007-1014407.PMID1528960.S2CID260253520.
- ^Wehr TA, Goodwin FK (November 1987). "Can antidepressants cause mania and worsen the course of affective illness?".The American Journal of Psychiatry.144(11): 1403–11.doi:10.1176/ajp.144.11.1403.PMID3314536.
- ^Perugi G, Medda P, Toni C, Mariani MG, Socci C, Mauri M (April 2017)."The Role of Electroconvulsive Therapy (ECT) in Bipolar Disorder: Effectiveness in 522 Patients with Bipolar Depression, Mixed-state, Mania and Catatonic Features".Current Neuropharmacology.15(3): 359–371.doi:10.2174/1570159X14666161017233642.PMC5405614.PMID28503107.
- ^Kuzman MR, Medved V, Velagic V, Goluza E, Bradas Z (June 2012). "The use of electroconvulsive therapy to treat schizoaffective disorder in a patient with pacemaker: a case report".Psychiatria Danubina.24(2): 211–4.PMID22706421.
- ^Azorin JM, Belzeaux R, Cermolacce M, Kaladjian A, Corréard N, Dassa D, Dubois M, Maurel M, Micoulaud Franchi JA, Pringuey D, Fakra E (December 2013). "[Recommendations for the treatment of mixed episodes in current guidelines]".L'Encephale(in French).39(Suppl 3): S185–7.doi:10.1016/S0013-7006(13)70120-9.PMID24359859.
- ^Patel RS, Bachu A, Youssef NA (2020)."Combination of lithium and electroconvulsive therapy (ECT) is associated with higher odds of delirium and cognitive problems in a large national sample across the United States".Brain Stimulation.13(1): 15–19.doi:10.1016/j.brs.2019.08.012.PMID31492631.S2CID201125145.
- ^Krüger S, Trevor Young L, Bräunig P (June 2005). "Pharmacotherapy of bipolar mixed states".Bipolar Disorders.7(3): 205–15.doi:10.1111/j.1399-5618.2005.00197.x.PMID15898959.
- ^Saito S, Kobayashi T, Kato S (2013). "[A case of major depressive disorder barely distinguishable from narcissistic personality disorder]".Seishin Shinkeigaku Zasshi = Psychiatria et Neurologia Japonica(in Japanese).115(4): 363–71.PMID23789317.
- ^Simeon J, Maguire J, Lawrence S (1981). Maprotiline effects in children with enuresis and behavioural disorders. Progress in Neuro-Psychopharmacology 5 ( 5–6), 495–8
- ^U.S. National Library of Medicine. Last Reviewed 1 Sept. 2010Medline Plus entry for Maprotiline
- ^Knudsen K, Heath A (February 1984)."Effects of self poisoning with maprotiline".British Medical Journal (Clinical Research Ed.).288(6417): 601–3.doi:10.1136/bmj.288.6417.601.PMC1444313.PMID6421394.
- ^Gillman K (October 2017).""Much ado about nothing": monoamine oxidase inhibitors, drug interactions, and dietary tyramine ".CNS Spectrums.22(5): 385–387.doi:10.1017/S1092852916000651.PMID28148312.S2CID206312818.
- ^Laux G, Beckmann H, Classen W, Becker T (1989). "Moclobemide and maprotiline in the treatment of inpatients with major depressive disorder".Journal of Neural Transmission. Supplementum.28:45–52.PMID2677241.
- ^Hoencamp E, Haffmans PM, Dijken WA, Hoogduin CA, Nolen WA, van Dyck R (March 1994). "Brofaromine versus lithium addition to maprotiline. A double-blind study in maprotiline refractory depressed outpatients".Journal of Affective Disorders.30(3): 219–27.doi:10.1016/0165-0327(94)90082-5.PMID8006248.
- ^König F, Wolfersdorf M, Löble M, Wössner S, Hauger B (July 1997). "Trimipramine and maprotiline plasma levels during combined treatment with moclobemide in therapy-resistant depression".Pharmacopsychiatry.30(4): 125–7.doi:10.1055/s-2007-979497.PMID9271778.S2CID35570626.
- ^Roth BL,Driscol J."PDSP KiDatabase ".Psychoactive Drug Screening Program (PDSP).University of North Carolina at Chapel Hill and the United States National Institute of Mental Health.Retrieved7 May2022.
- ^abcTatsumi M, Groshan K, Blakely RD, Richelson E (December 1997). "Pharmacological profile of antidepressants and related compounds at human monoamine transporters".European Journal of Pharmacology.340(2–3): 249–258.doi:10.1016/s0014-2999(97)01393-9.PMID9537821.
- ^Heffernan GD, Coghlan RD, Manas ES, McDevitt RE, Li Y, Mahaney PE, et al. (November 2009). "Dual acting norepinephrine reuptake inhibitors and 5-HT(2A) receptor antagonists: Identification, synthesis and activity of novel 4-aminoethyl-3-(phenylsulfonyl)-1H-indoles".Bioorganic & Medicinal Chemistry.17(22): 7802–7815.doi:10.1016/j.bmc.2009.09.023.PMID19836247.
- ^abPälvimäki EP, Roth BL, Majasuo H, Laakso A, Kuoppamäki M, Syvälahti E, Hietala J (August 1996). "Interactions of selective serotonin reuptake inhibitors with the serotonin 5-HT2c receptor".Psychopharmacology.126(3): 234–240.doi:10.1007/bf02246453.PMID8876023.S2CID24889381.
- ^Lucchelli A, Santagostino-Barbone MG, D'Agostino G, Masoero E, Tonini M (September 2000). "The interaction of antidepressant drugs with enteric 5-HT7 receptors".Naunyn-Schmiedeberg's Archives of Pharmacology.362(3): 284–289.doi:10.1007/s002100000295.PMID10997731.S2CID24189673.
- ^abcdeRichelson E, Nelson A (July 1984). "Antagonism by antidepressants of neurotransmitter receptors of normal human brain in vitro".The Journal of Pharmacology and Experimental Therapeutics.230(1): 94–102.PMID6086881.
- ^abcdefvon Coburg Y, Kottke T, Weizel L, Ligneau X, Stark H (January 2009). "Potential utility of histamine H3 receptor antagonist pharmacophore in antipsychotics".Bioorganic & Medicinal Chemistry Letters.19(2): 538–542.doi:10.1016/j.bmcl.2008.09.012.PMID19091563.
- ^abcAppl H, Holzammer T, Dove S, Haen E, Strasser A, Seifert R (February 2012). "Interactions of recombinant human histamine H₁R, H₂R, H₃R, and H₄R receptors with 34 antidepressants and antipsychotics".Naunyn-Schmiedeberg's Archives of Pharmacology.385(2): 145–170.doi:10.1007/s00210-011-0704-0.PMID22033803.S2CID14274150.
- ^Kanba S, Richelson E (June 1984). "Histamine H1 receptors in human brain labelled with [3H]doxepin".Brain Research.304(1): 1–7.doi:10.1016/0006-8993(84)90856-4.PMID6146381.S2CID45303586.
- ^El-Fakahany E, Richelson E (January 1983)."Antagonism by antidepressants of muscarinic acetylcholine receptors of human brain".British Journal of Pharmacology.78(1): 97–102.doi:10.1111/j.1476-5381.1983.tb17361.x.PMC2044798.PMID6297650.
- ^Peng WH, Lo KL, Lee YH, Hung TH, Lin YC (August 2007). "Berberine produces antidepressant-like effects in the forced swim test and in the tail suspension test in mice".Life Sciences.81(11): 933–938.doi:10.1016/j.lfs.2007.08.003.PMID17804020.
- ^Matthys A, Haegeman G, Van Craenenbroeck K, Vanhoenacker P (June 2011). "Role of the 5-HT7 receptor in the central nervous system: from current status to future perspectives".Molecular Neurobiology.43(3): 228–253.doi:10.1007/s12035-011-8175-3.PMID21424680.S2CID25515856.
- ^Nelson JC (2009)."Tricyclic and Tetracyclic Drugs".In Schatzberg AF, Nemeroff CB (eds.).The American Psychiatric Publishing Textbook of Psychopharmacology.American Psychiatric Pub. pp. 277–.doi:10.1176/appi.books.9781615371624.as09.ISBN978-1-58562-309-9.
- ^Miyake K, Fukuchi H, Kitaura T, Kimura M, Kimura Y, Nakahara T (December 1991). "Pharmacokinetics of maprotiline and its demethylated metabolite in serum and specific brain regions of rats after acute and chronic administration of maprotiline".Journal of Pharmaceutical Sciences.80(12): 1114–8.doi:10.1002/jps.2600801205.PMID1815068.
- ^abVardanyan R, Hruby V (10 March 2006)."Antidepressants".Synthesis of Essential Drugs.Elsevier. pp. 110–.ISBN978-0-08-046212-7.
- ^abcDawson AH (13 May 1980)."Polycyclic Aromatic Compounds".In Lednicer D, Mitscher LA (eds.).The Organic Chemistry of Drug Synthesis.John Wiley & Sons. pp. 220–.ISBN978-0-471-04392-8.
- ^abcdAndersen J, Kristensen AS, Bang-Andersen B, Strømgaard K (July 2009). "Recent advances in the understanding of the interaction of antidepressant drugs with serotonin and norepinephrine transporters".Chemical Communications(25): 3677–3692.doi:10.1039/b903035m.PMID19557250.
- ^abDart RC (2004)."Chapter 134: Cyclic Antidepressant Drugs".Medical Toxicology.Lippincott Williams & Wilkins. pp. 836–.ISBN978-0-7817-2845-4.
- ^Morton IK, Hall JM (31 October 1999).Concise Dictionary of Pharmacological Agents: Properties and Synonyms.Springer Science & Business Media. pp. 171–.ISBN978-0-7514-0499-9.
- ^Jensen L."Drug Shortage Detail: Maprotiline Tablets".www.ashp.org.American Society of Health-System Pharmacists.Retrieved22 October2023.
