Butyric acid
| |||

| |||
| Names | |||
|---|---|---|---|
| Preferred IUPAC name
Butanoic acid[1] | |||
| Other names | |||
| Identifiers | |||
3D model (JSmol)
|
| ||
| ChEBI |
| ||
| ChEMBL |
| ||
| ChemSpider | |||
| DrugBank |
| ||
| ECHA InfoCard | 100.003.212 | ||
| EC Number |
| ||
| |||
| KEGG |
| ||
| MeSH | Butyric+acid | ||
PubChemCID
|
|||
| RTECS number |
| ||
| UNII |
| ||
| UN number | 2820 | ||
CompTox Dashboard(EPA)
|
| ||
| |||
| |||
| Properties | |||
| C 3H 7COOH | |||
| Molar mass | 88.106g·mol−1 | ||
| Appearance | Colorless liquid | ||
| Odor | Unpleasant, similar to vomit or body odor | ||
| Density | 1.135 g/cm3(−43 °C)[2] 0.9528 g/cm3(25 °C)[3] | ||
| Melting point | −5.1 °C (22.8 °F; 268.0 K)[3] | ||
| Boiling point | 163.75 °C (326.75 °F; 436.90 K)[3] | ||
| Sublimes at −35 °C ΔsublH | |||
| Miscible | |||
| Solubility | Miscible withethanol,ether.Slightly soluble inCCl4 | ||
| logP | 0.79 | ||
| Vapor pressure | 0.112 kPa (20 °C) 0.74 kPa (50 °C) 9.62 kPa (100 °C)[4] | ||
| 5.35·10−4L·atm/mol | |||
| Acidity(pKa) | 4.82 | ||
| −55.10·10−6cm3/mol | |||
| Thermal conductivity | 1.46·105W/m·K | ||
Refractive index(nD)
|
1.398 (20 °C)[3] | ||
| Viscosity | 1.814 cP(15 °C)[5] 1.426 cP (25 °C) | ||
| Structure | |||
| Monoclinic(−43 °C)[2] | |||
| C2/m[2] | |||
a= 8.01 Å,b= 6.82 Å,c= 10.14 Å[2] α = 90°, β = 111.45°, γ = 90°
| |||
| 0.93 D (20 °C)[5] | |||
| Thermochemistry | |||
| 178.6 J/mol·K[4] | |||
Std molar
entropy(S⦵298) |
222.2 J/mol·K[5] | ||
Std enthalpy of
formation(ΔfH⦵298) |
−533.9 kJ/mol[4] | ||
Std enthalpy of
combustion(ΔcH⦵298) |
2183.5 kJ/mol[4] | ||
| Hazards | |||
| GHSlabelling: | |||
 [6] [6]
| |||
| Danger | |||
| H314[6] | |||
| P280,P305+P351+P338,P310[6] | |||
| NFPA 704(fire diamond) | |||
| Flash point | 71 to 72 °C (160 to 162 °F; 344 to 345 K)[6] | ||
| 440 °C (824 °F; 713 K)[6] | |||
| Explosive limits | 2.2–13.4% | ||
| Lethal doseor concentration (LD, LC): | |||
LD50(median dose)
|
2000 mg/kg (oral, rat) | ||
| Safety data sheet(SDS) | External MSDS | ||
| Related compounds | |||
Relatedcarboxylic acids
|
Propionic acid,Pentanoic acid | ||
Related compounds
|
1-Butanol Butyraldehyde Methyl butyrate | ||
Except where otherwise noted, data are given for materials in theirstandard state(at 25 °C [77 °F], 100 kPa).
| |||
Butyric acid(/ˈbjuːtɪrɪk/;fromAncient Greek:βούτῡρον,meaning "butter" ), also known under the systematic namebutanoic acid,is a straight-chainalkylcarboxylic acidwith thechemical formulaCH3CH2CH2CO2H.It is an oily, colorless liquid with anunpleasant odor.Isobutyric acid(2-methylpropanoic acid) is anisomer.Saltsandestersof butyric acid are known asbutyratesorbutanoates.The acid does not occur widely in nature, but its esters are widespread. It is a common industrial chemical[7]and an important component in the mammalian gut.
History
[edit]Butyric acid was first observed in an impure form in 1814 by the French chemistMichel Eugène Chevreul.By 1818, he had purified it sufficiently to characterize it. However, Chevreul did not publish his early research on butyric acid; instead, he deposited his findings in manuscript form with the secretary of theAcademy of Sciencesin Paris, France.Henri Braconnot,a French chemist, was also researching the composition of butter and was publishing his findings and this led to disputes about priority. As early as 1815, Chevreul claimed that he had found the substance responsible for the smell of butter.[8]By 1817, he published some of his findings regarding the properties of butyric acid and named it.[9]However, it was not until 1823 that he presented the properties of butyric acid in detail.[10]The name butyric acid comes fromβούτῡρον,meaning "butter", the substance in which it was first found. The Latin namebutyrum(orbuturum) is similar.
Occurrence
[edit]Triglyceridesof butyric acid compose 3–4% ofbutter.When butter goes rancid, butyric acid is liberated from the glyceride byhydrolysis.[11]It is one of the fatty acid subgroup calledshort-chain fatty acids.Butyric acid is a typicalcarboxylic acidthat reacts with bases and affects many metals.[12] It is found inanimal fatandplant oils,bovinemilk,breast milk,butter,parmesan cheese,body odor,vomitand as a product of anaerobicfermentation(including in thecolon).[13][14]It has atastesomewhat like butter and an unpleasantodor.Mammalswith good scent detection abilities, such asdogs,can detect it at 10parts per billion,whereashumanscan detect it only in concentrations above 10parts per million.Infood manufacturing,it is used as aflavoring agent.[15]
In humans, butyric acid is one of two primaryendogenous agonistsof humanhydroxycarboxylic acid receptor 2(HCA2), aGi/o-coupledG protein-coupled receptor.[16][17]
Butyric acid is present as itsoctyl esterinparsnip(Pastinaca sativa)[18]and in the seed of theginkgo tree.[19]
Production
[edit]Industrial
[edit]In industry, butyric acid is produced byhydroformylationfrompropeneandsyngas,formingbutyraldehyde,which isoxidisedto the final product.[7]
- H2+ CO + CH3CH=CH2→ CH3CH2CH2CHObutyric acid
It can be separated from aqueous solutions by saturation with salts such ascalcium chloride.The calcium salt,Ca(C4H7O2)2·H2O,is less soluble in hot water than in cold.
Microbial biosynthesis
[edit]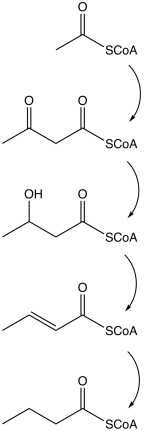
Butyrate is produced by several fermentation processes performed byobligateanaerobicbacteria.[20]This fermentation pathway was discovered byLouis Pasteurin 1861. Examples of butyrate-producingspeciesof bacteria:
- Clostridium butyricum
- Clostridium kluyveri
- Clostridium pasteurianum
- Faecalibacterium prausnitzii
- Fusobacterium nucleatum
- Butyrivibrio fibrisolvens
- Eubacterium limosum
The pathway starts with theglycolyticcleavage ofglucoseto twomoleculesofpyruvate,as happens in most organisms. Pyruvate isoxidizedintoacetyl coenzyme Acatalyzed bypyruvate:ferredoxin oxidoreductase.Two molecules ofcarbon dioxide(CO2) and two molecules ofhydrogen(H2) are formed as waste products. Subsequently,ATPis produced in the last step of the fermentation. Three molecules of ATP are produced for each glucose molecule, a relatively high yield. The balanced equation for this fermentation is
- C6H12O6→ C4H8O2+ 2CO2+ 2H2
Other pathways to butyrate includesuccinatereduction and crotonate disproportionation.
| Action | Responsible enzyme |
|---|---|
| Acetyl coenzyme A converts intoacetoacetyl coenzyme A | acetyl-CoA-acetyl transferase |
| Acetoacetyl coenzyme A converts intoβ-hydroxybutyryl CoA | β-hydroxybutyryl-CoA dehydrogenase |
| β-hydroxybutyryl CoA converts intocrotonyl CoA | crotonase |
| Crotonyl CoA converts intobutyryl CoA(CH3CH2CH2C=O−CoA) | butyryl CoA dehydrogenase |
| Aphosphategroup replaces CoA to formbutyryl phosphate | phosphobutyrylase |
| The phosphate group joinsADPto formATPandbutyrate | butyrate kinase |
Several species formacetoneandn-butanolin an alternative pathway, which starts as butyrate fermentation. Some of these species are:
- Clostridium acetobutylicum,the most prominent acetone and butanol producer, used also in industry
- Clostridium beijerinckii
- Clostridium tetanomorphum
- Clostridium aurantibutyricum
These bacteria begin with butyrate fermentation, as described above, but, when thepHdrops below 5, they switch into butanol and acetone production to prevent further lowering of the pH. Two molecules of butanol are formed for each molecule of acetone.
The change in the pathway occurs after acetoacetyl CoA formation. This intermediate then takes two possible pathways:
- acetoacetyl CoA → acetoacetate → acetone
- acetoacetyl CoA → butyryl CoA → butyraldehyde → butanol
For commercial purposes Clostridium species are used preferably for butyric acid or butanol production. The most common species used for probiotics is theClostridium butyricum.[21]
Fermentable fiber sources
[edit]Highly-fermentable fiber residues, such as those fromresistant starch,oat bran,pectin,andguarare transformed bycolonic bacteriaintoshort-chain fatty acids(SCFA) including butyrate, producing more SCFA than less fermentable fibers such ascelluloses.[14][22]One study found that resistant starch consistently produces more butyrate than other types ofdietary fiber.[23]The production of SCFA from fibers inruminantanimals such as cattle is responsible for the butyrate content of milk and butter.[13][24]
Fructans are another source of prebiotic soluble dietary fibers which can be digested to produce butyrate.[25]They are often found in the soluble fibers of foods which are high insulfur,such as thealliumandcruciferous vegetables.Sources of fructansincludewheat(although some wheat strains such asspeltcontain lower amounts),[26]rye,barley,onion,garlic,Jerusalemandglobe artichoke,asparagus,beetroot,chicory,dandelion leaves,leek,radicchio,the white part ofspring onion,broccoli,brussels sprouts,cabbage,fennel,andprebiotics,such as fructooligosaccharides (FOS),oligofructose,andinulin.[27][28]
Reactions
[edit]Butyric acid reacts as a typical carboxylic acid: it can formamide,ester,anhydride,andchloridederivatives.[29]The latter,butyryl chloride,is commonly used as the intermediate to obtain the others.
Uses
[edit]Butyric acid is used in the preparation of various butyrate esters. It is used to producecellulose acetate butyrate(CAB), which is used in a wide variety of tools, paints, and coatings, and is more resistant to degradation thancellulose acetate.[30]CAB can degrade with exposure to heat and moisture, releasing butyric acid.[31]
Low-molecular-weight esters of butyric acid, such asmethyl butyrate,have mostly pleasant aromas or tastes.[7]As a consequence, they are used as food and perfume additives. It is an approved food flavoring in the EUFLAVIS database(number 08.005).
Due to its powerful odor, it has also been used as a fishing bait additive.[32]Many of the commercially available flavors used incarp(Cyprinus carpio) baits use butyric acid as their ester base. It is not clear whether fish are attracted by the butyric acid itself or the substances added to it. Butyric acid was one of the few organic acids shown to be palatable for bothtenchandbitterling.[33]The substance has been used as astink bombby theSea Shepherd Conservation Societyto disrupt Japanesewhalingcrews.[34]
Pharmacology
[edit]| Inhibited enzyme | IC50(nM) | Entry note |
|---|---|---|
| HDAC1 | 16,000 | |
| HDAC2 | 12,000 | |
| HDAC3 | 9,000 | |
| HDAC4 | 2,000,000 | Lower bound |
| HDAC5 | 2,000,000 | Lower bound |
| HDAC6 | 2,000,000 | Lower bound |
| HDAC7 | 2,000,000 | Lower bound |
| HDAC8 | 15,000 | |
| HDAC9 | 2,000,000 | Lower bound |
| CA1 | 511,000 | |
| CA2 | 1,032,000 | |
| GPCRtarget | pEC50 | Entry note |
| FFAR2 | 2.9–4.6 | Full agonist |
| FFAR3 | 3.8–4.9 | Full agonist |
| HCA2 | 2.8 | Agonist |
Pharmacodynamics
[edit]Butyric acid (pKa4.82) is fullyionizedatphysiological pH,so itsanionis the material that is mainly relevant in biological systems. It is one of two primaryendogenous agonistsof humanhydroxycarboxylic acid receptor 2(HCA2,also known as GPR109A), aGi/o-coupledG protein-coupled receptor(GPCR),[16][17]
Like othershort-chain fatty acids(SCFAs), butyrate is an agonist at thefree fatty acid receptorsFFAR2andFFAR3,which function as nutrient sensors that facilitate thehomeostatic control of energy balance;however, among the group of SCFAs, only butyrate is an agonist ofHCA2.[37][38][39]It is also anHDAC inhibitor(specifically, HDAC1, HDAC2, HDAC3, and HDAC8),[35][36]a drug that inhibits the function ofhistone deacetylaseenzymes, thereby favoring an acetylated state ofhistonesin cells.[39]Histone acetylation loosens the structure ofchromatinby reducing theelectrostaticattraction between histones andDNA.[39]In general, it is thought thattranscription factorswill be unable to access regions where histones are tightly associated with DNA (i.e., non-acetylated, e.g., heterochromatin).[medical citation needed]Therefore, butyric acid is thought to enhance the transcriptional activity at promoters,[39]which are typically silenced or downregulated due to histone deacetylase activity.
Pharmacokinetics
[edit]Butyrate that is produced in the colon through microbial fermentation of dietary fiber is primarily absorbed and metabolized bycolonocytesand the liver[note 1]for the generation of ATP during energy metabolism; however, some butyrate is absorbed in the distal colon, which is not connected to the portal vein, thereby allowing for thesystemic distributionof butyrate to multiple organ systems through the circulatory system.[39][40]Butyrate that has reached systemic circulation can readily cross theblood–brain barrierviamonocarboxylate transporters(i.e., certain members of theSLC16A group of transporters).[41][42]Other transporters that mediate the passage of butyrate across lipid membranes includeSLC5A8(SMCT1),SLC27A1(FATP1), andSLC27A4(FATP4).[35][42]
Metabolism
[edit]Butyric acid is metabolized by various humanXM-ligases(ACSM1, ACSM2B, ASCM3, ACSM4, ACSM5, and ACSM6), also known as butyrate–CoA ligase.[43][44]The metabolite produced by this reaction isbutyryl–CoA,and is produced as follows:[43]
- Adenosine triphosphate + butyric acid + coenzyme A → adenosine monophosphate + pyrophosphate + butyryl-CoA
As ashort-chain fatty acid,butyrate is metabolized bymitochondriaas an energy (i.e.,adenosine triphosphateor ATP) source throughfatty acid metabolism.[39]In particular, it is an important energy source for cells lining the mammaliancolon(colonocytes).[25]Without butyrates, colon cells undergoautophagy(i.e., self-digestion) and die.[45]
In humans, the butyrate precursortributyrin,which is naturally present in butter, is metabolized bytriacylglycerol lipaseintodibutyrinand butyrate through the reaction:[46]
- Tributyrin +H2O →dibutyrin + butyric acid
Biochemistry
[edit]Butyrate has numerous effects onenergy homeostasisand related diseases (diabetesandobesity),inflammation,andimmune function(e.g., it has pronouncedantimicrobialandanticarcinogeniceffects) in humans. These effects occur through its metabolism by mitochondria to generateATPduringfatty acid metabolismor through one or more of itshistone-modifying enzymetargets (i.e., theclass I histone deacetylases) andG-protein coupled receptortargets (i.e.,FFAR2,FFAR3,andHCA2).[37][47]
In the mammalian gut
[edit]Butyrate is essential to host immune homeostasis.[37]Although the role and importance of butyrate in the gut is not fully understood, many researchers argue that a depletion of butyrate-producing bacteria in patients with several vasculitic conditions is essential to the pathogenesis of these disorders. A depletion of butyrate in the gut is typically caused by an absence or depletion of butyrate-producing-bacteria (BPB). This depletion in BPB leads to microbialdysbiosis.This is characterized by an overall low biodiversity and a depletion of key butyrate-producing members. Butyrate is an essential microbial metabolite with a vital role as a modulator of proper immune function in the host. It has been shown that children lacking in BPB are more susceptible to allergic disease[48]and Type 1 Diabetes.[49]Butyrate is also reduced in a diet low indietary fiber,which can induce inflammation and have other adverse affects insofar as theseshort-chain fatty acidsactivatePPAR-γ.[50]
Butyrate exerts a key role for the maintenance of immune homeostasis both locally (in the gut) and systemically (via circulating butyrate). It has been shown to promote the differentiation ofregulatory T cells.In particular, circulating butyrate prompts the generation of extrathymic regulatory T cells. The low-levels of butyrate in human subjects could favor reduced regulatory T cell-mediated control, thus promoting a powerful immuno-pathological T-cell response.[51]On the other hand, gut butyrate has been reported to inhibit local pro-inflammatory cytokines. The absence or depletion of these BPB in the gut could therefore be a possible aide in the overly-active inflammatory response. Butyrate in the gut also protects the integrity of the intestinal epithelial barrier. Decreased butyrate levels therefore lead to a damaged or dysfunctional intestinal epithelial barrier.[52]Butyrate reduction has also been associated withClostridioides difficileproliferation. Conversely, a high-fiber diet results in higher butyric acid concentration and inhibition ofC. difficilegrowth.[53]
In a 2013 research study conducted by Furusawa et al., microbe-derived butyrate was found to be essential in inducing the differentiation of colonic regulatory T cells in mice. This is of great importance and possibly relevant to the pathogenesis and vasculitis associated with many inflammatory diseases because regulatory T cells have a central role in the suppression of inflammatory and allergic responses.[54]In several research studies, it has been demonstrated that butyrate induced the differentiation of regulatory T cells in vitro and in vivo.[55]The anti-inflammatory capacity of butyrate has been extensively analyzed and supported by many studies. It has been found that microorganism-produced butyrate expedites the production of regulatory T cells, although the specific mechanism by which it does so unclear.[56]More recently, it has been shown that butyrate plays an essential and direct role in modulating gene expression of cytotoxic T-cells.[57]Butyrate also has an anti-inflammatory effect on neutrophils, reducing their migration to wounds. This effect is mediated via the receptorHCA1[58]
In the gut microbiomes found in the class Mammalia, omnivores and herbivores have butyrate-producing bacterial communities dominated by the butyryl-CoA:acetate CoA-transferase pathway, whereas carnivores have butyrate-producing bacterial communities dominated by the butyrate kinase pathway.[59]
The odor of butyric acid, which emanates from the sebaceous follicles of all mammals, works on the tick as a signal.
Immunomodulation and inflammation
[edit]Butyrate's effects on the immune system are mediated through the inhibition of class Ihistone deacetylasesand activation of itsG-protein coupled receptortargets:HCA2(GPR109A),FFAR2(GPR43), andFFAR3(GPR41).[38][60]Among theshort-chain fatty acids,butyrate is the most potent promoter of intestinal regulatory T cellsin vitroand the only one among the group that is anHCA2ligand.[38]It has been shown to be a critical mediator of the colonic inflammatory response. It possesses both preventive and therapeutic potential to counteract inflammation-mediatedulcerative colitisandcolorectal cancer.
Butyrate has established antimicrobial properties in humans that are mediated through theantimicrobial peptideLL-37,which it induces viaHDACinhibition on histone H3.[60][61][62]In vitro, butyrate increasesgene expressionofFOXP3(thetranscription regulatorforTregs) and promotes colonicregulatory T cells(Tregs) through the inhibition of class Ihistone deacetylases;[38][60]through these actions, it increases the expression ofinterleukin 10,an anti-inflammatorycytokine.[60][38]Butyrate also suppresses colonic inflammation by inhibiting theIFN-γ–STAT1signaling pathways, which is mediated partially throughhistone deacetylase inhibition.While transient IFN-γ signaling is generally associated with normal hostimmune response,chronic IFN-γ signaling is often associated with chronic inflammation. It has been shown that butyrate inhibits activity of HDAC1 that is bound to the Fas gene promoter in T cells, resulting in hyperacetylation of the Fas promoter and up-regulation ofFas receptoron the T-cell surface.[63]
Similar to otherHCA2agonists studied, butyrate also produces marked anti-inflammatory effects in a variety of tissues, including the brain, gastrointestinal tract, skin, andvascular tissue.[64][65][66]Butyrate binding at FFAR3 inducesneuropeptide Yrelease and promotes the functionalhomeostasisof colonic mucosa and the enteric immune system.[67]
Cancer
[edit]Butyrate has been shown to be a critical mediator of the colonic inflammatory response. It is responsible for about 70% of energy from the colonocytes, being a critical SCFA in colonhomeostasis.[68]Butyrate possesses both preventive and therapeutic potential to counteract inflammation-mediatedulcerative colitis(UC) andcolorectal cancer.[69]It produces different effects in healthy and cancerous cells: this is known as the "butyrate paradox". In particular, butyrate inhibits colonic tumor cells and stimulates proliferation of healthy colonic epithelial cells.[70][71]The explanation why butyrate is an energy source for normal colonocytes and inducesapoptosisincolon cancercells, is theWarburg effectin cancer cells, which leads to butyrate not being properly metabolized. This phenomenon leads to the accumulation of butyrate in the nucleus, acting as ahistone deacetylase(HDAC) inhibitor.[72]One mechanism underlying butyrate function in suppression of colonic inflammation is inhibition of theIFN-γ/STAT1signalling pathways. It has been shown that butyrate inhibits activity ofHDAC1that is bound to theFas genepromoter inT cells,resulting in hyperacetylation of the Fas promoter and upregulation of Fas receptor on the T cell surface. It is thus suggested that butyrate enhancesapoptosisof T cells in the colonic tissue and thereby eliminates the source of inflammation (IFN-γ production).[73]Butyrate inhibitsangiogenesisby inactivatingSp1 transcription factoractivity and downregulatingvascular endothelial growth factorgene expression.[74]
In summary, the production ofvolatile fatty acidssuch as butyrate from fermentable fibers may contribute to the role of dietary fiber in colon cancer.Short-chain fatty acids,which include butyric acid, are produced by beneficialcolonic bacteria(probiotics) that feed on, or ferment prebiotics, which are plant products that contain dietary fiber. These short-chain fatty acids benefit the colonocytes by increasing energy production, and may protect against colon cancer by inhibiting cell proliferation.[22]
Conversely, some researchers have sought to eliminate butyrate and consider it a potential cancer driver.[75]Studies in mice indicate it drives transformation ofMSH2-deficientcolon epithelial cells.[76]
Potential treatments from butyrate restoration
[edit]Owing to the importance of butyrate as an inflammatory regulator and immune system contributor, butyrate depletions could be a key factor influencing the pathogenesis of manyvasculiticconditions. It is thus essential to maintain healthy levels of butyrate in the gut.Fecal microbiota transplants(to restore BPB andsymbiosisin the gut) could be effective by replenishing butyrate levels. In this treatment, a healthy individual donates their stool to be transplanted into an individual with dysbiosis. A less-invasive treatment option is the administration of butyrate—as oral supplements or enemas—which has been shown to be very effective in terminating symptoms of inflammation with minimal-to-no side-effects. In a study where patients with ulcerative colitis were treated with butyrate enemas, inflammation decreased significantly, and bleeding ceased completely after butyrate provision.[77]
Addiction
[edit]Butyric acid is anHDACinhibitor that is selective for class I HDACs in humans.[35]HDACs arehistone-modifying enzymesthat can cause histone deacetylation and repression of gene expression. HDACs are important regulators of synaptic formation,synaptic plasticity,andlong-term memoryformation. Class I HDACs are known to be involved in mediating the development of anaddiction.[78][79][80]Butyric acid and other HDAC inhibitors have been used in preclinical research to assess the transcriptional, neural, and behavioral effects of HDAC inhibition in animals addicted to drugs.[80][81][82]
Butyrate salts and esters
[edit]Thebutyrateorbutanoateion,C3H7COO−,is theconjugate baseof butyric acid. It is the form found in biological systems atphysiological pH.A butyric (or butanoic) compound is acarboxylate saltoresterof butyric acid.
Examples
[edit]Salts
[edit]Esters
[edit]- Butyl butyrate
- Butyryl-CoA
- Cellulose acetate butyrate(aircraft dope)
- Estradiol benzoate butyrate
- Ethyl butyrate
- Methyl butyrate
- Pentyl butyrate
- Tributyrin
See also
[edit]- List of saturated fatty acids
- Hershey's milk chocolate
- Histone
- Hydroxybutyric acids
- Oxobutyric acids
- 2-Oxobutyric acid(α-ketobutyric acid)
- 3-Oxobutyric acid(acetoacetic acid)
- 4-Oxobutyric acid(succinic semialdehyde)
- β-Methylbutyric acid
Notes
[edit]- ^Most of the butyrate that is absorbed intoblood plasmafrom the colon enters the circulatory system via theportal vein;most of the butyrate that enters the circulatory system by this route is taken up by the liver.[39]
References
[edit]This article incorporates text from a publication now in thepublic domain:Chisholm, Hugh,ed. (1911). "Butyric Acid".Encyclopædia Britannica(11th ed.). Cambridge University Press.
- ^"Applications to Specific Classes of Compounds".Nomenclature of Organic Chemistry: IUPAC Recommendations and Preferred Names 2013 (Blue Book).Cambridge:The Royal Society of Chemistry.2014. p. 746.doi:10.1039/9781849733069-00648.ISBN978-0-85404-182-4.
- ^abcdStrieter FJ, Templeton DH (1962)."Crystal structure of butyric acid"(PDF).Acta Crystallographica.15(12): 1240–1244.Bibcode:1962AcCry..15.1240S.doi:10.1107/S0365110X6200328X.
- ^abcdLide, David R., ed. (2009).CRC Handbook of Chemistry and Physics(90th ed.).Boca Raton, Florida:CRC Press.ISBN978-1-4200-9084-0.
- ^abcdeButanoic acidin Linstrom, Peter J.; Mallard, William G. (eds.);NIST Chemistry WebBook,NIST Standard Reference Database Number 69,National Institute of Standards and Technology, Gaithersburg (MD) (retrieved 27 October 2020)
- ^abc"Butanoic acid".Chemister.ru. 19 March 2007.Retrieved27 October2020.
- ^abcdeSigma-Aldrich Co.,Butyric acid.Retrieved on 27 October 2020.
- ^abcRiemenschneider, Wilhelm (2002). "Carboxylic Acids, Aliphatic".Ullmann's Encyclopedia of Industrial Chemistry.Weinheim: Wiley-VCH.doi:10.1002/14356007.a05_235.ISBN978-3527306732.
- ^Chevreul (1815)"Lettre de M. Chevreul à MM. les rédacteurs des Annales de chimie"(Letter from Mr. Chevreul to the editors of the Annals of Chemistry),Annales de chimie,94:73–79; in a footnote spanning pages 75–76, he mentions that he had found a substance that is responsible for the smell of butter.
- ^Chevreul (1817)"Extrait d'une lettre de M. Chevreul à MM. les Rédacteurs du Journal de Pharmacie"(Extract of a letter from Mr. Chevreul to the editors of the Journal of Pharmacy),Journal de Pharmacie et des sciences accessoires,3:79–81. On p. 81, he named butyric acid:"Ce principe, que j'ai appelé depuis acid butérique,…"(This principle [i.e., constituent], which I have since named "butyric acid",… )
- ^E. Chevreul,Recherches chimiques sur les corps gras d'origine animale[Chemical researches on fatty substances of animal origin] (Paris, France: F.G. Levrault, 1823),pages 115–133.
- ^Woo, A.H.; Lindsay, R.C. (1983)."Stepwise Discriminant Analysis of Free Fatty Acid Profiles for Identifying Sources of Lipolytic Enzymes in Rancid Butter".Journal of Dairy Science.66(10): 2070–2075.doi:10.3168/jds.S0022-0302(83)82052-9.
- ^ICSC 1334 – Butyric acid.Inchem.org (23 November 1998). Retrieved on 2020-10-27.
- ^abMcNabney, S. M.; Henagan, T. M. (2017)."Short Chain Fatty Acids in the Colon and Peripheral Tissues: A Focus on Butyrate, Colon Cancer, Obesity and Insulin Resistance".Nutrients.9(12): 1348.doi:10.3390/nu9121348.PMC5748798.PMID29231905.
- ^abMorrison, D. J.; Preston, T. (2016)."Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism".Gut Microbes.7(3): 189–200.doi:10.1080/19490976.2015.1134082.PMC4939913.PMID26963409.
- ^"Butyric acid".The Good Scents Company.Retrieved26 October2020.
- ^abOffermanns S, Colletti SL, Lovenberg TW, Semple G, Wise A, IJzerman AP (June 2011)."International Union of Basic and Clinical Pharmacology. LXXXII: Nomenclature and Classification of Hydroxy-carboxylic Acid Receptors (GPR81, GPR109A, and GPR109B)".Pharmacological Reviews.63(2): 269–90.doi:10.1124/pr.110.003301.PMID21454438.
- ^abOffermanns S, Colletti SL, IJzerman AP, Lovenberg TW, Semple G, Wise A, Waters MG."Hydroxycarboxylic acid receptors".IUPHAR/BPS Guide to Pharmacology.International Union of Basic and Clinical Pharmacology.Retrieved13 July2018.
- ^Carroll, Mark J.; Berenbaum, May R. (2002). "Behavioral responses of the parsnip webworm to host plant volatiles".Journal of Chemical Ecology.28(11): 2191–2201.doi:10.1023/A:1021093114663.PMID12523562.S2CID23512190.
- ^Raven, Peter H.;Evert, Ray F.; Eichhorn, Susan E. (2005).Biology of Plants.W. H. Freemanand Company. pp.429–431.ISBN978-0-7167-1007-3.Retrieved11 October2018.
- ^Seedorf, H.; Fricke, W. F.; Veith, B.; Bruggemann, H.; Liesegang, H.; Strittmatter, A.; Miethke, M.; Buckel, W.; Hinderberger, J.; Li, F.; Hagemeier, C.; Thauer, R. K.; Gottschalk, G. (2008)."The Genome ofClostridium kluyveri,a Strict Anaerobe with Unique Metabolic Features ".Proceedings of the National Academy of Sciences.105(6): 2128–2133.Bibcode:2008PNAS..105.2128S.doi:10.1073/pnas.0711093105.PMC2542871.PMID18218779.
- ^Zigová, Jana; Šturdı́k, Ernest; Vandák, Dušan; Schlosser, Štefan (October 1999)."Butyric acid production by Clostridium butyricum with integrated extraction and pertraction".Process Biochemistry.34(8): 835–843.doi:10.1016/S0032-9592(99)00007-2.
- ^abLupton JR (February 2004)."Microbial degradation products influence colon cancer risk: the butyrate controversy".The Journal of Nutrition.134(2): 479–82.doi:10.1093/jn/134.2.479.PMID14747692.
- ^Cummings JH, Macfarlane GT, Englyst HN (February 2001)."Prebiotic digestion and fermentation".The American Journal of Clinical Nutrition.73(2 Suppl): 415S–420S.doi:10.1093/ajcn/73.2.415s.PMID11157351.
- ^Grummer RR (September 1991)."Effect of feed on the composition of milk fat".Journal of Dairy Science.74(9): 3244–57.doi:10.3168/jds.S0022-0302(91)78510-X.PMID1779073.
- ^abRivière, Audrey; Selak, Marija; Lantin, David; Leroy, Frédéric; De Vuyst, Luc (2016)."Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut".Frontiers in Microbiology.7:979.doi:10.3389/fmicb.2016.00979.PMC4923077.PMID27446020.
- ^"Frequently asked questions in the area of diet and IBS".Department of Gastroenterology Translational Nutrition Science, Monash University, Victoria, Australia.Retrieved24 March2016.
- ^Gibson, Peter R.; Shepherd, Susan J. (1 February 2010)."Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach".Journal of Gastroenterology and Hepatology.25(2): 252–258.doi:10.1111/j.1440-1746.2009.06149.x.ISSN1440-1746.PMID20136989.S2CID20666740.
- ^Gibson, Peter R.; Varney, Jane; Malakar, Sreepurna; Muir, Jane G. (1 May 2015)."Food components and irritable bowel syndrome".Gastroenterology.148(6): 1158–1174.e4.doi:10.1053/j.gastro.2015.02.005.ISSN1528-0012.PMID25680668.
- ^Jenkins, P. R. (1985). "Carboxylic acids and derivatives".General and Synthetic Methods.Vol. 7. pp. 96–160.doi:10.1039/9781847556196-00096.ISBN978-0-85186-884-4.
- ^Lokensgard, Erik (2015).Industrial Plastics: Theory and Applications(6th ed.). Cengage Learning.
- ^Williams, R. Scott."Care of Plastics: Malignant plastics".WAAC Newsletter.Vol. 24, no. 1. Conservation OnLine.Retrieved29 May2017.
- ^Freezer BaitsArchived25 January 2010 at theWayback Machine,nutrabaits.net
- ^Kasumyan A, Døving K (2003). "Taste preferences in fishes".Fish and Fisheries.4(4): 289–347.Bibcode:2003AqFF....4..289K.doi:10.1046/j.1467-2979.2003.00121.x.
- ^Japanese Whalers Injured by Acid-Firing ActivistsArchived8 June 2010 at theWayback Machine,newser.com, 10 February 2010
- ^abcd"Butyric acid".IUPHAR/BPS Guide to Pharmacology.International Union of Basic and Clinical Pharmacology.Retrieved13 July2018.
- ^ab"Butanoic acid and Sodium butyrate".BindingDB.The Binding Database.Retrieved27 October2020.
- ^abcKasubuchi M, Hasegawa S, Hiramatsu T, Ichimura A, Kimura I (2015)."Dietary gut microbial metabolites, short-chain fatty acids, and host metabolic regulation".Nutrients.7(4): 2839–49.doi:10.3390/nu7042839.PMC4425176.PMID25875123.
Short-chain fatty acids (SCFAs) such as acetate, butyrate, and propionate, which are produced by gut microbial fermentation of dietary fiber, are recognized as essential host energy sources and act as signal transduction molecules via G-protein coupled receptors (FFAR2, FFAR3, OLFR78, GPR109A) and as epigenetic regulators of gene expression by the inhibition of histone deacetylase (HDAC). Recent evidence suggests that dietary fiber and the gut microbial-derived SCFAs exert multiple beneficial effects on the host energy metabolism not only by improving the intestinal environment, but also by directly affecting various host peripheral tissues.
- ^abcdeHoeppli RE, Wu D, Cook L, Levings MK (February 2015)."The environment of regulatory T cell biology: cytokines, metabolites, and the microbiome".Front Immunol.6:61.doi:10.3389/fimmu.2015.00061.PMC4332351.PMID25741338.
Figure 1: Microbial-derived molecules promote colonic Treg differentiation. - ^abcdefgBourassa MW, Alim I, Bultman SJ, Ratan RR (June 2016)."Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health?".Neurosci. Lett.625:56–63.doi:10.1016/j.neulet.2016.02.009.PMC4903954.PMID26868600.
- ^van Hoogdalem, Edward; de Boer, Albertus G.; Breimer, Douwe D. (July 1991)."Pharmacokinetics of rectal drug administration, Part I. General considerations and clinical applications of centrally acting drugs".Clinical Pharmacokinetics.21(1): 14.doi:10.2165/00003088-199121010-00002.ISSN0312-5963.PMID1717195.Retrieved18 March2024.
the middle and inferior rectal veins drain the lower part of the rectum and venous blood is returned to the inferior vena cava. Therefore, drugs absorbed in the latter system will be delivered preferentially to the systemic circulation, bypassing the liver and avoiding first-pass metabolism
- ^Tsuji A (2005)."Small molecular drug transfer across the blood–brain barrier via carrier-mediated transport systems".NeuroRx.2(1): 54–62.doi:10.1602/neurorx.2.1.54.PMC539320.PMID15717057.
Other in vivo studies in our laboratories indicated that several compounds including acetate, propionate, butyrate, benzoic acid, salicylic acid, nicotinic acid, and some β-lactam antibiotics may be transported by the MCT at the BBB.21... Uptake of valproic acid was reduced in the presence of medium-chain fatty acids such as hexanoate, octanoate, and decanoate, but not propionate or butyrate, indicating that valproic acid is taken up into the brain via a transport system for medium-chain fatty acids, not short-chain fatty acids.
- ^abVijay N, Morris ME (2014)."Role of monocarboxylate transporters in drug delivery to the brain".Curr. Pharm. Des.20(10): 1487–98.doi:10.2174/13816128113199990462.PMC4084603.PMID23789956.
Monocarboxylate transporters (MCTs) are known to mediate the transport of short chain monocarboxylates such as lactate, pyruvate and butyrate.... MCT1 and MCT4 have also been associated with the transport of short chain fatty acids such as acetate and formate which are then metabolized in the astrocytes [78].... SLC5A8 is expressed in normal colon tissue, and it functions as a tumor suppressor in human colon with silencing of this gene occurring in colon carcinoma. This transporter is involved in the concentrative uptake of butyrate and pyruvate produced as a product of fermentation by colonic bacteria.
- ^abButyric acid.University of Alberta.Retrieved15 August2015.
{{cite encyclopedia}}:|website=ignored (help) - ^"Butanoate metabolism – Reference pathway".Kyoto Encyclopedia of Genes and Genomes.Kanehisa Laboratories. 1 November 2017.Retrieved1 February2018.
- ^Donohoe, Dallas R.; Garge, Nikhil; Zhang, Xinxin; Sun, Wei; O'Connell, Thomas M.; Bunger, Maureen K.; Bultman, Scott J. (4 May 2011)."The Microbiome and Butyrate Regulate Energy Metabolism and Autophagy in the Mammalian Colon".Cell Metabolism.13(5): 517–526.doi:10.1016/j.cmet.2011.02.018.ISSN1550-4131.PMC3099420.PMID21531334.
- ^"triacylglycerol lipase – Homo sapiens".BRENDA.Technische Universität Braunschweig.Retrieved25 May2015.
- ^Tilg H, Moschen AR (September 2014). "Microbiota and diabetes: an evolving relationship".Gut.63(9): 1513–1521.doi:10.1136/gutjnl-2014-306928.PMID24833634.S2CID22633025.
- ^Cait, Alissa; Cardenas, Erick (December 2019)."Reduced genetic potential for butyrate fermentation in the gut microbiome of infants who develop allergic sensitization".Journal of Allergy and Clinical Immunology.144(6): 1638–1647. E3.doi:10.1016/j.jaci.2019.06.029.PMID31279007.
- ^Vatanen, T.; Franzosa, E.A.; Schwager, R.; et al. (2018)."The human gut microbiome in early-onset type 1 diabetes from the TEDDY study".Nature.562(7728): 589–594.Bibcode:2018Natur.562..589V.doi:10.1038/s41586-018-0620-2.PMC6296767.PMID30356183.
- ^Kumar J, Rani K, Datt C (2020). "Molecular link between dietary fibre, gut microbiota and health".Molecular Biology Reports.47(8): 6229–6237.doi:10.1007/s11033-020-05611-3.PMID32623619.S2CID220337072.
- ^Consolandi, Clarissa; Turroni, Silvia; Emmi, Giacomo; et al. (April 2015)."Behçet's syndrome patients exhibit specific microbiome signature".Autoimmunity Reviews.14(4): 269–276.doi:10.1016/j.autrev.2014.11.009.hdl:2158/962790.PMID25435420.
- ^Ye, Zi; Zhang, Ni; Wu, Chunyan; et al. (4 August 2018)."A metagenomic study of the gut microbiome in Behcet's disease".Microbiome.6(1): 135.doi:10.1186/s40168-018-0520-6.PMC6091101.PMID30077182.
- ^Di Bella, Stefano; Sanson, Gianfranco; Monticelli, Jacopo; Zerbato, Verena; Principe, Luigi; Giuffrè, Mauro; Pipitone, Giuseppe; Luzzati, Roberto (29 February 2024). Staley, Christopher (ed.)."Clostridioides difficile infection: history, epidemiology, risk factors, prevention, clinical manifestations, treatment, and future options".Clinical Microbiology Reviews.37(2). Mayuresh Abhyankar: e0013523.doi:10.1128/cmr.00135-23.ISSN0893-8512.PMID38421181.
- ^Cait, Alissa; Hughes, Michael R (May 2018)."Microbiome-driven allergic lung inflammation is ameliorated by short chain fatty acids".Mucosal Immunology.11(3): 785–796.doi:10.1038/mi.2017.75.PMID29067994.
- ^Furusawa, Yukihiro; Obata, Yuuki; Fukuda, Shinji; et al. (13 November 2013). "Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells".Nature.504(7480): 446–450.Bibcode:2013Natur.504..446F.doi:10.1038/nature12721.PMID24226770.S2CID4408815.
- ^Arpaia, Nicholas; Campbell, Clarissa; Fan, Xiying; et al. (13 November 2013)."Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation".Nature.504(7480): 451–455.Bibcode:2013Natur.504..451A.doi:10.1038/nature12726.PMC3869884.PMID24226773.
- ^Luu, Maik; Weigand, Katharina; Wedi, Fatana; et al. (26 September 2018)."Regulation of the effector function of CD8+ T cells by gut microbiota-derived metabolite butyrate".Scientific Reports.8(1): 14430.Bibcode:2018NatSR...814430L.doi:10.1038/s41598-018-32860-x.PMC6158259.PMID30258117.
- ^Cholan, Pradeep Manuneedhi; Han, Alvin; Woodie, Brad R.; Watchon, Maxinne; Kurz, Angela RM; Laird, Angela S.; Britton, Warwick J.; Ye, Lihua; Holmes, Zachary C.; McCann, Jessica R.; David, Lawrence A. (9 November 2020)."Conserved anti-inflammatory effects and sensing of butyrate in zebrafish".Gut Microbes.12(1): 1–11.doi:10.1080/19490976.2020.1824563.ISSN1949-0976.PMC7575005.PMID33064972.
- ^Vital, Marius; Gao, Jiarong; Rizzo, Mike; Harrison, Tara; Tiedje, James M. (2015)."Diet is a major factor governing the fecal butyrate-producing community structure across Mammalia, Aves and Reptilia".The ISME Journal.9(4): 832–843.Bibcode:2015ISMEJ...9..832V.doi:10.1038/ismej.2014.179.PMC4817703.PMID25343515.
- ^abcdWang G (2014)."Human antimicrobial peptides and proteins".Pharmaceuticals.7(5): 545–94.doi:10.3390/ph7050545.PMC4035769.PMID24828484.
Table 3: Select human antimicrobial peptides and their proposed targets
Table 4: Some known factors that induce antimicrobial peptide expression - ^Yonezawa H, Osaki T, Hanawa T, Kurata S, Zaman C, Woo TD, Takahashi M, Matsubara S, Kawakami H, Ochiai K, Kamiya S (2012). "Destructive effects of butyrate on the cell envelope of Helicobacter pylori".J. Med. Microbiol.61(Pt 4): 582–9.doi:10.1099/jmm.0.039040-0.PMID22194341.
- ^McGee DJ, George AE, Trainor EA, Horton KE, Hildebrandt E, Testerman TL (2011)."Cholesterol enhances Helicobacter pylori resistance to antibiotics and LL-37".Antimicrob. Agents Chemother.55(6): 2897–904.doi:10.1128/AAC.00016-11.PMC3101455.PMID21464244.
- ^Zimmerman MA, Singh N, Martin PM, Thangaraju M, Ganapathy V, Waller JL, Shi H, Robertson KD, Munn DH, Liu K (2012)."Butyrate suppresses colonic inflammation through HDAC1-dependent Fas upregulation and Fas-mediated apoptosis of T cells".Am. J. Physiol. Gastrointest. Liver Physiol.302(12): G1405–15.doi:10.1152/ajpgi.00543.2011.PMC3378095.PMID22517765.
- ^Offermanns S, Schwaninger M (2015). "Nutritional or pharmacological activation of HCA(2) ameliorates neuroinflammation".Trends Mol Med.21(4): 245–255.doi:10.1016/j.molmed.2015.02.002.PMID25766751.
- ^Chai JT, Digby JE, Choudhury RP (May 2013)."GPR109A and vascular inflammation".Curr Atheroscler Rep.15(5): 325.doi:10.1007/s11883-013-0325-9.PMC3631117.PMID23526298.
- ^Graff EC, Fang H, Wanders D, Judd RL (February 2016). "Anti-inflammatory effects of the hydroxycarboxylic acid receptor 2".Metab. Clin. Exp.65(2): 102–113.doi:10.1016/j.metabol.2015.10.001.PMID26773933.
- ^Farzi A, Reichmann F, Holzer P (2015)."The homeostatic role of neuropeptide Y in immune function and its impact on mood and behaviour".Acta Physiol (Oxf).213(3): 603–27.doi:10.1111/apha.12445.PMC4353849.PMID25545642.
- ^Zeng, Huawei; Lazarova, DL; Bordonaro, M (2014)."Mechanisms linking dietary fiber, gut microbiota and colon cancer prevention".World Journal of Gastrointestinal Oncology.6(2): 41–51.doi:10.4251/wjgo.v6.i2.41.PMC3926973.PMID24567795.
- ^Chen, Jiezhong; Zhao, Kong-Nan; Vitetta, Luis (2019)."Effects of Intestinal Microbial–Elaborated Butyrate on Oncogenic Signaling Pathways"(pdf).Nutrients.11(5): 1026.doi:10.3390/nu11051026.PMC6566851.PMID31067776.S2CID148568580.
- ^Klampfer L, Huang J, Sasazuki T, Shirasawa S, Augenlicht L (August 2004)."Oncogenic Ras promotes butyrate-induced apoptosis through inhibition of gelsolin expression".The Journal of Biological Chemistry.279(35): 36680–8.doi:10.1074/jbc.M405197200.PMID15213223.
- ^Vanhoutvin SA, Troost FJ, Hamer HM, Lindsey PJ, Koek GH, Jonkers DM, Kodde A, Venema K, Brummer RJ (2009). Bereswill S (ed.)."Butyrate-induced transcriptional changes in human colonic mucosa".PLOS ONE.4(8): e6759.Bibcode:2009PLoSO...4.6759V.doi:10.1371/journal.pone.0006759.PMC2727000.PMID19707587.
- ^Encarnação, J. C.; Abrantes, A. M.; Pires, A. S.; et al. (30 July 2015). "Revisit dietary fiber on colorectal cancer: butyrate and its role on prevention and treatment".Cancer and Metastasis Reviews.34(3): 465–478.doi:10.1007/s10555-015-9578-9.PMID26224132.S2CID18573671.
- ^Zimmerman, Mary A.; Singh, Nagendra; Martin, Pamela M.; et al. (15 June 2012)."Butyrate suppresses colonic inflammation through HDAC1-dependent Fas upregulation and Fas-mediated apoptosis of T cells".American Journal of Physiology. Gastrointestinal and Liver Physiology.302(12): G1405–G1415.doi:10.1152/ajpgi.00543.2011.PMC3378095.PMID22517765.
- ^Prasanna Kumar, S.; Thippeswamy, G.; Sheela, M.L.; et al. (October 2008). "Butyrate-induced phosphatase regulates VEGF and angiogenesis via Sp1".Archives of Biochemistry and Biophysics.478(1): 85–95.doi:10.1016/j.abb.2008.07.004.PMID18655767.
- ^"Low-carb diet cuts risk of colon cancer, study finds | University of Toronto Media Room".media.utoronto.ca.Retrieved4 May2016.
- ^Belcheva, Antoaneta; Irrazabal, Thergiory; Robertson, Susan J.; Streutker, Catherine; Maughan, Heather; Rubino, Stephen; Moriyama, Eduardo H.; Copeland, Julia K.; Kumar, Sachin (17 July 2014)."Gut microbial metabolism drives transformation of MSH2-deficient colon epithelial cells".Cell.158(2): 288–299.doi:10.1016/j.cell.2014.04.051.ISSN1097-4172.PMID25036629.
- ^Scheppach, W.; Sommer, H.; Kirchner, T.; et al. (1992)."Effect of butyrate enemas on the colonic mucosa in distal ulcerative colitis".Gastroenterology.103(1): 51–56.doi:10.1016/0016-5085(92)91094-K.PMID1612357.
- ^Robison AJ, Nestler EJ (November 2011)."Transcriptional and epigenetic mechanisms of addiction".Nat. Rev. Neurosci.12(11): 623–637.doi:10.1038/nrn3111.PMC3272277.PMID21989194.
- ^Nestler EJ (January 2014)."Epigenetic mechanisms of drug addiction".Neuropharmacology.76 Pt B: 259–268.doi:10.1016/j.neuropharm.2013.04.004.PMC3766384.PMID23643695.
- ^abWalker DM, Cates HM, Heller EA, Nestler EJ (February 2015)."Regulation of chromatin states by drugs of abuse".Curr. Opin. Neurobiol.30:112–121.doi:10.1016/j.conb.2014.11.002.PMC4293340.PMID25486626.
- ^Ajonijebu DC, Abboussi O, Russell VA, Mabandla MV, Daniels WM (August 2017)."Epigenetics: a link between addiction and social environment".Cellular and Molecular Life Sciences.74(15): 2735–2747.doi:10.1007/s00018-017-2493-1.PMC11107568.PMID28255755.S2CID40791780.
- ^Legastelois R, Jeanblanc J, Vilpoux C, Bourguet E, Naassila M (2017)."Mécanismes épigénétiques et troubles de l'usage d'alcool: une cible thérapeutique intéressante?"[Epigenetic mechanisms and alcohol use disorders: a potential therapeutic target].Biologie Aujourd'hui(in French).211(1): 83–91.doi:10.1051/jbio/2017014.PMID28682229.



