Herbal medicine
| This article is part ofa serieson |
| Alternative medicine |
|---|
 |

Herbal medicine(also calledherbalism,phytomedicineorphytotherapy) is the study ofpharmacognosyand the use ofmedicinal plants,which are a basis oftraditional medicine.[1]With worldwide research intopharmacology,some herbal medicines have been translated into modern remedies, such as the anti-malarial group of drugs calledartemisininisolated fromArtemisia annua,a herb that was known inChinese medicineto treat fever.[2][3]There is limitedscientific evidencefor the safety and efficacy of many plants used in 21st-century herbalism, which generally does not provide standards for purity or dosage.[1][4]The scope of herbal medicine sometimes includesfungalandbeeproducts, as well asminerals,shellsand certain animal parts.[5]
Paraherbalismdescribesalternativeandpseudoscientificpractices of using unrefined plant or animalextractsas unproven medicines or health-promoting agents.[1][4][6][7]Paraherbalism relies on the belief that preserving various substances from a given source with less processing is safer or more effective than manufactured products, a concept for which there is no evidence.[6]
History
[edit]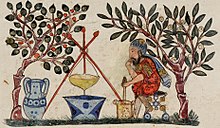
Archaeological evidence indicates that the use ofmedicinal plantsdates back to thePaleolithicage, approximately 60,000 years ago. Written evidence of herbal remedies dates back over 5,000 years to theSumerians,who compiled lists of plants. Some ancient cultures wrote about plants and their medical uses in books calledherbals.In ancient Egypt, herbs were mentioned inEgyptian medical papyri,depicted in tomb illustrations, or on rare occasions found in medical jars containing trace amounts of herbs.[8]In ancient Egypt, theEbers papyrusdates from about 1550 BCE, and covers more than 700 compounds, mainly of plant origin.[9]The earliest knownGreekherbals came fromTheophrastusof Eresos who, in the 4th century BCE, wrote inGreekHistoria Plantarum,fromDiocles of Carystuswho wrote during the 3rd century BCE, and from Krateuas who wrote in the 1st century BCE. Only a few fragments of these works have survived intact, but from what remains, scholars have noted overlap with the Egyptian herbals.[10]Seeds likely used for herbalism were found in archaeological sites ofBronze AgeChina dating from theShang dynasty[11](c. 1600– c. 1046 BCE). Over a hundred of the 224 compounds mentioned in theHuangdi Neijing,an early Chinese medical text, are herbs.[12]Herbs were also commonly used in thetraditional medicineof ancient India, where the principal treatment for diseases was diet.[13]De Materia Medica,originally written in Greek byPedanius Dioscorides(c. 40– c. 90 CE) ofAnazarbus,Cilicia,a physician and botanist, is one example of herbal writing used over centuries until the 1600s.[14]
Modern herbal medicine
[edit]TheWorld Health Organization(WHO) estimates that 80 percent of the population of some Asian and African countries presently uses herbal medicine for some aspect of primary health care.[15]
Someprescription drugshave a basis as herbal remedies, includingartemisinin,[16]digitalis,quinineandtaxanes.
Regulatory review
[edit]In 2015, theAustralian Government's Department of Healthpublished the results of a review of alternative therapies that sought to determine if any were suitable for being covered byhealth insurance;herbalism was one of 17 topics evaluated for which no clear evidence of effectiveness was found.[17]Establishing guidelines to assess the safety and efficacy of herbal products, theEuropean Medicines Agencyprovided criteria in 2017 for evaluating and grading the quality of clinical research in preparing monographs about herbal products.[18]In the United States, theNational Center for Complementary and Integrative Healthof theNational Institutes of Healthfunds clinical trials on herbal compounds, provides fact sheets evaluating the safety, potential effectiveness and side effects of many plant sources,[19]and maintains a registry of clinical research conducted on herbal products.[20]
According toCancer Research UKas of 2015, "there is currently no strong evidence from studies in people that herbal remedies can treat, prevent or cure cancer".[5]
Prevalence of use
[edit]The use of herbal remedies is more prevalent in people withchronic diseases,such as cancer,diabetes,asthma,andend-stage kidney disease.[21][22][23]Multiple factors such as gender, age, ethnicity, education and social class are also shown to have associations with the prevalence of herbal remedy use.[24]
Herbal preparations
[edit]
There are many forms in which herbs can be administered, the most common of which is a liquid consumed as a herbal tea or a (possibly diluted) plant extract.[25]
Herbal teas,or tisanes, are the resultant liquid of extracting herbs into water, though they are made in a few different ways.Infusionsare hot water extracts of herbs, such aschamomileormint,throughsteeping.Decoctionsare the long-term boiled extracts, usually of harder substances like roots or bark.Macerationis the cold infusion of plants with highmucilage-content, such assageorthyme.To make macerates, plants are chopped and added to cold water. They are then left to stand for 7 to 12 hours (depending on the herb used). For most macerates, 10 hours is used.[26]
Tincturesare alcoholic extracts of herbs, which are generally stronger than herbal teas.[27]Tinctures are usually obtained by combining pure ethanol (or a mixture of pure ethanol with water) with the herb. A completed tincture has an ethanol percentage of at least 25% (sometimes up to 90%).[26]Non-alcoholic tinctures can be made with glycerin but it is believed to be less absorbed by the body than alcohol based tinctures and has a shorter shelf life.[28]Herbal wine andelixirsare alcoholic extracts of herbs, usually with an ethanol percentage of 12–38%.[26]Extractsinclude liquid extracts, dry extracts, and nebulisates. Liquid extracts are liquids with a lower ethanol percentage than tinctures. They are usually made by vacuumdistillingtinctures. Dry extracts are extracts of plant material that areevaporatedinto a dry mass. They can then be further refined to a capsule or tablet.[26]
The exact composition of a herbal product is influenced by the method of extraction. A tea will be rich inpolarcomponents because water is apolar solvent.Oil on the other hand is anon-polarsolvent and it will absorb non-polar compounds. Alcohol lies somewhere in between.[25]

Many herbs are applied topically to the skin in a variety of forms.Essential oilextracts can be applied to the skin, usually diluted in a carrier oil. Many essential oils can burn the skin or are simply too high dose used straight; diluting them in olive oil or another food grade oil such as almond oil can allow these to be used safely as a topical.Salves,oils,balms,creams, and lotions are other forms of topical delivery mechanisms. Most topical applications are oil extractions of herbs. Taking a food grade oil and soaking herbs in it for anywhere from weeks to months allows certainphytochemicalsto be extracted into the oil. This oil can then be made into salves, creams, lotions, or simply used as an oil for topical application. Many massage oils, antibacterial salves, and wound healing compounds are made this way.[29]
Inhalation,as inaromatherapy,can be used as a treatment.[30][31][32]
Safety
[edit]
It is a popular misconception that herbal medicines are safe and side-effect free.[34]Consumption of herbs may causeadverse effects.[35]Furthermore, "adulteration, inappropriate formulation, or lack of understanding of plant and drug interactions have led to adverse reactions that are sometimes life threatening or lethal."[36]Proper double-blind clinical trials are needed to determine the safety and efficacy of each plant before medical use.[37]
Although many consumers believe that herbal medicines are safe because they are natural, herbal medicines and synthetic drugs may interact, causing toxicity to the consumer. Herbal remedies can also be dangerously contaminated, and herbal medicines without established efficacy, may unknowingly be used to replace prescription medicines.[38]
Standardization of purity and dosage is not mandated in the United States, but even products made to the same specification may differ as a result of biochemical variations within a species of plant.[39]Plants have chemical defense mechanisms against predators that can have adverse or lethal effects on humans. Examples of highly toxic herbs include poison hemlock and nightshade.[40]They are not marketed to the public as herbs, because the risks are well known, partly due to a long and colorful history in Europe, associated with "sorcery", "magic" and intrigue.[41]Although not frequent, adverse reactions have been reported for herbs in widespread use.[42]On occasion serious untoward outcomes have been linked to herb consumption. A case of major potassium depletion has been attributed to chronic licorice ingestion,[43]and consequently professional herbalists avoid the use of licorice where they recognize that this may be a risk. Black cohosh has been implicated in a case of liver failure.[44] Few studies are available on the safety of herbs for pregnant women,[45]and one study found that use of complementary and alternative medicines is associated with a 30% lower ongoing pregnancy and live birth rate during fertility treatment.[46]
Examples of herbal treatments with likely cause-effect relationships with adverse events includeaconite(which is often a legally restricted herb),Ayurvedic remedies,broom,chaparral,Chinese herb mixtures,comfrey,herbs containing certain flavonoids,germander,guar gum,liquorice root,andpennyroyal.[47]Examples of herbs that may have long-term adverse effects includeginseng,the endangered herbgoldenseal,milk thistle,senna,aloe vera juice,buckthorn bark and berry,cascara sagrada bark,saw palmetto,valerian,kava(which is banned in the European Union),St. John's wort,khat,betel nut,the restricted herbephedra,andguarana.[36]
There is also concern with respect to the numerous well-established interactions of herbs and drugs.[36][48]In consultation with a physician, usage of herbal remedies should be clarified, as some herbal remedies have the potential to cause adverse drug interactions when used in combination with various prescription andover-the-counterpharmaceuticals, just as a customer should inform a herbalist of their consumption of actual prescription and other medication.[49][50]
For example, dangerously low blood pressure may result from the combination of a herbal remedy that lowers blood pressure together with prescription medicine that has the same effect. Some herbs may amplify the effects of anticoagulants.[51] Certain herbs as well as common fruit interfere with cytochrome P450, an enzyme critical to much drug metabolism.[52]
In a 2018 study, the FDA identified activepharmaceutical additivesin over 700 analyzed dietary supplements sold as "herbal", "natural" or "traditional".[53]The undisclosed additives included "unapproved antidepressants and designer steroids", as well asprescription drugs,such assildenafilorsibutramine.
Labeling accuracy
[edit]Researchers at theUniversity of Adelaidefound in 2014 that almost 20 percent of herbal remedies surveyed were not registered with theTherapeutic Goods Administration,despite this being a condition for their sale.[54]They also found that nearly 60 percent of products surveyed had ingredients that did not match what was on the label. Out of 121 products, only 15 had ingredients that matched their TGA listing and packaging.[54]
In 2015, theNew York Attorney Generalissuedcease and desistletters to four major U.S. retailers (GNC,Target,Walgreens,andWalmart) who were accused of selling herbal supplements that were mislabeled and potentially dangerous.[55][56]Twenty-four products were tested byDNA barcodingas part of the investigation, with all but five containing DNA that did not match the product labels.
Practitioners of herbalism
[edit]
In some countries, formalized training and minimum education standards exist for herbalists, although these are not necessarily uniform within or between countries. In Australia, for example, the self-regulated status of the profession (as of 2009) resulted in variable standards of training, and numerous loosely formed associations setting different educational standards.[57]One 2009 review concluded that regulation of herbalists in Australia was needed to reduce the risk of interaction of herbal medicines withprescription drugs,to implement clinical guidelines and prescription of herbal products, and to assure self-regulation for protection of public health and safety.[57]In the United Kingdom, the training of herbalists is done by state-funded universities offering Bachelor of Science degrees in herbal medicine.[58]In the United States, according to the American Herbalist Guild, "there is currently no licensing or certification for herbalists in any state that precludes the rights of anyone to use, dispense, or recommend herbs."[59]However, there are U.S. federal restrictions for marketing herbs as cures for medical conditions, or essentially practicing as an unlicensed physician.
United States herbalism fraud
[edit]Over the years 2017–2021, theU.S. Food and Drug Administration(FDA) issuedwarning lettersto numerous herbalism companies for illegally marketing products under "conditions that cause them to be drugs under section 201(g)(1) of the Act [21 U.S.C. § 321(g)(1)], because they are intended for use in the diagnosis, cure, mitigation, treatment, or prevention of disease and/or intended to affect the structure or any function of the body" when no such evidence existed.[60][61][62]During theCOVID-19 pandemic,the FDA and U.S.Federal Trade Commissionissuedwarningsto several hundred American companies for promoting false claims that herbal products could prevent or treatCOVID-19 disease.[62][63]
Government regulations
[edit]TheWorld Health Organization(WHO), the specialized agency of the United Nations (UN) that is concerned with international public health, publishedQuality control methods for medicinal plant materialsin 1998 to support WHO Member States in establishing quality standards and specifications for herbal materials, within the overall context of quality assurance and control of herbal medicines.[64]
In the European Union (EU), herbal medicines are regulated under theCommittee on Herbal Medicinal Products.[65]
In the United States, herbal remedies are regulateddietary supplementsby theFood and Drug Administration(FDA) undercurrent good manufacturing practice(cGMP) policy for dietary supplements.[66]Manufacturers of products falling into this category are not required to prove the safety or efficacy of their product so long as they do not make 'medical' claims or imply uses other than as a 'dietary supplement', though the FDA may withdraw a product from sale should it prove harmful.[67][68]
Canadian regulations are described by the Natural and Non-prescription Health Products Directorate which requires an eight-digit Natural Product Number or Homeopathic Medicine Number on the label of licensed herbal medicines or dietary supplements.[69]
Some herbs, such ascannabisandcoca,are outright banned in most countries though coca is legal in most of the South American countries where it is grown. TheCannabisplantis used as a herbalmedicine,and as such islegalin some parts of the world. Since 2004, the sales ofephedraas a dietary supplement is prohibited in the United States by the FDA,[70]and subject to Schedule III restrictions in the United Kingdom.
Scientific criticism
[edit]Herbalism has been criticized as a potential "minefield"of unreliable product quality, safety hazards, and the potential for misleading health advice.[1][7]Globally, there are no standards across various herbal products to authenticate their contents, safety or efficacy,[39]and there is generally an absence of high-quality scientific research on product composition or effectiveness for anti-disease activity.[7][71]Presumed claims of therapeutic benefit from herbal products, without rigorous evidence of efficacy and safety, receive skeptical views by scientists.[1]
Unethical practices by some herbalists and manufacturers, which may include false advertising about health benefits on product labels or literature,[7]and contamination or use of fillers during product preparation,[39][72]may erodeconsumer confidenceabout services and products.[73][74]
Paraherbalism
[edit]
Paraherbalismis thepseudoscientificuse ofextractsof plant or animal origin as supposed medicines or health-promoting agents.[1][6][7]Phytotherapy differs from plant-derived medicines in standardpharmacologybecause it does not isolate andstandardizethe compounds from a given plant believed to be biologically active. It relies on the false belief that preserving the complexity of substances from a given plant with less processing is safer and potentially more effective, for which there is no evidence either condition applies.[6]
Phytochemical researcherVarro Eugene Tylerdescribed paraherbalism as "faulty or inferior herbalism based on pseudoscience", using scientific terminology but lacking scientific evidence for safety and efficacy. Tyler listed tenfallaciesthat distinguished herbalism from paraherbalism, including claims that there is aconspiracyto suppress safe and effective herbs, herbs cannot cause harm, whole herbs are more effective than molecules isolated from the plants, herbs are superior to drugs, thedoctrine of signatures(the belief that the shape of the plant indicates its function) is valid, dilution of substances increases their potency (a doctrine of the pseudoscience ofhomeopathy), astrological alignments are significant, animal testing is not appropriate to indicate human effects,anecdotal evidenceis an effective means of proving a substance works and herbs were created by God to cure disease. Tyler suggests that none of these beliefs have any basis in fact.[6][75]
Traditional systems
[edit]
Africa
[edit]Up to 80% of the population in Africa uses traditional medicine as primary health care.[76]
Americas
[edit]Native Americans used about 2,500 of the approximately 20,000 plant species that are native to North America.[77]
InAndeanhealing practices, the use ofentheogens,in particular the San Pedro cactus (Echinopsis pachanoi) is still a vital component, and has been around for millennia.[78]
China
[edit]Some researchers trained in both Western andtraditional Chinese medicinehave attempted to deconstruct ancient medical texts in the light of modern science. In 1972,Tu Youyou,a pharmaceutical chemist andNobel Prize winner,extracted the anti-malarial drugartemisininfromsweet wormwood,a traditional Chinese treatment for intermittent fevers.[79]
India
[edit]
In India,Ayurvedic medicinehas quite complex formulas with 30 or more ingredients, including a sizable number of ingredients that have undergone "alchemical processing",chosen to balancedosha.[80]In Ladakh, Lahul-Spiti, and Tibet, theTibetan Medical Systemis prevalent, also called the "Amichi Medical System". Over 337 species ofmedicinal plantshave been documented byC.P. Kala.Those are used by Amchis, the practitioners of this medical system.[81][82]The Indian book, Vedas, mentions treatment of diseases with plants.[83]
Indonesia
[edit]
InIndonesia,especially among theJavanese,thejamutraditional herbal medicine may have originated in theMataram Kingdomera, some 1300 years ago.[84]Thebas-reliefsonBorobudurdepict the image of people grinding herbs with stonemortar and pestle,a drink seller, a herbalist, andmasseusetreating people.[85]The Madhawapura inscription fromMajapahitperiod mentioned a specific profession of herb mixer and combiner (herbalist), calledAcaraki.[85]The book fromMataramdated from circa 1700 contains 3,000 entries of jamu herbal recipes, while Javanese classical literatureSerat Centhini(1814) describes some jamu herbal concoction recipes.[85]
Though possibly influenced by IndianAyurvedasystems, theIndonesia archipelagoholds numerous indigenous plants not found in India, including plants similar to those in Australia beyond theWallace Line.[86]Jamu practices may vary from region to region, and are often not recorded, especially in remote areas of the country.[87]Although primarily herbal, some Jamu materials are acquired from animals, such ashoney,royal jelly,milk, andAyam Kampungeggs.
Beliefs
[edit]Herbalists tend to use extracts from parts of plants, such as the roots or leaves,[88]believing that plants are subject to environmental pressures and therefore develop resistance to threats such as radiation,reactive oxygen speciesand microbial attack to survive, providing defensivephytochemicalsof use in herbalism.[88][89]
Use of plants by animals
[edit]Indigenous healers often claim to have learned by observing that sick animals change their food preferences to nibble at bitter herbs they would normally reject.[90]Field biologists have provided corroborating evidence based on observation of diverse species, such as chickens, sheep,butterflies,andchimpanzees.The habit of changing diet has been shown to be a physical means of purging intestinal parasites. Sick animals tend to forage plants rich insecondary metabolites,such astanninsandalkaloids.[91]
See also
[edit]- Chinese herbology
- Ethnobotany
- Ethnomedicine
- Herbal
- Medicinal fungi
- List of plants used in herbalism
- Traditional medicine
- Traditional Knowledge Digital Library
References
[edit]- ^abcdef"Hard to swallow".Nature.448(7150): 105–6. July 2007.Bibcode:2007Natur.448S.105..doi:10.1038/448106a.PMID17625521.
- ^"This Ancient Chinese Remedy Helped Win the Nobel Prize".Time.Archivedfrom the original on 3 November 2022.Retrieved11 October2021.
- ^Su, Xin-zhuan; Miller, Louis H. (November 2015)."The discovery of artemisinin and Nobel Prize in Physiology or Medicine".Science China Life Sciences.58(11): 1175–1179.doi:10.1007/s11427-015-4948-7.ISSN1674-7305.PMC4966551.PMID26481135.
- ^abLack CW, Rousseau J (2016).Critical Thinking, Science, and Pseudoscience: Why We Can't Trust Our Brains.Springer Publishing Company. pp. 212–214.ISBN9780826194268.
- ^ab"Herbal medicine".Cancer Research UK.2 February 2015.Archivedfrom the original on 29 May 2019.Retrieved12 November2018.
- ^abcdeTyler VE (31 August 1999)."False Tenets of Paraherbalism".Quackwatch.Archivedfrom the original on 11 November 2009.Retrieved29 October2016.
- ^abcdeBarrett S(23 November 2013)."The Herbal Minefield".Quackwatch.Archivedfrom the original on 5 August 2020.Retrieved25 February2017.
- ^Nunn J (2002).Ancient Egyptian Medicine.Vol. 113. University of Oklahoma Press. pp. 57–68.ISBN978-0-8061-3504-5.PMID10326089.
{{cite book}}:|journal=ignored (help) - ^Atanasov AG, Waltenberger B, Pferschy-Wenzig EM, Linder T, Wawrosch C, Uhrin P, et al. (December 2015)."Discovery and resupply of pharmacologically active plant-derived natural products: A review".Biotechnology Advances.33(8): 1582–1614.doi:10.1016/j.biotechadv.2015.08.001.PMC4748402.PMID26281720.
- ^Robson B, Baek OK (2009).The Engines of Hippocrates: From the Dawn of Medicine to Medical and Pharmaceutical Informatics.John Wiley & Sons. p. 50.ISBN9780470289532.
- ^Hong F (2004)."History of Medicine in China"(PDF).McGill Journal of Medicine.8(1): 7984. Archived fromthe original(PDF)on 1 December 2013.
- ^Unschuld P (2003).Huang Di Nei Jing: Nature, Knowledge, Imagery in an Ancient Chinese Medical Text.University of California Press. p. 286.ISBN978-0-520-92849-7.
- ^Ackerknecht E (1982).A Short History of Medicine.JHU Press. p.39.ISBN978-0-8018-2726-6.
- ^The Classical Tradition.Harvard University Press. 2010. p. 146.ISBN978-0-674-03572-0.
- ^"Traditional medicine".Archived fromthe originalon 27 July 2008.
- ^Su XZ, Miller LH (November 2015)."The discovery of artemisinin and the Nobel Prize in Physiology or Medicine".Science China Life Sciences.58(11): 1175–9.doi:10.1007/s11427-015-4948-7.PMC4966551.PMID26481135.
- ^Baggoley C (2015)."Review of the Australian Government Rebate on Natural Therapies for Private Health Insurance"(PDF).Australian Government – Department of Health. Archived fromthe original(PDF)on 26 June 2016.Retrieved12 December2015.
- ^"Assessment of clinical safety and efficacy in the preparation of Community herbal monographs for well-established and of Community herbal monographs/entries to the Community list for traditional herbal medicinal products/substances/preparations".European Medicines Agency. 2017.Archivedfrom the original on 26 February 2017.Retrieved25 February2017.
- ^"Herbs at a Glance".National Center for Complementary and Integrative Health, US National Institutes of Health. 21 November 2016.Archivedfrom the original on 30 March 2019.Retrieved24 February2017.
- ^"Clinicaltrials.gov, a registry of studies on herbal medicine".Clinicaltrials.gov, US National Institutes of Health. 2017.Archivedfrom the original on 1 April 2019.Retrieved25 February2017.
- ^Burstein HJ, Gelber S, Guadagnoli E, Weeks JC (June 1999)."Use of alternative medicine by women with early-stage breast cancer".The New England Journal of Medicine.340(22): 1733–9.doi:10.1056/NEJM199906033402206.PMID10352166.
- ^Egede LE, Ye X, Zheng D, Silverstein MD (February 2002)."The prevalence and pattern of complementary and alternative medicine use in individuals with diabetes".Diabetes Care.25(2): 324–9.doi:10.2337/diacare.25.2.324.PMID11815504.
- ^Roozbeh J, Hashempur MH, Heydari M (November 2013). "Use of herbal remedies among patients undergoing hemodialysis".Iranian Journal of Kidney Diseases.7(6): 492–5.PMID24241097.
- ^Bishop FL, Lewith GT (March 2010)."Who Uses CAM? A Narrative Review of Demographic Characteristics and Health Factors Associated with CAM Use".Evidence-Based Complementary and Alternative Medicine.7(1): 11–28.doi:10.1093/ecam/nen023.PMC2816378.PMID18955327.
- ^abSaad B, Said O (2011).Greco-Arab and Islamic Herbal Medicine: Traditional System, Ethics, Safety, Efficacy, and Regulatory Issues.John Wiley & Sons. p. 80.ISBN9780470474211.
- ^abcdGroot Handboek Geneeskrachtige Planten by Geert Verhelst
- ^Green J (2000).The Herbal Medicine Maker's Handbook: A Home Manual.Chelsea Green Publishing. p. 168.ISBN9780895949905.
- ^Romm A (2010).Botanical Medicine for Women's Health.Churchill Livingstone. p. 24.ISBN978-0-443-07277-2.
- ^Odinsson E (2010).Northern Lore: A Field Guide to the Northern Mind-Body-Spirit.Eoghan Odinsson.ISBN978-1452851433.
- ^"Aromatherapy".University of Maryland Medical Center. 2017. Archived fromthe originalon 25 October 2017.
- ^Herz RS (2009). "Aromatherapy facts and fictions: a scientific analysis of olfactory effects on mood, physiology and behavior".The International Journal of Neuroscience.119(2): 263–90.doi:10.1080/00207450802333953.PMID19125379.S2CID205422999.
- ^Gilani AH, Shah AJ, Zubair A, Khalid S, Kiani J, Ahmed A, et al. (January 2009). "Chemical composition and mechanisms underlying the spasmolytic and bronchodilatory properties of the essential oil of Nepeta cataria L".Journal of Ethnopharmacology.121(3): 405–11.doi:10.1016/j.jep.2008.11.004.PMID19041706.
- ^Gaire BP, Subedi L (March 2013). "A review on the pharmacological and toxicological aspects of Datura stramonium L".Journal of Integrative Medicine.11(2): 73–9.doi:10.3736/jintegrmed2013016.PMID23506688.
- ^Kumar P, Nandave M, Kumar A, Nandave D (2024). "Herbovigilance". In Nandave M, Kumar A (eds.).Pharmacovigilance Essentials.Springer. pp. 243–267.doi:10.1007/978-981-99-8949-2_12.ISBN978-981-99-8948-5.
- ^Talalay P, Talalay P (March 2001)."The importance of using scientific principles in the development of medicinal agents from plants".Academic Medicine.76(3): 238–47.doi:10.1097/00001888-200103000-00010.PMID11242573.
- ^abcElvin-Lewis M (May 2001). "Should we be concerned about herbal remedies".Journal of Ethnopharmacology.75(2–3): 141–64.doi:10.1016/S0378-8741(00)00394-9.PMID11297844.
- ^Vickers AJ (2007)."Which botanicals or other unconventional anticancer agents should we take to clinical trial?".Journal of the Society for Integrative Oncology.5(3): 125–9.PMC2590766.PMID17761132.
- ^Ernst E (2007). "Herbal Medicines: Balancing Benefits and Risks".Dietary Supplements and Health.Novartis Foundation Symposia. Vol. 282. pp. 154–67, discussion 167–72, 212–18.doi:10.1002/9780470319444.ch11.ISBN978-0-470-31944-4.PMID17913230.
- ^abcNewmaster SG, Grguric M, Shanmughanandhan D, Ramalingam S, Ragupathy S (October 2013)."DNA barcoding detects contamination and substitution in North American herbal products".BMC Medicine.11:222.doi:10.1186/1741-7015-11-222.PMC3851815.PMID24120035.(Retracted, seedoi:10.1186/s12916-024-03504-x,PMID38965520)
- ^Müller JL (1998). "Love potions and the ointment of witches: historical aspects of the nightshade alkaloids".Journal of Toxicology. Clinical Toxicology.36(6): 617–27.doi:10.3109/15563659809028060.PMID9776969.
- ^Lee MR (December 2006). "Solanaceae III: henbane, hags and Hawley Harvey Crippen".The Journal of the Royal College of Physicians of Edinburgh.36(4): 366–73.PMID17526134.
- ^Pinn G (November 2001). "Adverse effects associated with herbal medicine".Australian Family Physician.30(11): 1070–5.PMID11759460.
- ^Lin SH, Yang SS, Chau T, Halperin ML (March 2003). "An unusual cause of hypokalemic paralysis: chronic licorice ingestion".The American Journal of the Medical Sciences.325(3): 153–6.doi:10.1097/00000441-200303000-00008.PMID12640291.S2CID35033559.
- ^Lynch CR, Folkers ME, Hutson WR (June 2006)."Fulminant hepatic failure associated with the use of black cohosh: a case report".Liver Transplantation.12(6): 989–92.doi:10.1002/lt.20778.PMID16721764.S2CID28255622.
- ^Born D, Barron ML (May–June 2005). "Herb use in pregnancy: what nurses should know".MCN: The American Journal of Maternal/Child Nursing.30(3): 201–6, quiz 207–8.doi:10.1097/00005721-200505000-00009.PMID15867682.S2CID35882289.
- ^Boivin J, Schmidt L (July 2009)."Use of complementary and alternative medicines associated with a 30% lower ongoing pregnancy/live birth rate during 12 months of fertility treatment".Human Reproduction.24(7): 1626–31.doi:10.1093/humrep/dep077.PMID19359338.
- ^Ernst E (February 1998). "Harmless herbs? A review of the recent literature".The American Journal of Medicine.104(2): 170–8.doi:10.1016/S0002-9343(97)00397-5.PMID9528737.
- ^Izzo AA (2012)."Interactions between herbs and conventional drugs: overview of the clinical data".Medical Principles and Practice.21(5): 404–28.doi:10.1159/000334488.PMID22236736.
- ^"Herb-Drug Interactions".NCCIH.10 September 2015.Archivedfrom the original on 26 June 2019.Retrieved26 June2019.
- ^Kuhn MA (April 2002). "Herbal remedies: drug-herb interactions".Critical Care Nurse.22(2): 22–8, 30, 32, quiz 34–5.doi:10.4037/ccn2002.22.2.22.PMID11961942.
- ^Spolarich AE, Andrews L (Summer 2007)."An examination of the bleeding complications associated with herbal supplements, antiplatelet and anticoagulant medications".Journal of Dental Hygiene.81(3): 67.PMID17908423.Archivedfrom the original on 12 October 2011.Retrieved28 December2010.
- ^Nekvindová J, Anzenbacher P (July 2007). "Interactions of food and dietary supplements with drug metabolising cytochrome P450 enzymes".Ceska a Slovenska Farmacie.56(4): 165–73.PMID17969314.
- ^Cohen R (12 October 2018)."No Wonder It Works So Well: There May Be Viagra In That Herbal Supplement".NPR.org.Archivedfrom the original on 13 October 2018.Retrieved13 October2018.
- ^abCarroll L (24 February 2014)."Herbal medicines: Study raises alarm over labelling".The Sydney Morning Herald, Australia.Archivedfrom the original on 26 February 2017.Retrieved25 February2017.
- ^O'Connor A (3 February 2015)."New York Attorney General Targets Supplements at Major Retailers".The New York Times.Archivedfrom the original on 28 April 2019.Retrieved3 February2015.
- ^Kaplan S (3 February 2015)."GNC, Target, Wal-Mart, Walgreens accused of selling adulterated 'herbals'".The Washington Post.Archivedfrom the original on 24 May 2019.Retrieved3 February2015.
- ^abLin V, McCabe P, Bensoussan A, Myers S, Cohen M, Hill S, Howse G (2009)."The practice and regulatory requirements of naturopathy and western herbal medicine in Australia".Risk Management and Healthcare Policy.2:21–33.doi:10.2147/RMHP.S4652.PMC3270908.PMID22312205.
- ^"Becoming a Herbalist".The National Institute of Medical Herbalists.Archivedfrom the original on 26 June 2019.Retrieved26 June2019.
- ^"Legal and Regulatory FAQs".American Herbalist Guild.24 January 2014.Archivedfrom the original on 24 November 2020.Retrieved25 November2020.
- ^"2017 Warning Letters – Health Fraud".US Food and Drug Administration. 27 February 2017.Archivedfrom the original on 9 May 2021.Retrieved2 April2021.
- ^Porter Jr SE (25 May 2017)."Warning Letter – Herbal Doctor Remedies".U.S. Food and Drug Administration.Archivedfrom the original on 2 December 2020.Retrieved25 November2020.
- ^ab"Fraudulent Coronavirus Disease 2019 (COVID-19) Products".US Food and Drug Administration. 2 April 2021.Archivedfrom the original on 5 March 2021.Retrieved2 April2021.
- ^Bellamy J (19 November 2020)."FDA and FTC issue more warning letters citing products and services making illegal COVID claims".Science-Based Medicine.Archivedfrom the original on 14 January 2021.Retrieved2 April2021.
- ^"WHO Quality Control Methods for Herbal Materials"(PDF).World Health Organization, Geneva, Switzerland. 2011. Archived fromthe original(PDF)on 1 August 2014.
- ^"Herbal medicinal products".European Medicines Agency. 2017.Archivedfrom the original on 15 March 2017.Retrieved25 February2017.
- ^"Botanical Dietary Supplements".Office of Dietary Supplements, US National Institutes of Health. June 2011.Archivedfrom the original on 20 October 2018.Retrieved25 February2017.
- ^"US Dietary Supplement Health and Education Act of 1994".Food and Drug Administration.Archivedfrom the original on 31 May 2009.Retrieved16 December2019.
- ^Goldman P (October 2001). "Herbal medicines today and the roots of modern pharmacology".Annals of Internal Medicine.135(8 Pt 1): 594–600.doi:10.7326/0003-4819-135-8_Part_1-200110160-00010.PMID11601931.S2CID35766876.
- ^"Licensed Natural Health Products Database: What is it?".Health Canada. 8 December 2016.Archivedfrom the original on 4 June 2017.Retrieved25 February2017.
- ^FDA Issues Regulation Prohibiting Sale of Dietary Supplements Containing Ephedrine Alkaloids and Reiterates Its Advice That Consumers Stop Using These ProductsArchived15 September 2007 at theWayback Machine
- ^"WHO Traditional Medicine Strategy, 2014–2023"(PDF).World Health Organization. 2013. p. 41.Archived(PDF)from the original on 18 November 2017.Retrieved25 February2017.
- ^Zhang J, Wider B, Shang H, Li X, Ernst E (2012). "Quality of herbal medicines: challenges and solutions".Complementary Therapies in Medicine.20(1–2): 100–6.doi:10.1016/j.ctim.2011.09.004.PMID22305255.
- ^Morris CA, Avorn J (September 2003). "Internet marketing of herbal products".JAMA.290(11): 1505–9.doi:10.1001/jama.290.11.1505.PMID13129992.
- ^Coghlan ML, Haile J, Houston J, Murray DC, White NE, Moolhuijzen P, et al. (2012)."Deep sequencing of plant and animal DNA contained within traditional Chinese medicines reveals legality issues and health safety concerns".PLOS Genetics.8(4): e1002657.doi:10.1371/journal.pgen.1002657.PMC3325194.PMID22511890.
- ^Tyler VE,Robbers JE (1999).Tyler's Herbs of Choice: The Therapeutic Use of Phytomedicinals.Routledge.pp.6–8.ISBN978-0789001597.
- ^"Traditional medicine, Factsheet No. 134".World Health Organization. May 2003. Archived fromthe originalon 8 June 2003.
- ^Moerman DE (1997)."Ethnobotany in North America".InSelin, Helaine(ed.).Encyclopaedia of the History of Science, Technology, and Medicine in Non-Western Cultures.Springer. p. 321.ISBN9780792340669.
- ^Bussmann RW, Sharon D (November 2006)."Traditional medicinal plant use in Northern Peru: tracking two thousand years of healing culture".Journal of Ethnobiology and Ethnomedicine.2(1): 47.doi:10.1186/1746-4269-2-47.PMC1637095.PMID17090303.
- ^Yuan D, Yang X, Guo JC (May 2016)."A great honor and a huge challenge for China: You-you TU getting the Nobel Prize in Physiology or Medicine".Journal of Zhe gian g University. Science. B.17(5): 405–8.doi:10.1631/jzus.B1600094.PMC4868832.PMID27143269.
- ^Kala CP (2006)."Preserving Ayurvedic herbal formulations by Vaidyas: The traditional healers of the Uttaranchal Himalaya region in India".HerbalGram.70:42–50.Archivedfrom the original on 18 February 2020.Retrieved9 June2020.
- ^Kala CP (2005). "Health traditions of Buddhist community and role of amchis in trans-Himalayan region of India".Current Science.89(8): 1331–38.
- ^Kala CP (2003).Medicinal plants of Indian trans-Himalaya.Dehradun: Bishen Singh Mahendra Pal Singh. p. 200.
- ^Petrovska BB (January 2012)."Historical review of medicinal plants' usage".Pharmacognosy Reviews.6(11): 1–5.doi:10.4103/0973-7847.95849.PMC3358962.PMID22654398.
- ^Wahono T (21 February 2012)."Jejak Mataram Kuno di Sindoro"[Traces of Ancient Mataram in Sindoro].KOMPAS(in Indonesian).Archivedfrom the original on 9 June 2020.Retrieved9 June2020.
- ^abc"Jamu dan Lulur, Rahasia Cantik Para Putri Keraton".Tribun Jogja(in Indonesian). 21 May 2013.Archivedfrom the original on 3 April 2019.Retrieved4 November2015.
- ^Society, National Geographic (20 August 2020)."Dividing Species: Wallace Line Map".National Geographic Society.Archivedfrom the original on 7 May 2022.Retrieved4 May2022.
- ^Beers SJ (2001).Jamu: The Ancient Indonesian Art of Herbal Healing.Periplus Editions (HK) Limited.ISBN978-962-593-503-4.[page needed]
- ^abVickers A, Zollman C (October 1999)."ABC of complementary medicine: herbal medicine".BMJ.319(7216): 1050–3.doi:10.1136/bmj.319.7216.1050.PMC1116847.PMID10521203.
- ^Grassmann J, Hippeli S, Elstner EF (June 2002). "Plant's defence and its benefits for animals and medicine: role of phenolics and terpenoids in avoiding oxygen stress".Plant Physiology and Biochemistry.40(6–8): 471–478.Bibcode:2002PlPB...40..471G.doi:10.1016/S0981-9428(02)01395-5.
- ^Huffman MA (May 2003)."Animal self-medication and ethno-medicine: exploration and exploitation of the medicinal properties of plants".The Proceedings of the Nutrition Society.62(2): 371–81.doi:10.1079/pns2003257.PMID14506884.
- ^Hutchings MR, Athanasiadou S, Kyriazakis I, Gordon IJ (May 2003)."Can animals use foraging behaviour to combat parasites?".The Proceedings of the Nutrition Society.62(2): 361–70.doi:10.1079/pns2003243.PMID14506883.
Further reading
[edit]- Aronson JK (2008).Meyler's Side Effects of Herbal Medicines.Elsevier.ISBN9780080932903.
- Braun L, Cohen M (2007).Herbs and Natural Supplements: An Evidence-Based Guide.Elsevier.ISBN9780729537964.


