Colitis
| Colitis | |
|---|---|
 | |
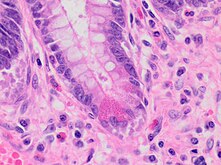
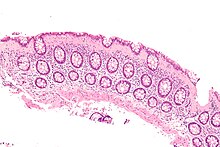
| Amicrographdemonstratingcryptitis,amicroscopiccorrelate of colitis.H&E stain. | |
| Specialty | Gastroenterology |
Colitisis swelling orinflammationof the large intestine (colon).[1]Colitis may beacuteand self-limited orlong-term.It broadly fits into the category ofdigestive diseases.
In a medical context, the labelcolitis(without qualification) is used if:
- The cause of the inflammation in the colon is undetermined; for example,colitismay be applied toCrohn's diseaseat a time when thediagnosisis unknown, or
- The context is clear; for example, an individual withulcerative colitisis talking about their disease with a physician who knows thediagnosis.
Signs and symptoms
[edit]Thesignsandsymptomsof colitis are quite variable and dependent on the cause of the given colitis and factors that modify its course and severity.[2]
Common symptoms of colitis may include: mild to severeabdominal painsandtenderness(depending on the stage of the disease), persistenthemorrhagicdiarrheawith pus either present or absent in thestools,fecal incontinence,flatulence,fatigue,loss of appetiteand unexplainedweight loss.[3]
More severe symptoms may include:shortness of breath,a fast orirregular heartbeatandfever.[3]
Other less common or rarenon-specific symptomsthat may accompany colitis include:arthritis,mouth ulcers,painful, red and swollen skin and irritated,bloodshot eyes.[3]
Signs seen oncolonoscopyinclude: colonic mucosalerythema(redness of the colon's inner surface),ulcerationsandhemorrhage.[4]
Diagnosis
[edit]Symptoms suggestive of colitis are worked-up by obtaining themedical history,a physical examination and laboratory tests (CBC,electrolytes,stool culture and sensitivity, stool ova and parasites et cetera). Additional tests may include medical imaging (e.g. abdominalcomputed tomography,abdominal X-rays) and an examination with a camera inserted into the rectum (sigmoidoscopy,colonoscopy).[5]
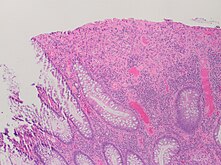
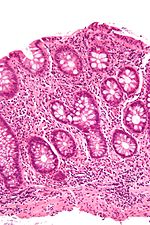
An important investigation in the assessment of colitis is biopsy forhistopathology.A very small piece of tissue (usually about 2mm) is removed from the bowel mucosa during endoscopy and examined under the microscope by a histopathologist. A biopsy report generally does not state the diagnosis, but should state any presence of chronic colitis, give an indication of disease activity, as well as state the presence of any epithelial damage (erosions and ulcerations).[6]
Histopathology findings generally associated with chronic colitis include:[6]
-
Crypt degeneration
-
Crypt branching and other architectural distortions
-
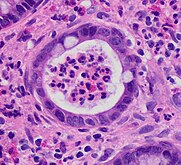
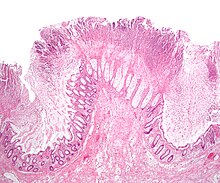
Paneth cell(pictured) or gastric metaplasia (only applies in the left colon and rectum)
Other findings include basal plasmacytosis and mucin depletion.[6] Histopathology findings generally associated with active colitis include:[6]
-
Neutrophilic cryptitis (neutrophils within crypt epithelium)
-
Crypt abscesses (luminal neutrophilic aggregates)
-
Gland destruction
-
Ulceration (seen here as absence of epithelium, and granulation tissue with many fibroblasts)
Types
[edit]There are many types of colitis. They are usually classified by the cause.
Types of colitis include:
Autoimmune
[edit]- Inflammatory bowel disease(IBD) – a group of chronic colitides.
- Ulcerative colitis(UC) – a chronic colitis that affects the large intestine.[7]
- Crohn's disease(CD) – another type of IBD that often leads to colitis.
Unknown
[edit]- Microscopic colitis– a colitis diagnosed bymicroscopicexamination of colonic tissue; macroscopically ( "to the eye" ) it appears normal.
Treatment-caused
[edit]- Diversion colitis
- Chemical colitis
- Chemotherapy-induced colitis
- Radiation colitis
- Checkpoint inhibitor induced colitis
Vascular disease
[edit]Infectious
[edit]
- Infectious colitis
A subtype of infectious colitis isClostridioides difficilecolitis,[8]which is informally abbreviated as "C-diff colitis". It classically formspseudomembranesand is often referred to as pseudomembranous colitis, which is its (nonspecific)histomorphologicdescription.
Enterohemorrhagiccolitis may be caused byShiga toxininShigella dysenteriaeorShigatoxigenic groupofEscherichia coli(STEC), which includesserotypeO157:H7and other enterohemorrhagicE. coli.[9]
Parasiticinfections, like those caused byEntamoeba histolytica,can also cause colitis.
Unclassifiable colitides
[edit]Indeterminate colitisis the classification for colitis that has features of bothCrohn's diseaseandulcerative colitis.[10]Indeterminate colitis' behaviour is usually closer to ulcerative colitis than Crohn's disease.[11]
Treatment
[edit]Treatment for this condition can include medications such as steroids and dietary changes. In some instances, hospitalization and surgery may be required.[12]
Moreover, several studies recently have found significant relationship between colitis anddairy allergy(including: cow milk, cow milk UHT and casein),[13][14][15]suggesting some patients may benefit from anelimination diet.
Microbiome modification
[edit]The use of oralprobioticsupplements to modify the composition and behavior of the microbiome has been considered as a possible therapy for both induction and maintenance of remission in people with Crohn's disease and ulcerative colitis. A Cochrane review in 2020 did not find clear evidence of improved remission likelihood, nor lower adverse events, in people with Crohn's disease, following probiotic treatment.[16]
For ulcerative colitis, there is low-certainty evidence that probiotic supplements may increase the probability of clinical remission.[17]People receiving probiotics were 73% more likely to experience disease remission and over 2x as likely to report improvement in symptoms compared to those receiving a placebo, with no clear difference in minor or serious adverse effects.[17]Although there was no clear evidence of greater remission when probiotic supplements were compared with5‐aminosalicylic acidtreatment as amonotherapy,the likelihood of remission was 22% higher if probiotics were used in combination with 5-aminosalicylic acid therapy.[17]Whereas in people who are already in remission, it is unclear whether probiotics help to prevent future relapse, either as a monotherapy orcombination therapy.[18]
Research
[edit]One study reported successfully treating experimental colitis in mice withmesenchymal stem cells.[19]
Additional research was conducted by Huanget al.that analyzed specific genes and biological markers that are associated with the risk of colon cancer development in patients with colitis. The results showed a correlation between certain biomarkers and the development of disease.[20]
Colitis is common in parts of the world wherehelminthiccolonisation is rare, and uncommon in those areas where most people carry worms.Infectionswith helminths may alter the autoimmune response that causes the disease. Early trials ofTrichuris suisova (TSO) showed promising results when used in people with IBD[21][22][23][24]but later trials failed at Phase 2, and most were eventually discontinued.[25]However, the phase 2 trials had used a different formulation of TSO from the one that had been used in the earlier studies that had shown positive outcomes.[26]
References
[edit]- ^"Colitis".pennmedicine.org.July 1, 2021.Retrieved2022-11-18.
- ^"Ulcerative colitis - Symptoms and causes".Mayo Clinic.Retrieved2024-04-11.
- ^abcNHS Choices."Ulcerative colitis - Symptoms - NHS Choices".nhs.uk.Retrieved2015-11-03.
- ^"Colonoscopy for ulcerative colitis: Why to get one, prep, and more".30 July 2021.
- ^"Diagnosis of Ulcerative Colitis | NIDDK".National Institute of Diabetes and Digestive and Kidney Diseases.Retrieved2022-11-18.
- ^abcdKellermann L, Riis LB. (2021)."A close view on histopathological changes in inflammatory bowel disease, a narrative review".Dig Med Res.4(3): 3.doi:10.21037/dmr-21-1.
- ^Elghobashy M, Steed H (2024)."Ulcerative colitis".Medicine.52(4): 232–237.doi:10.1016/j.mpmed.2024.01.001.ISSN1357-3039.
- ^"Clostridium Difficile Colitis – Overview".WebMD, LLC.Retrieved2006-09-15.
- ^Beutin L (September 2006). "Emerging enterohaemorrhagic Escherichia coli, causes and effects of the rise of a human pathogen".Journal of Veterinary Medicine. B, Infectious Diseases and Veterinary Public Health.53(7): 299–305.doi:10.1111/j.1439-0450.2006.00968.x.PMID16930272.
- ^Romano C, Famiani A, Gallizzi R, Comito D, Ferrau' V, Rossi P (December 2008). "Indeterminate colitis: a distinctive clinical pattern of inflammatory bowel disease in children".Pediatrics.122(6): e1278–e1281.doi:10.1542/peds.2008-2306.PMID19047226.S2CID1409823.
- ^Melton GB, Kiran RP, Fazio VW, He J, Shen B, Goldblum JR, et al. (October 2010). "Do preoperative factors predict subsequent diagnosis of Crohn's disease after ileal pouch-anal anastomosis for ulcerative or indeterminate colitis?".Colorectal Disease.12(10): 1026–1032.doi:10.1111/j.1463-1318.2009.02014.x.PMID19624520.S2CID44406331.
- ^"Treatment for Ulcerative Colitis - NIDDK".National Institute of Diabetes and Digestive and Kidney Diseases.Retrieved2024-04-20.
- ^Yang M, Geng L, Chen P, Wang F, Xu Z, Liang C, et al. (March 2015)."Effectiveness of dietary allergen exclusion therapy on eosinophilic colitis in Chinese infants and young children ≤ 3 years of age".Nutrients.7(3): 1817–1827.doi:10.3390/nu7031817.PMC4377883.PMID25768952.
- ^Lucendo AJ, Serrano-Montalbán B, Arias Á, Redondo O, Tenias JM (July 2015)."Efficacy of Dietary Treatment for Inducing Disease Remission in Eosinophilic Gastroenteritis".Journal of Pediatric Gastroenterology and Nutrition.61(1): 56–64.doi:10.1097/MPG.0000000000000766.PMID25699593.S2CID26195645.
- ^Sun J, Lin J, Parashette K, Zhang J, Fan R (February 2015). "Association of lymphocytic colitis and lactase deficiency in pediatric population".Pathology, Research and Practice.211(2): 138–144.doi:10.1016/j.prp.2014.11.009.PMID25523228.
- ^Limketkai BN, Akobeng AK, Gordon M, Adepoju AA (2020-07-17). Cochrane Gut Group (ed.)."Probiotics for induction of remission in Crohn's disease".Cochrane Database of Systematic Reviews.2020(7): CD006634.doi:10.1002/14651858.CD006634.pub3.PMC7389339.PMID32678465.
- ^abcKaur L, Gordon M, Baines PA, Iheozor-Ejiofor Z, Sinopoulou V, Akobeng AK (2020-03-04). Cochrane IBD Group (ed.)."Probiotics for induction of remission in ulcerative colitis".Cochrane Database of Systematic Reviews.3(3): CD005573.doi:10.1002/14651858.CD005573.pub3.PMC7059959.PMID32128795.
- ^Iheozor-Ejiofor Z, Kaur L, Gordon M, Baines PA, Sinopoulou V, Akobeng AK (2020-03-04). Cochrane IBD Group (ed.)."Probiotics for maintenance of remission in ulcerative colitis".Cochrane Database of Systematic Reviews.3(3): CD007443.doi:10.1002/14651858.CD007443.pub3.PMC7059960.PMID32128794.
- ^Yang F, Ni B, Liu Q, He F, Li L, Zhong X, et al. (September 2022)."Human umbilical cord-derived mesenchymal stem cells ameliorate experimental colitis by normalizing the gut microbiota".Stem Cell Research & Therapy.13(1): 475.doi:10.1186/s13287-022-03118-1.PMC9476645.PMID36104756.
- ^Huang Y, Zhang X, Li Y, Yao J (June 2022)."Identification of hub genes and pathways in colitis-associated colon cancer by integrated bioinformatic analysis".BMC Genomic Data.23(1): 48.doi:10.1186/s12863-022-01065-7.PMC9219145.PMID35733095.
- ^Summers RW, Elliott DE, Urban JF, Thompson RA, Weinstock JV (2005)."Trichuris suis therapy for active ulcerative colitis: a randomized controlled trial".Gastroenterology.128(4): 825–32.doi:10.1053/j.gastro.2005.01.005.PMID15825065.
- ^Pommerville J (2014).Fundamentals of microbiology.Burlington, MA: Jones & Bartlett Learning.ISBN978-1-4496-8861-5.
- ^Elliott DE, Weinstock JV (November 2012)."Where are we on worms?".Current Opinion in Gastroenterology.28(6): 551–6.doi:10.1097/MOG.0b013e3283572f73.PMC3744105.PMID23079675.
- ^Weinstock JV, Elliott DE (March 2013)."Translatability of helminth therapy in inflammatory bowel diseases".International Journal for Parasitology.43(3–4): 245–51.doi:10.1016/j.ijpara.2012.10.016.PMC3683647.PMID23178819.
Early clinical trials suggested that exposure to helminths such as Trichuris suis or Necator americanus can improve IBD.
- ^Coronado Biosciences (November 7, 2013)."Coronado Biosciences Announces Independent Data Monitoring Committee Recommendation to Discontinue Falk Phase 2 Trial of TSO in Crohn's Disease".Archived fromthe originalon August 16, 2016.RetrievedAugust 16,2016.
- ^Parker W (December 2017). "Not infection with parasitic worms, but rather colonization with therapeutic helminths".Immunology Letters.196:104–105.doi:10.1016/j.imlet.2017.07.008.PMID28720335.