Thromboxane
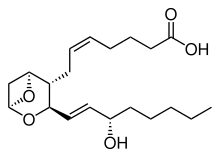

Thromboxaneis a member of the family oflipidsknown aseicosanoids.The two major thromboxanes arethromboxane A2andthromboxane B2.The distinguishing feature of thromboxanes is a 6-memberedether-containing ring.
Thromboxane is named for its role in blood clot formation (thrombosis).
Production[edit]


Thromboxane-A synthase,an enzyme found inplatelets,converts thearachidonic acidderivativeprostaglandin H2to thromboxane.
People withasthmatend to have increased thromboxane production, and analogs of thromboxane act as bronchoconstrictors in patients with asthma.[1]
Mechanism[edit]
Thromboxane acts by binding to any of thethromboxane receptors,G-protein-coupled receptorscoupled to theG proteinGq.[2]
Functions[edit]
Thromboxane is avasoconstrictorand a potent hypertensive agent, and it facilitates platelet aggregation.
It is inhomeostaticbalance in thecirculatory systemwithprostacyclin,a related compound. The mechanism of secretion of thromboxanes from platelets is still unclear. They act in the formation of blood clots and reduce blood flow to the site of a clot.
If the cap of a vulnerable plaque erodes or ruptures, as inmyocardial infarction,platelets stick to the damaged lining of the vessel and to each other within seconds and form a plug. These "Sticky platelets" secrete several chemicals, including thromboxane A2 that stimulate vasoconstriction, reducing blood flow at the site.
Role of A2 in platelet aggregation[edit]
Thromboxane A2(TXA2), produced by activated platelets, has prothrombotic properties, stimulating activation of new platelets as well as increasing platelet aggregation.
Platelet aggregation is achieved by mediating expression of the glycoprotein complexGP IIb/IIIain the cell membrane of platelets. Circulatingfibrinogenbinds these receptors on adjacent platelets, further strengthening theclot.
Pathology[edit]
It is believed that the vasoconstriction caused by thromboxanes plays a role inPrinzmetal's angina.Omega-3 fatty acidsare metabolized to produce higher levels of TxA3,which is relatively less potent than TxA2and PGI3;therefore, there is a balance shift toward inhibition of vasoconstriction and platelet aggregation. It is believed that this shift in balance lowers the incidence of myocardial infarction (heart attack) and stroke. Vasoconstriction and, perhaps, various proinflammatory effects exerted by TxA on tissue microvasculature, is probable reason why the TxA is pathogenic in various diseases, such as ischemia-reperfusion injury.,[3]hepatic inflammatory processes,[4]acute hepatotoxicity[5]etc. TxB2, a stable degradation product of TxA2, plays a role in acute hepatoxicity induced by acetaminophen.[6][7]
Thromboxane inhibitors[edit]
Thromboxane inhibitors are broadly classified as either those that inhibit the synthesis of thromboxane, or those that inhibit the target effect of it.
Thromboxane synthesis inhibitors, in turn, can be classified regarding which step in the synthesis they inhibit:
- The widely used drugaspirinacts by inhibiting the ability of the COX enzyme to synthesize the precursors of thromboxane within platelets. Low-dose, long-term aspirin use irreversibly blocks the formation ofthromboxane A2inplatelets,producing an inhibitory effect onplatelet aggregation.This anticoagulant property makes aspirin useful for reducing the incidence of heart attacks.[8]40 mg of aspirin a day is able to inhibit a large proportion of maximum thromboxane A2release provoked acutely, with the prostaglandin I2 synthesis being little affected; however, higher doses of aspirin are required to attain further inhibition.[9]
- Thromboxane synthase inhibitorsinhibit the final enzyme (thromboxane synthase) in the synthesis of thromboxane.Ifetrobanis a potent and selective thromboxane receptor antagonist.[10]Dipyridamoleantagonizes this receptor too, but has various other mechanisms of antiplatelet activity as well.
- High-dosenaproxencan induce near-complete suppression of platelet thromboxane throughout the dosing interval and appears not to increase cardiovascular disease (CVD) risk, whereas other high-dose NSAID (non-steroidal-anti-inflammatory) regimens have only transient effects on plateletCOX-1and have been found to be associated "with a small but definite vascular hazard".[11]
The inhibitors of the target effects of thromboxane are thethromboxane receptor antagonist,includingterutroban.
Picotamidehas activity both as a thromboxane synthase inhibitor and as a thromboxane receptor antagonist.[12]
Ridogrelis another example.[13]
References[edit]
- ^Chung, Kian Fan; Barnes, Peter J. (2009)."Mediator Antagonists".Asthma and COPD:655–662.doi:10.1016/B978-0-12-374001-4.00052-3.ISBN9780123740014.Retrieved20 January2023.
- ^Rat kidney thromboxane receptor: molecular cloning, signal...
- ^Ito Y (2003). "Effects of selective cyclooxygenase inhibitors on ischemia/reperfusion-induced hepatic microcirculatory dysfunction in mice".Eur Surg Res.35(5): 408–16.doi:10.1159/000072174.PMID12928598.S2CID40932766.
- ^Katagiri H (2004). "Role of thromboxane derived from COX-1 and -2 in hepatic microcirculatory dysfunction during endotoxemia in mice".Hepatology.39(1): 139–150.doi:10.1002/hep.20000.PMID14752832.S2CID27252438.
- ^Yokoyama Y (2005)."Role of thromboxane in producing hepatic injury during a hepatic stress disorder".Arch. Surg.140(8): 801–7.doi:10.1001/archsurg.140.8.801.PMID16103291.
- ^Cavar I (2011)."Anti-thromboxane B2 antibodies protect against acetaminophen-induced liver injury in mice".Journal of Xenobiotics.1(1): 38–44.doi:10.4081/xeno.2011.e8.
- ^Cavar I (2010). "The role of prostaglandin E2 in acute acetaminophen hepatotoxicity in mice".Histol Histopathol.25(7): 819–830.PMID20503171.
- ^[1]American Heart Association:Aspirin in Heart Attack and Stroke Prevention"The American Heart Association recommends aspirin use for patients who've had a myocardial infarction (heart attack), unstable angina, ischemic stroke (caused by blood clot) or transient ischemic attacks (TIAs or" little strokes "), if not contraindicated. This recommendation is based on sound evidence from clinical trials showing that aspirin helps prevent the recurrence of such events as heart attack, hospitalization for recurrent angina, second strokes, etc. (secondary prevention). Studies show aspirin also helps prevent these events from occurring in people at high risk (primary prevention)."[2]
- ^Tohgi, H; S Konno; K Tamura; B Kimura; K Kawano (1992). "Effects of low-to-high doses of aspirin on platelet aggregability and metabolites of thromboxane A2 and prostacyclin".Stroke.23(10): 1400–1403.doi:10.1161/01.STR.23.10.1400.PMID1412574.S2CID14177039.
- ^Dockens, RC; Santone, KS; Mitroka, JG; Morrison, RA; Jemal, M; Greene, DS; Barbhaiya, RH (Aug 2000). "Disposition of radiolabeled ifetroban in rats, dogs, monkeys, and humans".Drug Metabolism and Disposition.28(8): 973–80.PMID10901709.
- ^Coxib and traditional NSAID Trialists' (CNT) Collaboration (30 May 2013)."Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials".Lancet.382(9894): 769–79.doi:10.1016/S0140-6736(13)60900-9.PMC3778977.PMID23726390.
- ^Ratti, S; Quarato, P; Casagrande, C; Fumagalli, R; Corsini, A (1998). "Picotamide, an antithromboxane agent, inhibits the migration and proliferation of arterial myocytes".European Journal of Pharmacology.355(1): 77–83.doi:10.1016/S0014-2999(98)00467-1.PMID9754941.
- ^Di Perri, T.; Notari, M.; Assogna, G. (October 1991)."[Ridogrel, a new platelet antiaggregant molecule with a double mechanism of action. A pharmacological and clinical profile]".Recenti Progressi in Medicina.82(10): 533–540.ISSN0034-1193.PMID1759039.
External links[edit]
- Thromboxanesat the U.S. National Library of MedicineMedical Subject Headings(MeSH)
