Sirolimus
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Rapamune, Fyarro, Hyftor |
| Other names | Rapamycin, ABI-009 |
| License data | |
| Pregnancy category |
|
| Routes of administration | By mouth,intravenous,topical |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokineticdata | |
| Bioavailability | 14% (oral solution), lower with high-fat meals; 18% (tablet), higher with high-fat meals[7] |
| Protein binding | 92% |
| Metabolism | Liver |
| Eliminationhalf-life | 57–63 hours[8] |
| Excretion | Mostly fecal |
| Identifiers | |
| |
| CAS Number | |
| PubChemCID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard(EPA) | |
| ECHA InfoCard | 100.107.147 |
| Chemical and physical data | |
| Formula | C51H79NO13 |
| Molar mass | 914.187g·mol−1 |
| 3D model (JSmol) | |
| Solubility in water | 0.0026[9] |
| |
| |
| (verify) | |
Sirolimus,also known asrapamycinand sold under the brand nameRapamuneamong others, is amacrolidecompound that is used to coatcoronary stents,preventorgan transplant rejection,treat a rare lung disease calledlymphangioleiomyomatosis,and treat perivascular epithelioid cell tumor (PEComa).[2][3][10][11]It hasimmunosuppressantfunctions in humans and is especially useful in preventing the rejection ofkidneytransplants. It is amechanistic target of rapamycin(mTOR) kinase inhibitor[3]that reduces the sensitivity ofT cellsandB cellstointerleukin-2(IL-2), inhibiting their activity.[12]
This compound also has a use in cardiovasculardrug-eluting stenttechnologies to inhibitrestenosis.
It is produced by thebacteriumStreptomyces hygroscopicusand was isolated for the first time in 1972, from samples ofStreptomyces hygroscopicusfound onEaster Island.[13][14][15]The compound was originally named rapamycin after the native name of the island, Rapa Nui.[10]Sirolimus was initially developed as anantifungalagent. However, this use was abandoned when it was discovered to have potent immunosuppressive andantiproliferativeproperties due to itsability to inhibit mTOR.It was approved by the U.S.Food and Drug Administration(FDA) in September 1999.[16]Hyftor was approved for treatment of facialangiofibromain the European Union in May 2023.[6]
Medical uses
[edit]Sirolimus isindicatedfor thepreventionoforgan transplant rejectionand for the treatment oflymphangioleiomyomatosis(LAM).[2]
Sirolimus (Fyarro), as protein-bound particles, is indicated for the treatment of adults with locally advanced unresectable or metastaticmalignantperivascular epithelioid cell tumor(PEComa).[3][17]
In the EU, sirolimus, as Rapamune, is indicated for the prophylaxis of organ rejection in adults at low to moderate immunological risk receiving a renal transplant[5]and, as Hyftor, is indicated for the treatment of facialangiofibromaassociated withtuberous sclerosiscomplex.[6]
Prevention of transplant rejection
[edit]The chief advantage sirolimus has overcalcineurin inhibitorsis its low toxicity toward kidneys. Transplant patients maintained on calcineurin inhibitors long-term tend to develop impaired kidney function or evenkidney failure;this can be avoided by using sirolimus instead. It is particularly advantageous in patients with kidney transplants forhemolytic-uremic syndrome,as this disease is likely to recur in the transplanted kidney if a calcineurin-inhibitor is used. However, on 7 October 2008, the FDA approved safety labeling revisions for sirolimus to warn of the risk for decreased renal function associated with its use.[18][19]In 2009, the FDA notified healthcare professionals that a clinical trial conducted by Wyeth showed an increased mortality in stable liver transplant patients after switching from a calcineurin inhibitor-based immunosuppressive regimen to sirolimus.[20]A 2019 cohort study of nearly 10,000 lung transplant recipients in the US demonstrated significantly improved long-term survival using sirolimus + tacrolimus instead of mycophenolate mofetil + tacrolimus for immunosuppressive therapy starting at one year after transplant.[21]
Sirolimus can also be used alone, or in conjunction with acalcineurin inhibitor(such astacrolimus), and/ormycophenolate mofetil,to provide steroid-free immunosuppression regimens. Impaired wound healing andthrombocytopeniaare possible side effects of sirolimus; therefore, some transplant centers prefer not to use it immediately after the transplant operation, but instead administer it only after a period of weeks or months. Its optimal role in immunosuppression has not yet been determined, and it remains the subject of a number of ongoing clinical trials.[12]
Lymphangioleiomyomatosis
[edit]In May 2015, the FDA approved sirolimus to treatlymphangioleiomyomatosis(LAM), a rare, progressive lung disease that primarily affects women of childbearing age. This made sirolimus the first drug approved to treat this disease.[22]LAM involves lung tissue infiltration withsmooth muscle-like cells with mutations of thetuberous sclerosis complexgene (TSC2). Loss of TSC2 gene function activates themTORsignaling pathway, resulting in the release of lymphangiogenicgrowth factors.Sirolimus blocks this pathway.[2]
The safety and efficacy of sirolimus treatment of LAM were investigated inclinical trialsthat compared sirolimus treatment with aplacebogroup in 89 patients for 12 months. The patients were observed for 12 months after the treatment had ended. The most commonly reported side effects of sirolimus treatment of LAM were mouth and lip ulcers,diarrhea,abdominal pain, nausea, sore throat, acne, chest pain, leg swelling,upper respiratory tract infection,headache, dizziness, muscle pain and elevatedcholesterol.Serious side effects including hypersensitivity and swelling (edema) have been observed inrenal transplantpatients.[22]
While sirolimus was considered for treatment of LAM, it receivedorphan drugdesignation status because LAM is a rare condition.[22]
The safety of LAM treatment by sirolimus in people younger than 18 years old has not been tested.[2]
Coronary stent coating
[edit]The antiproliferative effect of sirolimus has also been used in conjunction withcoronary stentsto prevent restenosis in coronary arteries following balloon angioplasty. The sirolimus is formulated in a polymer coating that affords controlled release through the healing period following coronary intervention. Several large clinical studies have demonstrated lower restenosis rates in patients treated with sirolimus-eluting stents when compared to bare-metal stents, resulting in fewer repeat procedures. A sirolimus-eluting coronary stent was marketed byCordis,a division ofJohnson & Johnson,under the tradenameCypher.[11]However, this kind of stent may also increase the risk of vascular thrombosis.[23]
Vascular malformations
[edit]Sirolimus is used to treat vascular malformations. Treatment with sirolimus can decrease pain and the fullness of vascular malformations, improve coagulation levels, and slow the growth of abnormal lymphatic vessels.[24]Sirolimus is a relatively new medical therapy for the treatment of vascular malformations[25]in recent years, sirolimus has emerged as a new medical treatment option for both vascular tumors and vascular malformations, as a mammalian target of rapamycin (mTOR), capable of integrating signals from the PI3K/AKT pathway to coordinate proper cell growth and proliferation. Hence, sirolimus is ideal for "proliferative" vascular tumors through the control of tissue overgrowth disorders caused by inappropriate activation of the PI3K/AKT/mTOR pathway as an antiproliferative agent.[26][27]
Angiofibromas
[edit]Sirolimus has been used as a topical treatment ofangiofibromaswithtuberous sclerosiscomplex (TSC). Facial angiofibromas occur in 80% of patients with TSC, and the condition is very disfiguring. A retrospective review of English-language medical publications reporting on topical sirolimus treatment of facial angiofibromas found sixteen separate studies with positive patient outcomes after using the drug. The reports involved a total of 84 patients, and improvement was observed in 94% of subjects, especially if treatment began during the early stages of the disease. Sirolimus treatment was applied in several different formulations (ointment, gel, solution, and cream), ranging from 0.003 to 1% concentrations. Reported adverse effects included one case of perioral dermatitis, one case of cephalea, and four cases of irritation.[28]
In April 2022, sirolimus was approved by the FDA for treating angiofibromas.[29]
Adverse effects
[edit]The most common adverse reactions (≥30% occurrence, leading to a 5% treatment discontinuation rate) observed with sirolimus in clinical studies of organ rejection prophylaxis in individuals with kidney transplants include:peripheral edema,hypercholesterolemia,abdominal pain, headache, nausea, diarrhea, pain, constipation,hypertriglyceridemia,hypertension,increasedcreatinine,fever,urinary tract infection,anemia,arthralgia,andthrombocytopenia.[2]
The most common adverse reactions (≥20% occurrence, leading to an 11% treatment discontinuation rate) observed with sirolimus in clinical studies for the treatment of lymphangioleiomyomatosis are: peripheral edema, hypercholesterolemia, abdominal pain, headache, nausea, diarrhea, chest pain,stomatitis,nasopharyngitis,acne,upper respiratory tract infection,dizziness, andmyalgia.[2]
The following adverse effects occurred in 3–20% of individuals taking sirolimus for organ rejection prophylaxis following a kidney transplant:[2]
| System | Adverse effects |
|---|---|
| Body as a whole | Sepsis,lymphocele,herpes zosterinfection,herpes simplexinfection |
| Cardiovascular | Venous thromboembolism(pulmonary embolismanddeep venous thrombosis),rapid heart rate |
| Digestive | Stomatitis |
| Hematologic/lymphatic | Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome(TTP/HUS),leukopenia |
| Metabolic | Abnormal healing, increasedlactic dehydrogenase(LDH),hypokalemia,diabetes |
| Musculoskeletal | Bonenecrosis |
| Respiratory | Pneumonia,epistaxis |
| Skin | Melanoma,squamous cell carcinoma,basal cell carcinoma |
| Urogenital | Pyelonephritis,ovarian cysts,menstrual disorders (amenorrheaandmenorrhagia) |
Diabetes-like symptoms
[edit]While sirolimus inhibition ofmTORC1appears to mediate the drug's benefits, it also inhibitsmTORC2,which results in diabetes-like symptoms.[30]This includes decreased glucose tolerance and insensitivity to insulin.[30]Sirolimus treatment may additionally increase the risk of type 2 diabetes.[31]In mouse studies, these symptoms can be avoided through the use of alternate dosing regimens oranalogssuch aseverolimusortemsirolimus.[32]
Lung toxicity
[edit]Lung toxicity is a serious complication associated with sirolimus therapy,[33][34][35][36][37][38][39][excessive citations]especially in the case of lung transplants.[40]The mechanism of theinterstitial pneumonitiscaused by sirolimus and other macrolideMTORinhibitors is unclear, and may have nothing to do with themTORpathway.[41][42][43]The interstitial pneumonitis is not dose-dependent, but is more common in patients with underlying lung disease.[33][44]
Lowered effectiveness of immune system
[edit]There have been warnings about the use of sirolimus in transplants, where it may increase mortality due to an increased risk of infections.[2]
Cancer risk
[edit]Sirolimus may increase an individual's risk for contractingskin cancersfrom exposure to sunlight or UV radiation, and risk of developinglymphoma.[2]In studies, the skin cancer risk under sirolimus was lower than under other immunosuppressants such asazathioprineandcalcineurin inhibitors,and lower than underplacebo.[2][45]
Impaired wound healing
[edit]Individuals taking sirolimus are at increased risk of experiencing impaired or delayed wound healing, particularly if they have abody mass indexin excess of 30 kg/m2(classified as obese).[2]
Interactions
[edit]Sirolimus is metabolized by theCYP3A4enzymeand is a substrate of theP-glycoprotein(P-gp)efflux pump;hence, inhibitors of either protein may increase sirolimus concentrations inblood plasma,whereas inducers of CYP3A4 and P-gp may decrease sirolimus concentrations in blood plasma.[2]
Pharmacology
[edit]Pharmacodynamics
[edit]Unlike the similarly namedtacrolimus,sirolimus is not acalcineurin inhibitor,but it has a similar suppressive effect on the immune system. Sirolimus inhibits IL-2 and other cytokine receptor-dependent signal transduction mechanisms, via action onmTOR,and thereby blocks activation ofTandB cells.Ciclosporin and tacrolimus inhibit the secretion of IL-2, by inhibitingcalcineurin.[12]
The mode of action of sirolimus is to bind thecytosolicproteinFK-binding protein 12(FKBP12) in a manner similar to tacrolimus. Unlike the tacrolimus-FKBP12 complex, which inhibits calcineurin (PP2B), the sirolimus-FKBP12 complex inhibits themTOR(mammalian Target Of Rapamycin, rapamycin being another name for sirolimus) pathway by directly binding to mTOR Complex 1 (mTORC1).[12]
mTOR has also been called FRAP (FKBP-rapamycin-associated protein), RAFT (rapamycin and FKBP target), RAPT1, or SEP. The earlier names FRAP and RAFT were coined to reflect the fact that sirolimus must bind FKBP12 first, and only the FKBP12-sirolimus complex can bind mTOR. However, mTOR is now the widely accepted name, since Tor was first discovered via genetic and molecular studies of sirolimus-resistant mutants ofSaccharomyces cerevisiaethat identified FKBP12, Tor1, and Tor2 as the targets of sirolimus and provided robust support that the FKBP12-sirolimus complex binds to and inhibits Tor1 and Tor2.[46][12]
Pharmacokinetics
[edit]Sirolimus is metabolized by theCYP3A4enzymeand is a substrate of theP-glycoprotein(P-gp)efflux pump.[2]It has linear pharmacokinetics.[47]In studies on N=6 and N=36 subjects, peak concentration was obtained in 1.3 hours +/r- 0.5 hours and the terminal elimination was slow, with ahalf lifearound 60 hours +/- 10 hours.[48][47]Sirolimus was not found to effect the concentration ofciclosporin,which is also metabolized primarily by theCYP3A4enzyme.[47]
The bioavailabiliy of sirolimus is low, and the absorption of sirolimus into the blood stream from the intestine varies widely between patients, with some patients having up to eight times more exposure than others for the same dose. Drug levels are, therefore, taken to make sure patients get the right dose for their condition.[12][non-primary source needed]This is determined by taking a blood sample before the next dose, which gives the trough level. However, good correlation is noted between trough concentration levels and drug exposure, known as area under the concentration-time curve, for both sirolimus (SRL) and tacrolimus (TAC) (SRL: r2 = 0.83; TAC: r2 = 0.82), so only one level need be taken to know itspharmacokinetic(PK) profile. PK profiles of SRL and of TAC are unaltered by simultaneous administration. Dose-corrected drug exposure of TAC correlates with SRL (r2 = 0.8), so patients have similar bioavailability of both.[49][non-primary source needed]
Chemistry
[edit]This sectionneeds expansionwith: content on this topic from[8].You can help byadding to it.(August 2016) |
Sirolimus is anatural productandmacrocycliclactone.[8]
Biosynthesis
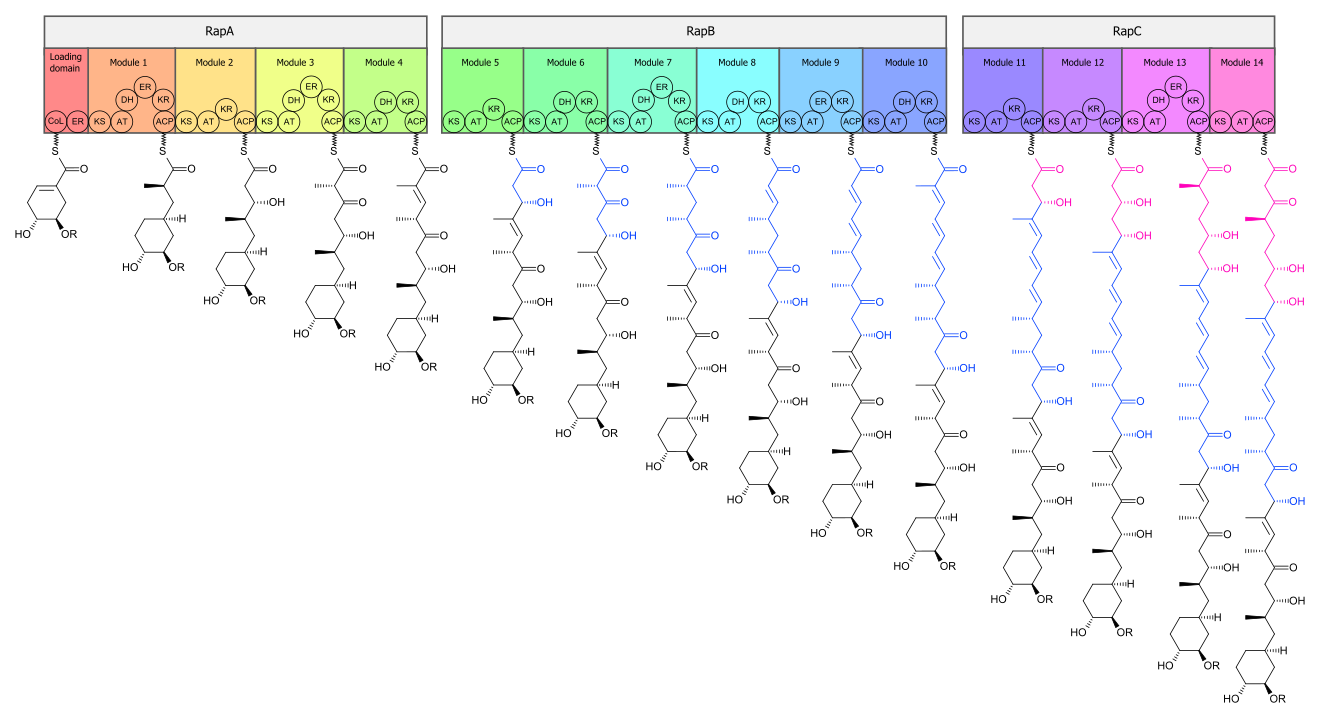
[edit]Thebiosynthesisof the rapamycin core is accomplished by a type Ipolyketide synthase(PKS) in conjunction with anonribosomal peptide synthetase(NRPS). The domains responsible for thebiosynthesisof the linearpolyketideof rapamycin are organized into three multienzymes, RapA, RapB, and RapC, which contain a total of 14 modules (figure 1). The three multienzymes are organized such that the first four modules of polyketide chain elongation are in RapA, the following six modules for continued elongation are in RapB, and the final four modules to complete thebiosynthesisof the linear polyketide are in RapC.[50]Then, the linearpolyketideis modified by the NRPS, RapP, which attaches L-pipecolate to the terminal end of the polyketide, and then cyclizes the molecule, yielding the unbound product, prerapamycin.[51]
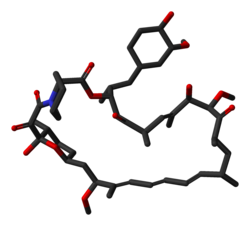
The coremacrocycle,prerapamycin (figure 2), is then modified (figure 3) by an additional five enzymes, which lead to the final product, rapamycin. First, the core macrocycle is modified by RapI, SAM-dependent O-methyltransferase (MTase), which O-methylates at C39. Next, a carbonyl is installed at C9 by RapJ, acytochrome P-450monooxygenases (P-450). Then, RapM, another MTase, O-methylates at C16. Finally, RapN, another P-450, installs a hydroxyl at C27 immediately followed by O-methylation by Rap Q, a distinct MTase, at C27 to yield rapamycin.[52]
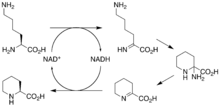
The biosyntheticgenesresponsible for rapamycin synthesis have been identified. As expected, three extremely largeopen reading frames(ORF's) designated asrapA,rapB,andrapCencode for three extremely large and complex multienzymes, RapA, RapB, and RapC, respectively.[50]ThegenerapLhas been established to code for aNAD+-dependentlysinecycloamidase, which converts L-lysineto L-pipecolic acid(figure 4) for incorporation at the end of the polyketide.[53][54]ThegenerapP,which is embedded between the PKS genes and translationally coupled torapC,encodes for an additionalenzyme,an NPRS responsible for incorporating L-pipecolic acid,chain terminationand cyclization of prerapamycin. In addition, genesrapI,rapJ,rapM,rapN,rapO,andrapQhave been identified as coding for tailoring enzymes that modify the macrocyclic core to give rapamycin (figure 3). Finally,rapGandrapHhave been identified to code for enzymes that have a positive regulatory role in the preparation of rapamycin through the control of rapamycin PKS gene expression.[55] Biosynthesis of this 31-membered macrocycle begins as the loading domain is primed with the starter unit, 4,5-dihydroxocyclohex-1-ene-carboxylic acid, which is derived from theshikimate pathway.[50]Note that thecyclohexanering of the starting unit is reduced during the transfer to module 1. The starting unit is then modified by a series ofClaisen condensationswithmalonylor methylmalonyl substrates, which are attached to anacyl carrier protein(ACP) and extend the polyketide by two carbons each. After each successivecondensation,the growing polyketide is further modified according to enzymatic domains that are present toreduceanddehydrateit, thereby introducing the diversity of functionalities observed in rapamycin (figure 1). Once the linear polyketide is complete, L-pipecolic acid, which is synthesized by a lysine cycloamidase from an L-lysine, is added to the terminal end of the polyketide by an NRPS. Then, the NSPS cyclizes the polyketide, giving prerapamycin, the first enzyme-free product. The macrocyclic core is then customized by a series of post-PKSenzymesthroughmethylationsby MTases andoxidationsby P-450s to yield rapamycin.
Research
[edit]
Cancer
[edit]The antiproliferative effects of sirolimus may have a role in treating cancer. When dosed appropriately, sirolimus can enhance the immune response to tumor targeting[56]or otherwise promote tumor regression in clinical trials.[57]Sirolimus seems to lower the cancer risk in some transplant patients.[58]
Sirolimus was shown to inhibit the progression of dermalKaposi's sarcomain patients with renal transplants.[59]OthermTOR inhibitors,such astemsirolimus(CCI-779) oreverolimus(RAD001), are being tested for use in cancers such asglioblastoma multiformeandmantle cell lymphoma.However, these drugs have a higher rate of fatal adverse events in cancer patients than control drugs.[60]
Acombination therapyofdoxorubicinand sirolimus has been shown to driveAkt-positive lymphomas intoremissionin mice. Akt signalling promotes cell survival in Akt-positive lymphomas and acts to prevent thecytotoxiceffects ofchemotherapydrugs, such asdoxorubicinorcyclophosphamide.Sirolimus blocks Akt signalling and the cells lose their resistance to the chemotherapy.Bcl-2-positive lymphomas were completely resistant to the therapy;eIF4E-expressing lymphomas are not sensitive to sirolimus.[61][62][63][64][65]
Tuberous sclerosis complex
[edit]Sirolimus also shows promise in treatingtuberous sclerosis complex(TSC), a congenital disorder that predisposes those afflicted to benign tumor growth in the brain, heart, kidneys, skin, and other organs. After several studies conclusively linked mTOR inhibitors to remission in TSC tumors, specifically subependymal giant-cell astrocytomas in children andangiomyolipomasin adults, many US doctors began prescribing sirolimus (Wyeth's Rapamune) andeverolimus(Novartis's RAD001) to TSC patients off-label. Numerous clinical trials using both rapamycin analogs, involving both children and adults with TSC, are underway in the United States.[66]
Effects on longevity
[edit]mTOR,specifically mTORC1, was first shown to be important in aging in 2003, in a study on worms; sirolimus was shown to inhibit and slow aging in worms, yeast, and flies, and then to improve the condition ofmouse modelsof various diseases of aging.[67][68]Sirolimus was first shown to extend lifespan in wild-type mice in a study published by NIH investigators in 2009; the studies have been replicated in mice of many different genetic backgrounds.[68]A study published in 2020 found late-life sirolimus dosing schedules enhanced mouse lifespan in a sex-specific manner where limited rapamycin exposure enhanced male lifespan but not female, providing evidence for sex differences in sirolimus response.[69][70]The results are further supported by the finding that genetically modified mice with impaired mTORC1 signalling live longer.[68]
Sirolimus has potential for widespread use as a longevity-promoting drug, with evidence pointing to its ability to prevent age-associated decline of cognitive and physical health. In 2014, researchers at Novartis showed a related compound,everolimus,increased elderly patients' immune response on an intermittent dose.[71]This led to many in the anti-aging community self-experimenting with the compound.[72]However, because of the different biochemical properties of Sirolimus the dosing is potentially very different than everolimus. Ultimately, due to known side effects of sirolimus, as well as inadequate evidence for optimal dosing, more research is required before sirolimus could be widely prescribed for this purpose.[68][73]
Sirolimus has complex effects on the immune system—whileIL-12goes up andIL-10decreases, which suggests an immunostimulatory response,TNFandIL-6are decreased, which suggests an immunosuppressive response. The duration of the inhibition and the exact extent to which mTORC1 and mTORC2 are inhibited play a role, but are not yet well understood.[74]
Topical administration
[edit]When applied as a topical preparation, researchers showed that rapamycin can regenerate collagen and reverse clinical signs of aging in elderly patients.[75]The concentrations are far lower than those used to treat angiofibromas.
SARS-CoV-2
[edit]Rapamycin has been proposed as a treatment forsevere acute respiratory syndrome coronavirus 2insofar as itsimmunosuppressiveeffects could prevent or reduce thecytokine stormseen in very serious cases of COVID-19.[76]Moreover, inhibition ofcell proliferationby rapamycin could reduceviral replication.[76]
Atherosclerosis
[edit]Rapamycin can accelerate degradation ofoxidized LDL cholesterolinendothelial cells,thereby lowering the risk of atherosclerosis.[77]Oxidized LDL cholesterol is a major contributor to atherosclerosis.[78]
Lupus
[edit]As of 2016, studies in cells, animals, and humans have suggested that mTOR activation as process underlyingsystemic lupus erythematosusand that inhibiting mTOR with rapamycin may be a disease-modifying treatment.[79]As of 2016 rapamycin had been tested in small clinical trials in people with lupus.[79]
Lymphatic malformation
[edit]Lymphatic malformation,or cystic hygroma, is an abnormal growth of lymphatic vessels that usually affects children around the head and neck. Treatment often consists of to removal of the tissue, but the rate of recurrence is high. Sirolimus has shown evidence of being helpful in alleviating symptoms and reducing the size of the malformation.[80]
Graft-versus-host disease
[edit]Due to its immunosuppressant activity, Rapamycin has been assessed as prophylaxis or treatment agent ofGraft-versus-host disease(GVHD), a complication ofhematopoietic stem cell transplantation.While contrasted results were obtained in clinical trials,[81]pre-clinical studies have shown that Rapamycin can mitigate GVHD by increasing the proliferation of regulatory T cells, inhibiting cytotoxic T cells and lowering the differentiation of effector T cells.[82][83]
Applications in biology research
[edit]Rapamycin is used in biology research as an agent forchemically induced dimerization.[84]In this application, rapamycin is added to cells expressing two fusion constructs, one of which contains the rapamycin-binding FRB domain from mTOR and the other of which contains an FKBP domain. Each fusion protein also contains additional domains that are brought into proximity when rapamycin induces binding of FRB and FKBP. In this way, rapamycin can be used to control and study protein localization and interactions.
Veterinary uses
[edit]A number ofveterinary medicineteaching hospitalsare participating in a long-termclinical studyexamining the effect of rapamycin on thelongevityofdogs.[85]
References
[edit]- ^"FDA-sourced list of all drugs with black box warnings (Use Download Full Results and View Query links.)".nctr-crs.fda.gov.FDA.Retrieved22 October2023.
- ^abcdefghijklmn"Rapamune- sirolimus solution Rapamune- sirolimus tablet, sugar coated".DailyMed.Archivedfrom the original on 27 November 2021.Retrieved26 November2021.
- ^abcd"Fyarro- sirolimus injection, powder, lyophilized, for suspension".DailyMed.Archivedfrom the original on 19 December 2021.Retrieved19 December2021.
- ^"Hyftor- sirolimus gel".DailyMed.28 January 2021.Archivedfrom the original on 24 March 2022.Retrieved23 March2022.
- ^ab"Rapamune EPAR".European Medicines Agency.17 September 2018.Archivedfrom the original on 13 August 2021.Retrieved26 November2021.
- ^abc"Hyftor EPAR".European Medicines Agency(EMA).9 June 2023.Retrieved12 June2023.Text was copied from this source which is copyright European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ^Buck ML (2006)."Immunosuppression With Sirolimus After Solid Organ Transplantation in Children".Pediatric Pharmacotherapy.12(2).Archivedfrom the original on 18 April 2020.Retrieved4 April2022.
- ^abc"Rapamycin".PubChem Compound.National Center for Biotechnology Information.Archivedfrom the original on 16 August 2016.Retrieved1 August2016.
- ^Simamora P, Alvarez JM, Yalkowsky SH (February 2001). "Solubilization of rapamycin".International Journal of Pharmaceutics.213(1–2): 25–29.doi:10.1016/s0378-5173(00)00617-7.PMID11165091.
- ^abVézina C, Kudelski A, Sehgal SN (October 1975)."Rapamycin (AY-22,989), a new antifungal antibiotic. I. Taxonomy of the producing streptomycete and isolation of the active principle".The Journal of Antibiotics.28(10): 721–726.doi:10.7164/antibiotics.28.721.PMID1102508.
- ^ab"Cypher Sirolimus-eluting Coronary Stent".Cypher Stent.Archived fromthe originalon 27 April 2003.Retrieved1 April2008.
- ^abcdefMukherjee S, Mukherjee U (1 January 2009)."A comprehensive review of immunosuppression used for liver transplantation".Journal of Transplantation.2009:701464.doi:10.1155/2009/701464.PMC2809333.PMID20130772.
- ^Qari S, Walters P, Lechtenberg S (21 May 2021)."The Dirty Drug and the Ice Cream Tub".Radiolab.Archivedfrom the original on 25 July 2021.Retrieved25 July2021.
- ^Seto B (November 2012)."Rapamycin and mTOR: a serendipitous discovery and implications for breast cancer".Clinical and Translational Medicine.1(1): 29.doi:10.1186/2001-1326-1-29.PMC3561035.PMID23369283.
- ^Pritchard DI (May 2005). "Sourcing a chemical succession for cyclosporin from parasites and human pathogens".Drug Discovery Today.10(10): 688–691.doi:10.1016/S1359-6446(05)03395-7.PMID15896681.
- ^"Drug Approval Package: Rapamune (Sirolimus) NDA# 021083".U.S.Food and Drug Administration(FDA).Archivedfrom the original on 1 February 2022.Retrieved1 February2022.
- ^"Aadi Bioscience Announces FDA Approval of its First Product Fyarro for Patients with Locally Advanced Unresectable or Metastatic Malignant Perivascular Epithelioid Cell Tumor (PEComa)".Aadi Bioscience, Inc.(Press release). 23 November 2021.Archivedfrom the original on 27 November 2021.Retrieved26 November2021.
- ^Li JJ, Corey EJ (3 April 2013).Drug Discovery: Practices, Processes, and Perspectives.John Wiley & Sons.ISBN978-1-118-35446-9.Archivedfrom the original on 19 August 2020.Retrieved1 August2016.
- ^Koprowski G (7 February 2012).Nanotechnology in Medicine: Emerging Applications.Momentum Press.ISBN978-1-60650-250-1.Archivedfrom the original on 30 September 2020.Retrieved1 August2016.
- ^"Sirolimus (marketed as Rapamune) Safety".U.S.Food and Drug Administration(FDA). 11 June 2009.Archivedfrom the original on 16 September 2016.Retrieved1 August2016.
- ^Wijesinha M, Hirshon JM, Terrin M, Magder L, Brown C, Stafford K, et al. (August 2019)."Survival Associated With Sirolimus Plus Tacrolimus Maintenance Without Induction Therapy Compared With Standard Immunosuppression After Lung Transplant".JAMA Network Open.2(8): e1910297.doi:10.1001/jamanetworkopen.2019.10297.PMC6716294.PMID31461151.
- ^abcPahon E (28 May 2015)."FDA approves Rapamune to treat LAM, a very rare lung disease".U.S.Food and Drug Administration(FDA).Archivedfrom the original on 14 August 2016.Retrieved1 August2016.
- ^Shuchman M (November 2006). "Trading restenosis for thrombosis? New questions about drug-eluting stents".The New England Journal of Medicine.355(19): 1949–1952.doi:10.1056/NEJMp068234.PMID17093244.
- ^"Venous Malformation: Treatments".Boston Children's Hospital.Archived fromthe originalon 17 January 2021.Retrieved22 April2020.
- ^Dekeuleneer V, Seront E, Van Damme A, Boon LM, Vikkula M (April 2020)."Theranostic Advances in Vascular Malformations".The Journal of Investigative Dermatology.140(4): 756–763.doi:10.1016/j.jid.2019.10.001.PMID32200879.
- ^Lee BB (January 2020)."Sirolimus in the treatment of vascular anomalies".Journal of Vascular Surgery.71(1): 328.doi:10.1016/j.jvs.2019.08.246.PMID31864650.
- ^Triana P, Dore M, Cerezo VN, Cervantes M, Sánchez AV, Ferrero MM, et al. (February 2017)."Sirolimus in the Treatment of Vascular Anomalies".European Journal of Pediatric Surgery.27(1): 86–90.doi:10.1055/s-0036-1593383.PMID27723921.
- ^Balestri R, Neri I, Patrizi A, Angileri L, Ricci L, Magnano M (January 2015). "Analysis of current data on the use of topical rapamycin in the treatment of facial angiofibromas in tuberous sclerosis complex".Journal of the European Academy of Dermatology and Venereology.29(1): 14–20.doi:10.1111/jdv.12665.PMID25174683.S2CID9967001.
- ^"FDA Approves Nobelpharma's Topical Treatment for Facial Angiofibroma".FDAnews.7 April 2022.Archivedfrom the original on 1 June 2022.Retrieved24 May2022.
- ^abLamming DW, Ye L, Katajisto P, Goncalves MD, Saitoh M, Stevens DM, et al. (March 2012)."Rapamycin-induced insulin resistance is mediated by mTORC2 loss and uncoupled from longevity".Science.335(6076): 1638–1643.Bibcode:2012Sci...335.1638L.doi:10.1126/science.1215135.PMC3324089.PMID22461615.
- ^Johnston O, Rose CL, Webster AC, Gill JS (July 2008)."Sirolimus is associated with new-onset diabetes in kidney transplant recipients".Journal of the American Society of Nephrology.19(7): 1411–1418.doi:10.1681/ASN.2007111202.PMC2440303.PMID18385422.
- ^Arriola Apelo SI, Neuman JC, Baar EL, Syed FA, Cummings NE, Brar HK, et al. (February 2016)."Alternative rapamycin treatment regimens mitigate the impact of rapamycin on glucose homeostasis and the immune system".Aging Cell.15(1): 28–38.doi:10.1111/acel.12405.PMC4717280.PMID26463117.
- ^abChhajed PN, Dickenmann M, Bubendorf L, Mayr M, Steiger J, Tamm M (2006). "Patterns of pulmonary complications associated with sirolimus".Respiration; International Review of Thoracic Diseases.73(3): 367–374.doi:10.1159/000087945.PMID16127266.S2CID24408680.
- ^Morelon E, Stern M, Israël-Biet D, Correas JM, Danel C, Mamzer-Bruneel MF, et al. (September 2001)."Characteristics of sirolimus-associated interstitial pneumonitis in renal transplant patients".Transplantation.72(5): 787–790.doi:10.1097/00007890-200109150-00008.PMID11571438.S2CID12116798.
- ^Filippone EJ, Carson JM, Beckford RA, Jaffe BC, Newman E, Awsare BK, et al. (September 2011)."Sirolimus-induced pneumonitis complicated by pentamidine-induced phospholipidosis in a renal transplant recipient: a case report".Transplantation Proceedings.43(7): 2792–2797.doi:10.1016/j.transproceed.2011.06.060.PMID21911165.Archivedfrom the original on 7 August 2020.Retrieved24 September2019.
- ^Pham PT, Pham PC, Danovitch GM, Ross DJ, Gritsch HA, Kendrick EA, et al. (April 2004)."Sirolimus-associated pulmonary toxicity".Transplantation.77(8): 1215–1220.doi:10.1097/01.TP.0000118413.92211.B6.PMID15114088.S2CID24496443.
- ^Mingos MA, Kane GC (December 2005)."Sirolimus-induced interstitial pneumonitis in a renal transplant patient"(PDF).Respiratory Care.50(12): 1659–1661.PMID16318648.Archived(PDF)from the original on 5 June 2022.Retrieved4 April2022.
- ^Das BB, Shoemaker L, Subramanian S, Johnsrude C, Recto M, Austin EH (March 2007). "Acute sirolimus pulmonary toxicity in an infant heart transplant recipient: case report and literature review".The Journal of Heart and Lung Transplantation.26(3): 296–298.doi:10.1016/j.healun.2006.12.004.PMID17346635.
- ^Delgado JF, Torres J, José Ruiz-Cano M, Sánchez V, Escribano P, Borruel S, et al. (September 2006). "Sirolimus-associated interstitial pneumonitis in 3 heart transplant recipients".The Journal of Heart and Lung Transplantation.25(9): 1171–1174.doi:10.1016/j.healun.2006.05.013.PMID16962483.
- ^McWilliams TJ, Levvey BJ, Russell PA, Milne DG, Snell GI (February 2003). "Interstitial pneumonitis associated with sirolimus: a dilemma for lung transplantation".The Journal of Heart and Lung Transplantation.22(2): 210–213.doi:10.1016/S1053-2498(02)00564-8.PMID12581772.
- ^Aparicio G, Calvo MB, Medina V, Fernández O, Jiménez P, Lema M, et al. (August 2009). "Comprehensive lung injury pathology induced by mTOR inhibitors".Clinical & Translational Oncology.11(8): 499–510.doi:10.1007/s12094-009-0394-y.hdl:2183/19864.PMID19661024.S2CID39914334.
- ^Paris A, Goupil F, Kernaonet E, Foulet-Rogé A, Molinier O, Gagnadoux F, et al. (January 2012). "[Drug-induced pneumonitis due to sirolimus: an interaction with atorvastatin?]".Revue des Maladies Respiratoires(in French).29(1): 64–69.doi:10.1016/j.rmr.2010.03.026.PMID22240222.
- ^Maroto JP, Hudes G, Dutcher JP, Logan TF, White CS, Krygowski M, et al. (May 2011)."Drug-related pneumonitis in patients with advanced renal cell carcinoma treated with temsirolimus".Journal of Clinical Oncology.29(13): 1750–1756.doi:10.1200/JCO.2010.29.2235.PMID21444868.
- ^Errasti P, Izquierdo D, Martín P, Errasti M, Slon F, Romero A, et al. (October 2010). "Pneumonitis associated with mammalian target of rapamycin inhibitors in renal transplant recipients: a single-center experience".Transplantation Proceedings.42(8): 3053–3054.doi:10.1016/j.transproceed.2010.07.066.PMID20970608.
- ^Euvrard S, Morelon E, Rostaing L, Goffin E, Brocard A, Tromme I, et al. (July 2012)."Sirolimus and secondary skin-cancer prevention in kidney transplantation".The New England Journal of Medicine.367(4): 329–339.doi:10.1056/NEJMoa1204166.hdl:2445/178597.PMID22830463.
- ^Heitman J, Movva NR, Hall MN (August 1991). "Targets for cell cycle arrest by the immunosuppressant rapamycin in yeast".Science.253(5022): 905–909.Bibcode:1991Sci...253..905H.doi:10.1126/science.1715094.PMID1715094.S2CID9937225.
- ^abcFerron GM, Mishina EV, Zimmerman JJ, Jusko WJ (April 1997). "Population pharmacokinetics of sirolimus in kidney transplant patients".Clinical Pharmacology and Therapeutics.61(4): 416–428.doi:10.1016/S0009-9236(97)90192-2.PMID9129559.
- ^Leung LY, Lim HK, Abell MW, Zimmerman JJ (February 2006). "Pharmacokinetics and metabolic disposition of sirolimus in healthy male volunteers after a single oral dose".Therapeutic Drug Monitoring.28(1): 51–61.doi:10.1097/01.ftd.0000179838.33020.34.PMID16418694.
- ^McAlister VC, Mahalati K, Peltekian KM, Fraser A, MacDonald AS (June 2002). "A clinical pharmacokinetic study of tacrolimus and sirolimus combination immunosuppression comparing simultaneous to separated administration".Therapeutic Drug Monitoring.24(3): 346–350.doi:10.1097/00007691-200206000-00004.PMID12021624.S2CID34950948.
- ^abcSchwecke T, Aparicio JF, Molnár I, König A, Khaw LE, Haydock SF, et al. (August 1995)."The biosynthetic gene cluster for the polyketide immunosuppressant rapamycin".Proceedings of the National Academy of Sciences of the United States of America.92(17): 7839–7843.Bibcode:1995PNAS...92.7839S.doi:10.1073/pnas.92.17.7839.PMC41241.PMID7644502.
- ^Gregory MA, Gaisser S, Lill RE, Hong H, Sheridan RM, Wilkinson B, et al. (May 2004). "Isolation and characterization of pre-rapamycin, the first macrocyclic intermediate in the biosynthesis of the immunosuppressant rapamycin by S. hygroscopicus".Angewandte Chemie.43(19): 2551–2553.doi:10.1002/anie.200453764.PMID15127450.
- ^Gregory MA, Hong H, Lill RE, Gaisser S, Petkovic H, Low L, et al. (October 2006). "Rapamycin biosynthesis: Elucidation of gene product function".Organic & Biomolecular Chemistry.4(19): 3565–3568.doi:10.1039/b608813a.PMID16990929.
- ^Graziani EI (May 2009). "Recent advances in the chemistry, biosynthesis and pharmacology of rapamycin analogs".Natural Product Reports.26(5): 602–609.doi:10.1039/b804602f.PMID19387497.
- ^Gatto GJ, Boyne MT, Kelleher NL, Walsh CT (March 2006). "Biosynthesis of pipecolic acid by RapL, a lysine cyclodeaminase encoded in the rapamycin gene cluster".Journal of the American Chemical Society.128(11): 3838–3847.doi:10.1021/ja0587603.PMID16536560.
- ^Aparicio JF, Molnár I, Schwecke T, König A, Haydock SF, Khaw LE, et al. (February 1996). "Organization of the biosynthetic gene cluster for rapamycin in Streptomyces hygroscopicus: analysis of the enzymatic domains in the modular polyketide synthase".Gene.169(1): 9–16.doi:10.1016/0378-1119(95)00800-4.PMID8635756.
- ^Li Q, Rao R, Vazzana J, Goedegebuure P, Odunsi K, Gillanders W, et al. (April 2012)."Regulating mammalian target of rapamycin to tune vaccination-induced CD8(+) T cell responses for tumor immunity".Journal of Immunology.188(7): 3080–3087.doi:10.4049/jimmunol.1103365.PMC3311730.PMID22379028.
- ^Easton JB, Houghton PJ (October 2006). "mTOR and cancer therapy".Oncogene.25(48): 6436–6446.doi:10.1038/sj.onc.1209886.PMID17041628.S2CID19250234.
- ^Law BK (October 2005). "Rapamycin: an anti-cancer immunosuppressant?".Critical Reviews in Oncology/Hematology.56(1): 47–60.doi:10.1016/j.critrevonc.2004.09.009.PMID16039868.
- ^"A new role for sirolimus: regression of Kaposi's sarcoma in kidney-transplant recipients".Nature Clinical Practice Urology.2(5): 211. May 2005.doi:10.1038/ncponc0156x.ISSN1743-4289.S2CID198175394.
- ^Bankhead C (17 February 2013)."Fatal AEs Higher with mTOR Drugs in Cancer".Med Page Today.Archivedfrom the original on 28 February 2021.Retrieved19 February2013.
- ^Sun SY, Rosenberg LM, Wang X, Zhou Z, Yue P, Fu H, et al. (August 2005). "Activation of Akt and eIF4E survival pathways by rapamycin-mediated mammalian target of rapamycin inhibition".Cancer Research.65(16): 7052–7058.doi:10.1158/0008-5472.CAN-05-0917.PMID16103051.
- ^Chan S (October 2004)."Targeting the mammalian target of rapamycin (mTOR): a new approach to treating cancer".British Journal of Cancer.91(8): 1420–1424.doi:10.1038/sj.bjc.6602162.PMC2409926.PMID15365568.
- ^Wendel HG, De Stanchina E, Fridman JS, Malina A, Ray S, Kogan S, et al. (March 2004). "Survival signalling by Akt and eIF4E in oncogenesis and cancer therapy".Nature.428(6980): 332–337.Bibcode:2004Natur.428..332W.doi:10.1038/nature02369.PMID15029198.S2CID4426215.
- ^"Combination therapy drives cancer into remission".Cold Spring Harbor Laboratory.17 March 2004.Archivedfrom the original on 1 June 2022.Retrieved23 March2022.
- ^Novak K (May 2004)."Therapeutics: Means to an end".Nature Reviews Cancer.4(5): 332.doi:10.1038/nrc1349.S2CID45906785.
- ^Li M, Zhou Y, Chen C, Yang T, Zhou S, Chen S, et al. (February 2019)."Efficacy and safety of mTOR inhibitors (rapamycin and its analogues) for tuberous sclerosis complex: a meta-analysis".Orphanet Journal of Rare Diseases.14(1): 39.doi:10.1186/s13023-019-1012-x.PMC6373010.PMID30760308.
- ^Lawton G."What is rapamycin?".New Scientist.Archivedfrom the original on 25 July 2021.Retrieved25 July2021.
- ^abcdArriola Apelo SI, Lamming DW (July 2016)."Rapamycin: An InhibiTOR of Aging Emerges From the Soil of Easter Island".The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences.71(7): 841–849.doi:10.1093/gerona/glw090.PMC4906330.PMID27208895.
A diverse and severe set of negative side effects likely preclude the wide-scale use of rapamycin and its analogs as a prolongevity agent.
- ^Strong R, Miller RA, Bogue M, Fernandez E, Javors MA, Libert S, et al. (November 2020)."Rapamycin-mediated mouse lifespan extension: Late-life dosage regimes with sex-specific effects".Aging Cell.19(11): e13269.doi:10.1111/acel.13269.PMC7681050.PMID33145977.
- ^"Late-Life Rapamycin Regimens Extend Mouse Lifespan in a Sex-Specific Manner".Nicotinamide Mononucleotide (NMN).11 November 2020.Archivedfrom the original on 28 February 2021.Retrieved23 March2022.
- ^Mannick JB, Del Giudice G, Lattanzi M, Valiante NM, Praestgaard J, Huang B, et al. (December 2014). "mTOR inhibition improves immune function in the elderly".Science Translational Medicine.6(268): 268ra179.doi:10.1126/scitranslmed.3009892.PMID25540326.S2CID206685475.
- ^Janin A (May 2023)."Can a Kidney Transplant Drug Keep You From Aging?".Wall Street Journal.Archivedfrom the original on 8 May 2023.Retrieved9 May2023.
- ^Johnson SC, Rabinovitch PS, Kaeberlein M (January 2013)."mTOR is a key modulator of ageing and age-related disease".Nature.493(7432): 338–345.Bibcode:2013Natur.493..338J.doi:10.1038/nature11861.PMC3687363.PMID23325216.
- ^Weichhart T, Hengstschläger M, Linke M (October 2015)."Regulation of innate immune cell function by mTOR".Nature Reviews. Immunology.15(10): 599–614.doi:10.1038/nri3901.PMC6095456.PMID26403194.
- ^Chung CL, Lawrence I, Hoffman M, Elgindi D, Nadhan K, Potnis M, et al. (December 2019)."Topical rapamycin reduces markers of senescence and aging in human skin: an exploratory, prospective, randomized trial".GeroScience.41(6): 861–869.doi:10.1007/s11357-019-00113-y.PMC6925069.PMID31761958.
- ^abHusain A, Byrareddy SN (November 2020)."Rapamycin as a potential repurpose drug candidate for the treatment of COVID-19".Chemico-Biological Interactions.331:109282.Bibcode:2020CBI...33109282H.doi:10.1016/j.cbi.2020.109282.PMC7536130.PMID33031791.
- ^Liu Y, Yang F, Zou S, Qu L (2019)."Rapamycin: A Bacteria-Derived Immunosuppressant That Has Anti-atherosclerotic Effects and Its Clinical Application".Frontiers in Pharmacology.9:1520.doi:10.3389/fphar.2018.01520.PMC6330346.PMID30666207.
- ^Stocker R, Keaney JF (October 2004). "Role of oxidative modifications in atherosclerosis".Physiological Reviews.84(4): 1381–1478.doi:10.1152/physrev.00047.2003.PMID15383655.
- ^abOaks Z, Winans T, Huang N, Banki K, Perl A (December 2016)."Activation of the Mechanistic Target of Rapamycin in SLE: Explosion of Evidence in the Last Five Years".Current Rheumatology Reports.18(12): 73.doi:10.1007/s11926-016-0622-8.PMC5314949.PMID27812954.
- ^Wiegand S, Dietz A, Wichmann G (August 2022)."Efficacy of sirolimus in children with lymphatic malformations of the head and neck".European Archives of Oto-Rhino-Laryngology.279(8): 3801–3810.doi:10.1007/s00405-022-07378-8.PMC9249683.PMID35526176.
- ^Lutz M, Mielke S (November 2016)."New perspectives on the use of mTOR inhibitors in allogeneic haematopoietic stem cell transplantation and graft-versus-host disease".British Journal of Clinical Pharmacology.82(5): 1171–1179.doi:10.1111/bcp.13022.PMC5061796.PMID27245261.
- ^Blazar BR, Taylor PA, Panoskaltsis-Mortari A, Vallera DA (June 1998)."Rapamycin inhibits the generation of graft-versus-host disease- and graft-versus-leukemia-causing T cells by interfering with the production of Th1 or Th1 cytotoxic cytokines".Journal of Immunology.160(11): 5355–5365.doi:10.4049/jimmunol.160.11.5355.PMID9605135.S2CID31313976.
- ^Ehx G, Ritacco C, Hannon M, Dubois S, Delens L, Willems E, et al. (August 2021)."Comprehensive analysis of the immunomodulatory effects of rapamycin on human T cells in graft-versus-host disease prophylaxis".American Journal of Transplantation.21(8): 2662–2674.doi:10.1111/ajt.16505.hdl:2268/256132.PMID33512760.S2CID231766741.
- ^Rivera VM, Clackson T, Natesan S, Pollock R, Amara JF, Keenan T, et al. (September 1996). "A humanized system for pharmacologic control of gene expression".Nature Medicine.2(9): 1028–1032.doi:10.1038/nm0996-1028.PMID8782462.S2CID30469863.
- ^
- "Study to assess healthy aging in dogs: the Dog Aging Project and Test of Rapamycin in Aging Dogs (TRIAD study)".University of Georgia College of Veterinary Medicine.29 July 2022.Archivedfrom the original on 23 February 2023.Retrieved23 February2023.
- "Dog Aging Project TRIAD Study".Washington State University Veterinary Teaching Hospital.28 March 2022.Archivedfrom the original on 23 February 2023.Retrieved23 February2023.
- "Dog aging project - TRIAD (Test of Rapamycin in Aging Dogs)".Iowa State University College of Veterinary Medicine.Archivedfrom the original on 23 February 2023.Retrieved23 February2023.
Further reading
[edit]- Benjamin D, Colombi M, Moroni C, Hall MN (October 2011). "Rapamycin passes the torch: a new generation of mTOR inhibitors".Nature Reviews. Drug Discovery.10(11): 868–880.doi:10.1038/nrd3531.PMID22037041.S2CID1227277.
- Freixo C, Ferreira V, Martins J, Almeida R, Caldeira D, Rosa M, et al. (January 2020)."Efficacy and safety of sirolimus in the treatment of vascular anomalies: A systematic review".Journal of Vascular Surgery.71(1): 318–327.doi:10.1016/j.jvs.2019.06.217.PMID31676179.S2CID207831199.
- Geeurickx M, Labarque V (September 2021). "A narrative review of the role of sirolimus in the treatment of congenital vascular malformations".Journal of Vascular Surgery. Venous and Lymphatic Disorders.9(5): 1321–1333.doi:10.1016/j.jvsv.2021.03.001.PMID33737259.
External links
[edit]- Clinical trial numberNCT02494570for "A Phase 2 Study of ABI-009 in Patients With Advanced Malignant PEComa (AMPECT)" atClinicalTrials.gov