Chlamydia
| Chlamydia | |
|---|---|
| Other names | Chlamydia infection |
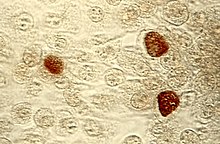
 | |
| Pap smearshowingC. trachomatis(H&E stain) | |
| Pronunciation | |
| Specialty | Infectious disease,gynecology,urology |
| Symptoms | None,vaginal discharge,discharge from the penis,burning with urination[1] |
| Complications | Pain in the testicles,pelvic inflammatory disease,infertility,ectopic pregnancy[1][2] |
| Usual onset | Few weeks following exposure[1] |
| Causes | Chlamydia trachomatisspread by sexual intercourse or childbirth[3] |
| Diagnostic method | Urine or swab of the cervix, vagina, orurethra[2] |
| Prevention | Not having sex,condoms,sex with only one non–infected person[1] |
| Treatment | Antibiotics(azithromycinordoxycycline)[2] |
| Frequency | 4.2% (women), 2.7% (men)[4][5] |
| Deaths | ~200 (2015)[6] |
Chlamydia,or more specifically achlamydia infection,is asexually transmitted infectioncaused by the bacteriumChlamydia trachomatis.[3]Most people who are infected have no symptoms.[1]When symptoms do appear they may occur only several weeks after infection;[1]theincubation periodbetween exposure and being able to infect others is thought to be on the order of two to six weeks.[7]Symptoms in women may includevaginal dischargeorburning with urination.[1]Symptoms in men may include discharge from the penis, burning with urination, orpain and swelling of one or both testicles.[1]The infection can spread to the upper genital tract in women, causingpelvic inflammatory disease,which may result in futureinfertilityorectopic pregnancy.[2]
Chlamydia infections can occur in other areas besides the genitals, including the anus, eyes, throat, and lymph nodes. Repeated chlamydia infections of the eyes that go without treatment can result intrachoma,a common cause of blindness in thedeveloping world.[8]
Chlamydia can be spread duringvaginal,anal,oral,ormanual sexand can be passed from an infected mother to her baby during childbirth.[1][9]The eye infections may also be spread by personal contact, flies, and contaminated towels in areas with poor sanitation.[8]Infection by the bacteriumChlamydia trachomatisonly occurs in humans.[10]Diagnosis is often byscreeningwhich is recommended yearly in sexually active women under the age of twenty-five, others at higher risk, and at the firstprenatal visit.[1][2]Testing can be done on the urine or a swab of the cervix, vagina, orurethra.[2]Rectal or mouth swabs are required to diagnose infections in those areas.[2]
Prevention is bynot having sex,the use ofcondoms,or having sex with only one other person, who is not infected.[1]Chlamydia can be cured byantibioticswith typically eitherazithromycinordoxycyclinebeing used.[2]Erythromycinor azithromycin is recommended in babies and during pregnancy.[2]Sexual partners should also be treated, and infected people should be advised not to have sex for seven days and until symptom free.[2]Gonorrhea,syphilis,andHIVshould be tested for in those who have been infected.[2]Following treatment people should be tested again after three months.[2]
Chlamydia is one of the most common sexually transmitted infections, affecting about 4.2% of women and 2.7% of men worldwide.[4][5]In 2015, about 61 million new cases occurred globally.[11]In the United States about 1.4 million cases were reported in 2014.[3]Infections are most common among those between the ages of 15 and 25 and are more common in women than men.[2][3]In 2015 infections resulted in about 200 deaths.[6]The wordchlamydiais from theGreekχλαμύδα,meaning 'cloak'.[12][13]
Signs and symptoms
Genital disease


Women
Chlamydial infection of thecervix(neck of the womb) is a sexually transmitted infection which hasno symptomsfor around 70% of women infected. The infection can be passed through vaginal, anal, oral, or manual sex. Of those who have an asymptomatic infection that is not detected by their doctor, approximately half will developpelvic inflammatory disease(PID), a generic term for infection of theuterus,fallopian tubes,and/orovaries.PID can cause scarring inside thereproductive organs,which can later cause serious complications, including chronicpelvicpain, difficulty becoming pregnant,ectopic (tubal) pregnancy,and other dangerous complications of pregnancy.[14]
Chlamydia is known as the "silent epidemic", as at least 70% of genitalC. trachomatisinfections in women (and 50% in men) are asymptomatic at the time of diagnosis,[15]and can linger for months or years before being discovered. Signs and symptoms may include abnormalvaginal bleedingor discharge, abdominal pain,painful sexual intercourse,fever,painful urinationor the urge to urinate more often than usual (urinary urgency).[14]
For sexually active women who are not pregnant, screening is recommended in those under 25 and others at risk of infection.[16]Risk factors include a history of chlamydial or other sexually transmitted infection, new or multiple sexual partners, and inconsistentcondomuse.[17]Guidelines recommend all women attending foremergency contraceptiveare offered chlamydia testing, with studies showing up to 9% of women aged under 25 years had chlamydia.[18]
Men
In men, those with a chlamydial infection show symptoms of infectiousinflammation of the urethrain about 50% of cases.[15]Symptoms that may occur include: a painful or burning sensation when urinating, an unusual discharge from thepenis,testicularpain or swelling, or fever. If left untreated, chlamydia in men can spread to the testicles causingepididymitis,which in rare cases can lead tosterilityif not treated.[15]Chlamydia is also a potential cause ofprostatic inflammationin men, although the exact relevance in prostatitis is difficult to ascertain due to possible contamination from urethritis.[19]
Eye disease

Trachomais a chronicconjunctivitiscaused byChlamydia trachomatis.[20]It was once the leading cause of blindness worldwide, but its role diminished from 15% of blindness cases by trachoma in 1995 to 3.6% in 2002.[21][22]The infection can be spread from eye to eye by fingers, shared towels or cloths, coughing and sneezing and eye-seeking flies.[23]Symptoms includemucopurulentocular discharge, irritation, redness, and lid swelling.[20]Newborns can also develop chlamydia eye infection through childbirth (see below). Using the SAFE strategy (acronym for surgery forin-growingorin-turnedlashes,antibiotics,facial cleanliness, and environmental improvements), theWorld Health Organizationaimed (unsuccessfully) for the global elimination of trachoma by 2020 (GET 2020 initiative).[24][25]The updated World Health Assembly neglected tropical diseases road map (2021–2030) sets 2030 as the new timeline for global elimination.[26]
Joints
Chlamydia may also causereactive arthritis—the triad of arthritis, conjunctivitis and urethral inflammation—especially in young men. About 15,000 men develop reactive arthritis due to chlamydia infection each year in the U.S., and about 5,000 are permanently affected by it. It can occur in both sexes, though is more common in men.[citation needed]
Infants
As many as half of all infants born to mothers with chlamydia will be born with the disease. Chlamydia can affect infants by causing spontaneous abortion;premature birth;conjunctivitis,which may lead to blindness; andpneumonia.[27]Conjunctivitis due to chlamydia typically occurs one week after birth (compared with chemical causes (within hours) or gonorrhea (2–5 days)).[28]
Other conditions
A differentserovarofChlamydia trachomatisis also the cause oflymphogranuloma venereum,an infection of thelymph nodesandlymphatics.It usually presents withgenital ulcerationandswollen lymph nodesin the groin, but it may also manifest asrectal inflammation,feveror swollen lymph nodes in other regions of the body.[29]
Transmission
Chlamydia can be transmitted during vaginal, anal, oral, or manual sex or direct contact with infected tissue such asconjunctiva.Chlamydia can also be passed from an infected mother to her baby during vaginal childbirth.[27]It is assumed that the probability of becoming infected is proportionate to the number of bacteria one is exposed to.[30]
Pathophysiology
Chlamydia bacteria have the ability to establish long-term associations with host cells. When an infected host cell is starved for various nutrients such asamino acids(for example,tryptophan),[31]iron,orvitamins,this has a negative consequence for chlamydia bacteria since the organism is dependent on the host cell for these nutrients. Long-term cohort studies indicate that approximately 50% of those infected clear within a year, 80% within two years, and 90% within three years.[32]
The starved chlamydia bacteria can enter a persistent growth state where they stopcell divisionand become morphologically aberrant by increasing in size.[33]Persistent organisms remain viable as they are capable of returning to a normal growth state once conditions in the host cell improve.[34]
There is debate as to whether persistence has relevance: some believe that persistent chlamydia bacteria are the cause of chronic chlamydial diseases. Some antibiotics such asβ-lactamshave been found to induce a persistent-like growth state.[35][36]
Diagnosis
The diagnosis of genital chlamydial infections evolved rapidly from the 1990s through 2006.Nucleic acid amplification tests(NAAT), such aspolymerase chain reaction(PCR), transcription mediated amplification (TMA), and the DNAstrand displacement amplification(SDA) now are the mainstays. NAAT for chlamydia may be performed on swab specimenssampledfrom the cervix (women) or urethra (men), on self-collected vaginal swabs, or on voided urine.[37]NAAT has been estimated to have asensitivityof approximately 90% and aspecificityof approximately 99%, regardless of sampling from a cervical swab or by urine specimen.[38]In women seeking treatment in a sexually transmitted infection clinic where a urine test is negative, a subsequent cervical swab has been estimated to be positive in approximately 2% of the time.[38]
At present, the NAATs have regulatory approval only for testing urogenital specimens, although rapidly evolving research indicates that they may give reliable results on rectal specimens.
Because of improved test accuracy, ease of specimen management, convenience in specimen management, and ease of screening sexually active men and women, the NAATs have largely replaced culture, the historicgold standardfor chlamydia diagnosis, and the non-amplified probe tests. The latter test is relatively insensitive, successfully detecting only 60–80% of infections in asymptomatic women, and often giving falsely-positive results. Culture remains useful in selected circumstances and is currently the only assay approved for testing non-genital specimens. Other methods also exist including:ligase chain reaction(LCR), direct fluorescent antibody resting,enzyme immunoassay,and cell culture.[39]
The swab sample for chlamydial infections does not show difference whether the sample was collected in home or in clinic in terms of numbers of patient treated. The implications in cured patients, reinfection, partner management, and safety are unknown.[40]
Rapid point-of-care tests are, as of 2020, not thought to be effective for diagnosing chlamydia in men of reproductive age and non-pregnant women because of high false-negative rates.[41]
Prevention
Prevention is bynot having sex,the use ofcondoms,or having sex with only one other person, who is not infected.[1]
Screening
For sexually active women who are not pregnant, screening is recommended in those under 25 and others at risk of infection.[16]Risk factors include a history of chlamydial or other sexually transmitted infection, new or multiple sexual partners, and inconsistentcondomuse.[17]For pregnant women, guidelines vary: screening women with age or other risk factors is recommended by theU.S. Preventive Services Task Force(USPSTF) (which recommends screening women under 25) and theAmerican Academy of Family Physicians(which recommends screening women aged 25 or younger). TheAmerican College of Obstetricians and Gynecologistsrecommends screening all at risk, while theCenters for Disease Control and Preventionrecommend universal screening of pregnant women.[16]The USPSTF acknowledges that in some communities there may be other risk factors for infection, such as ethnicity.[16]Evidence-based recommendations for screening initiation, intervals and termination are currently not possible.[16]For men, the USPSTF concludes evidence is currently insufficient to determine if regular screening of men for chlamydia is beneficial.[17]They recommend regular screening of men who are at increased risk for HIV or syphilis infection.[17]ACochrane reviewfound that the effects of screening are uncertain in terms of chlamydia transmission but that screening probably reduces the risk of pelvic inflammatory disease in women.[42]
In the United Kingdom theNational Health Service (NHS)aims to:
- Prevent and control chlamydia infection through early detection and treatment of asymptomatic infection;
- Reduce onward transmission to sexual partners;
- Prevent the consequences of untreated infection;
- Test at least 25 percent of the sexually active under 25 population annually.[43]
- Retest after treatment.[44]
Treatment
C. trachomatisinfection can be effectively cured withantibiotics.Guidelines recommendazithromycin,doxycycline,erythromycin,levofloxacin orofloxacin.[45]In men, doxycycline (100 mg twice a day for 7 days) is probably more effective than azithromycin (1 g single dose) but evidence for the relative effectiveness of antibiotics in women is very uncertain.[46]Agents recommended during pregnancy include erythromycin oramoxicillin.[2][47]
An option for treating sexual partners of those with chlamydia orgonorrheaincludespatient-delivered partner therapy(PDT or PDPT), which is the practice of treating the sex partners of index cases by providing prescriptions or medications to the patient to take to his/her partner without the health care provider first examining the partner.[48]
Following treatment people should be tested again after three months to check for reinfection.[2]Test of cure may befalse-positivedue to the limitations of NAAT in a bacterial (rather than a viral) context, since targeted genetic material may persist in the absence of viable organisms.[49]
Epidemiology
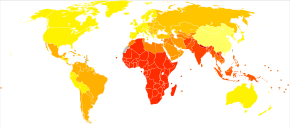
Globally, as of 2015, sexually transmitted chlamydia affects approximately 61 million people.[11]It is more common in women (3.8%) than men (2.5%).[51]In 2015 it resulted in about 200 deaths.[6]
In the United States about 1.6 million cases were reported in 2016.[52]The CDC estimates that if one includes unreported cases there are about 2.9 million each year.[52]It affects around 2% of young people.[53]Chlamydial infection is the most common bacterial sexually transmitted infection in the UK.[54]
Chlamydia causes more than 250,000 cases of epididymitis in the U.S. each year. Chlamydia causes 250,000 to 500,000 cases of PID every year in the United States. Women infected with chlamydia are up to five times more likely to become infected with HIV, if exposed.[27]
See also
References
- ^abcdefghijkl"Chlamydia – CDC Fact Sheet".CDC. May 19, 2016.Archivedfrom the original on 11 June 2016.Retrieved10 June2016.
- ^abcdefghijklmno"2015 Sexually Transmitted Diseases Treatment Guidelines".CDC. June 4, 2015.Archivedfrom the original on 11 June 2016.Retrieved10 June2016.
- ^abcd"2014 Sexually Transmitted Diseases Surveillance Chlamydia".November 17, 2015.Archivedfrom the original on 10 June 2016.Retrieved10 June2016.
- ^abNewman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N, et al. (8 December 2015)."Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting".PLOS ONE.10(12): e0143304.Bibcode:2015PLoSO..1043304N.doi:10.1371/journal.pone.0143304.PMC4672879.PMID26646541.
- ^ab"Sexually transmitted infections (STIs) Fact sheet N°110".who.int.December 2015.Archivedfrom the original on 25 November 2014.Retrieved10 June2016.
- ^abcWang H, Naghavi M, Allen C, Barber RM, Bhutta ZA, Carter A, et al. (October 2016)."Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015".Lancet.388(10053): 1459–1544.doi:10.1016/s0140-6736(16)31012-1.PMC5388903.PMID27733281.
- ^Shors T (2018).Krasner's Microbial Challenge.p. 366.
- ^ab"CDC – Trachoma, Hygiene-related Diseases, Healthy Water".Centers for Disease Control and Prevention. December 28, 2009.Archivedfrom the original on September 5, 2015.Retrieved2015-07-24.
- ^Hoyle A, McGeeney E (2019).Great Relationships and Sex Education.Taylor and Francis.ISBN978-1-35118-825-8.RetrievedJuly 11,2023.
- ^Graeter L (2014).Elsevier's Medical Laboratory Science Examination Review.Elsevier Health Sciences. p. 30.ISBN9780323292412.Archivedfrom the original on 2017-09-10.
- ^abVos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (October 2016)."Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015".Lancet.388(10053): 1545–1602.doi:10.1016/S0140-6736(16)31678-6.PMC5055577.PMID27733282.
- ^Stevenson A (2010).Oxford dictionary of English(3rd ed.). New York, NY: Oxford University Press. p. 306.ISBN9780199571123.Archivedfrom the original on 10 September 2017.Retrieved10 June2016.
- ^Byrne GI (July 2003)."Chlamydia uncloaked".Proceedings of the National Academy of Sciences of the United States of America.100(14): 8040–8042.Bibcode:2003PNAS..100.8040B.doi:10.1073/pnas.1533181100.PMC166176.PMID12835422.
The term was coined based on the incorrect conclusion that Chlamydia are intracellular protozoan pathogens that appear to cloak the nucleus of infected cells.
- ^abWitkin SS, Minis E, Athanasiou A, Leizer J, Linhares IM (October 2017)."Chlamydia trachomatis: the Persistent Pathogen".Clinical and Vaccine Immunology.24(10).doi:10.1128/CVI.00203-17.PMC5629669.PMID28835360.
- ^abcNHS Chlamydia pageArchived2013-01-16 at theWayback Machine
- ^abcdeMeyers D, Wolff T, Gregory K, Marion L, Moyer V, Nelson H, et al. (March 2008)."USPSTF recommendations for STI screening".American Family Physician.77(6): 819–824.PMID18386598.Archived fromthe originalon 2021-08-28.Retrieved2008-03-17.
- ^abcdU.S. Preventive Services Task Force (July 2007)."Screening for chlamydial infection: U.S. Preventive Services Task Force recommendation statement".Annals of Internal Medicine.147(2): 128–134.doi:10.7326/0003-4819-147-2-200707170-00172.PMID17576996.S2CID35816540.Archivedfrom the original on 2008-03-03.
- ^Yeung EY, Comben E, McGarry C, Warrington R (February 2015)."STI testing in emergency contraceptive consultations".The British Journal of General Practice.65(631): 63.1–64.doi:10.3399/bjgp15X683449.PMC4325454.PMID25624285.
- ^Wagenlehner FM, Naber KG, Weidner W (April 2006)."Chlamydial infections and prostatitis in men".BJU International.97(4): 687–690.doi:10.1111/j.1464-410X.2006.06007.x.PMID16536754.S2CID34481915.
- ^abLewis SM (2017).Medical-surgical nursing: assessment and management of clinical problems.Bucher, Linda; Heitkemper, Margaret M. (Margaret McLean); Harding, Mariann (10th ed.). St. Louis, Missouri.ISBN978-0-323-32852-4.OCLC944472408.
{{cite book}}:CS1 maint: location missing publisher (link) - ^Thylefors B, Négrel AD, Pararajasegaram R, Dadzie KY (1995)."Global data on blindness"(PDF).Bulletin of the World Health Organization.73(1): 115–121.PMC2486591.PMID7704921.Archived fromthe original(PDF)on 2008-06-25.
- ^Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. (November 2004)."Global data on visual impairment in the year 2002".Bulletin of the World Health Organization.82(11): 844–851.hdl:10665/269277.PMC2623053.PMID15640920.
- ^Mabey DC, Solomon AW, Foster A (July 2003). "Trachoma".Lancet.362(9379): 223–229.doi:10.1016/S0140-6736(03)13914-1.PMID12885486.S2CID208789262.
- ^World Health Organization.TrachomaArchived2012-10-21 at theWayback Machine.Accessed March 17, 2008.
- ^Ngondi J, Onsarigo A, Matthews F, Reacher M, Brayne C, Baba S, et al. (August 2006). "Effect of 3 years of SAFE (surgery, antibiotics, facial cleanliness, and environmental change) strategy for trachoma control in southern Sudan: a cross-sectional study".Lancet.368(9535): 589–595.doi:10.1016/S0140-6736(06)69202-7.PMID16905023.S2CID45018412.
- ^"Trachoma".who.int.Retrieved2023-06-27.
- ^abc"STD Facts – Chlamydia".Center For Disease Control. December 16, 2014.Archivedfrom the original on July 14, 2015.Retrieved2015-07-24.
- ^Hansford P (April 2010),"Palliative Care in the United Kingdom",Oxford Textbook of Palliative Nursing,Oxford University Press, pp. 1265–1274,doi:10.1093/med/9780195391343.003.0072,ISBN978-0-19-539134-3,retrieved15 December2022
- ^Williams D, Churchill D (January 2006)."Ulcerative proctitis in men who have sex with men: an emerging outbreak".BMJ.332(7533): 99–100.doi:10.1136/bmj.332.7533.99.PMC1326936.PMID16410585.
- ^Gambhir M, Basáñez MG, Turner F, Kumaresan J, Grassly NC (June 2007). "Trachoma: transmission, infection, and control".The Lancet. Infectious Diseases.7(6): 420–427.doi:10.1016/S1473-3099(07)70137-8.PMID17521595.
- ^Leonhardt RM, Lee SJ, Kavathas PB, Cresswell P (November 2007)."Severe tryptophan starvation blocks onset of conventional persistence and reduces reactivation of Chlamydia trachomatis".Infection and Immunity.75(11): 5105–5117.doi:10.1128/IAI.00668-07.PMC2168275.PMID17724071.
- ^Fairley CK, Gurrin L, Walker J, Hocking JS (September 2007).""Doctor, how long has my Chlamydia been there?" Answer: ".... years"".Sexually Transmitted Diseases.34(9): 727–728.doi:10.1097/OLQ.0b013e31812dfb6e.PMID17717486.
- ^Mpiga P, Ravaoarinoro M (2006). "Chlamydia trachomatis persistence: an update".Microbiological Research.161(1): 9–19.doi:10.1016/j.micres.2005.04.004.PMID16338585.
- ^Kushwaha AK (2020-07-26).Textbook of Microbiology.Dr. A.K KUSHWAHA.
- ^Bayramova F, Jacquier N, Greub G (2018)."Insight in the biology of Chlamydia-related bacteria".Microbes and Infection.20(7–8). Elsevier: 432–440.doi:10.1016/j.micinf.2017.11.008.PMID29269129.
- ^Klöckner A, Bühl H, Viollier P, Henrichfreise B (2018). "Deconstructing the Chlamydial Cell Wall". In Häcker, Georg (ed.).Biology of Chlamydia.Current Topics in Microbiology and Immunology. Vol. 412. Cham: Springer International Publishing. pp. 1–33.doi:10.1007/82_2016_34.ISBN978-3-319-71232-1.PMID27726004.
- ^Gaydos CA, Theodore M, Dalesio N, Wood BJ, Quinn TC (July 2004)."Comparison of three nucleic acid amplification tests for detection of Chlamydia trachomatis in urine specimens".Journal of Clinical Microbiology.42(7): 3041–3045.CiteSeerX10.1.1.335.7713.doi:10.1128/JCM.42.7.3041-3045.2004.PMC446239.PMID15243057.
- ^abHaugland S, Thune T, Fosse B, Wentzel-Larsen T, Hjelmevoll SO, Myrmel H (March 2010)."Comparing urine samples and cervical swabs for Chlamydia testing in a female population by means of Strand Displacement Assay (SDA)".BMC Women's Health.10(1): 9.doi:10.1186/1472-6874-10-9.PMC2861009.PMID20338058.
- ^"Recommendations for the Laboratory-Based Detection of Chlamydia trachomatis and Neisseria gonorrhoeae — 2014".Centers for Disease Control and Prevention.Archivedfrom the original on 2016-06-27.Retrieved2016-06-12.
- ^Fajardo-Bernal L, Aponte-Gonzalez J, Vigil P, Angel-Müller E, Rincon C, Gaitán HG, et al. (Cochrane STI Group) (September 2015)."Home-based versus clinic-based specimen collection in the management of Chlamydia trachomatis and Neisseria gonorrhoeae infections".The Cochrane Database of Systematic Reviews.2015(9): CD011317.doi:10.1002/14651858.CD011317.pub2.PMC8666088.PMID26418128.
- ^Grillo-Ardila CF, Torres M, Gaitán HG (January 2020)."Rapid point of care test for detecting urogenital Chlamydia trachomatis infection in nonpregnant women and men at reproductive age".The Cochrane Database of Systematic Reviews.1(1): CD011708.doi:10.1002/14651858.CD011708.pub2.PMC6988850.PMID31995238.
- ^Low N, Redmond S, Uusküla A, van Bergen J, Ward H, Andersen B, et al. (September 2016)."Screening for genital chlamydia infection".The Cochrane Database of Systematic Reviews.2016(9): CD010866.doi:10.1002/14651858.CD010866.pub2.PMC6457643.PMID27623210.
- ^"National Chlamydia Screening Programme Data tables".chlamydiascreening.nhs.uk.Archived fromthe originalon 2009-05-04.Retrieved2009-08-28.
- ^Desai M, Woodhall SC, Nardone A, Burns F, Mercey D, Gilson R (August 2015)."Active recall to increase HIV and STI testing: a systematic review".Sexually Transmitted Infections.91(5): 314–323.doi:10.1136/sextrans-2014-051930.PMID25759476.
Strategies for improved follow up care include the use of text messages and emails from those who provided treatment.
- ^Eliopoulos GM, Gilbert DN, Moellering RC, eds. (2015).The Sanford guide to antimicrobial therapy 2011.Sperryville, VA: Antimicrobial Therapy, Inc. pp.20.ISBN978-1-930808-65-2.
- ^Páez-Canro C, Alzate JP, González LM, Rubio-Romero JA, Lethaby A, Gaitán HG (January 2019)."Antibiotics for treating urogenital Chlamydia trachomatis infection in men and non-pregnant women".The Cochrane Database of Systematic Reviews.1(1): CD010871.doi:10.1002/14651858.CD010871.pub2.PMC6353232.PMID30682211.
- ^Miller KE (April 2006)."Diagnosis and treatment of Chlamydia trachomatis infection".American Family Physician.73(8): 1411–1416.PMID16669564.Archivedfrom the original on November 27, 2011.Retrieved2010-10-30.
- ^Expedited Partner Therapy in the Management of Sexually Transmitted Diseases (2 February 2006)Archived29 July 2017 at theWayback MachineU.S. Department of Health and Human Services Public Health Service. Centers for Disease Control and Prevention National Center for HIV, STD, and TB Prevention
- ^Dukers-Muijrers N, Morré S, Speksnijder A, Sande M, Hoebe C (28 March 2012)."Chlamydia trachomatisTest-of-Cure Cannot Be Based on a Single Highly Sensitive Laboratory Test Taken at Least 3 Weeks after Treatment ".PLOS ONE.7(3): e34108.Bibcode:2012PLoSO...734108D.doi:10.1371/journal.pone.0034108.PMC3314698.PMID22470526.
- ^"WHO Disease and injury country estimates".World Health Organization.2004.Archivedfrom the original on 2009-11-11.RetrievedNov 11,2009.
- ^Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. (December 2012)."Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010".Lancet.380(9859): 2163–2196.doi:10.1016/S0140-6736(12)61729-2.PMC6350784.PMID23245607.
- ^ab"Detailed STD Facts – Chlamydia".Centers for Disease Control and Prevention.20 September 2017.Retrieved14 January2018.
- ^Torrone E, Papp J, Weinstock H (September 2014)."Prevalence of Chlamydia trachomatis genital infection among persons aged 14-39 years--United States, 2007-2012".MMWR. Morbidity and Mortality Weekly Report.63(38): 834–838.PMC4584673.PMID25254560.
- ^"Chlamydia".UK Health Protection Agency. Archived fromthe originalon 13 September 2012.Retrieved31 August2012.
