Fascia of Scarpa
| Fascia of Scarpa | |
|---|---|
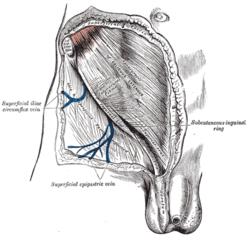 The subcutaneous inguinal ring. (Superficial fascia visible at top.) | |
| Details | |
| Identifiers | |
| Latin | stratum membranosumtelae subcutaneae abdominis |
| TA98 | A04.5.02.022 |
| TA2 | 7093 |
| FMA | 72080 |
| Anatomical terminology | |
Thefascia of Scarpais the deepmembranous layer(stratum membranosum)of thesuperficial fasciaof the abdomen. It is alayer of the anterior abdominal wall.It is founddeepto thefascia of Camperandsuperficialto theexternal oblique muscle.
Structure[edit]
It is thinner and more membranous in character than the superficialfascia of Camper,and contains a considerable quantity of orange elastic fibers.
It is loosely connected by areolar tissue to the aponeurosis of theexternal oblique muscle,but in the midline it is more intimately adherent to thelinea albaand thepubic symphysis,and in the male, it is prolonged on to the dorsum of thepenis,forming thefundiform ligament;above, it is continuous with thesuperficial fasciaover the rest of thetrunk;inferiorly, it is continuous with thefascia of Collesof theperineum;however, it does not extend into the thigh as it just attaches to its fascia, which is known asfascia lata;medially and below, it is continued over the penis andspermatic cordto thescrotum,where it helps to form thedartos.
From the scrotum, it may be traced backward into continuity with the deep layer of the superficialfascia of the perineum(superficial perineal fascia or fascia of Colles).
In the female, it is continued into thelabia majoraand from there to the fascia of Colles. The Scarpa's fascia also thickens into a collagenous structure called the fundiform ligament of theclitoris.[1]
History[edit]
It is named for Italian anatomistAntonio Scarpa.[2]His description of the membranous superficial fascia is vague in his 1809 hernia monograph.[3]Life-size illustrations included by Scarpa do not identify the layer even though some show all the other anatomical layers of the abdominal wall in the inguinal region. A probable description of the fascia is in the text which discusses femoral (called crural) hernia in the male. Scarpa describes that "below the skin" we find "a layer of condensed substance forming the second covering of the hernia" which adheres to "the aponeurosis of the fascia lata". A little later he describes this layer as being membranous and he believes it has a role in containing this particular herniation. In 1810,Abraham Collesdescribed detailed methods of dissection to expose membranous superficial fascia in the lower abdomen and the inguino-perineal region including the penis and scrotum. Colles clearly associated the subcutaneous limitation of urine extravasation from a ruptured urethra with the attachments of the membranous superficial fascia to deeper structures.[4]
Clinical significance[edit]
Scarpa's belief that the fascia stops hernias from forming is not thought to be true today. Some anatomists suggest the membranous superficial fascia is the scaffold which attaches the skin to the deeper structures so that the skin does not sag with gravity but still stretches as the body flexes or changes shape with exercise.[4]The attachment of the fascia to deeper layers confines fluid which may have come from inside the body in certain diseases giving rise toclinical signssuch as urethral disruption noticed byCollesand bruising inCullen's signorGrey Turner's sign.[4]
References[edit]
![]() This article incorporates text in thepublic domainfrompage 408of the 20th edition ofGray's Anatomy(1918)
This article incorporates text in thepublic domainfrompage 408of the 20th edition ofGray's Anatomy(1918)
- ^Di Giuseppe, Alberto; Shiffman, Melvin A. (2015).Aesthetic Plastic Surgery of the Abdomen.Springer International Publishing. p. 23.ISBN978-3-31920-004-0.
- ^synd/2925atWho Named It?
- ^A. Scarpa. Sull' ernie: memorie anatomico-chirurgiche. Milano, d. reale Stamperia, 1809; 2nd edition, 1820.
- ^abcUllah, S. M.; Grant, R. C.; Johnson, M; McAlister, V. C. (2013)."Scarpa's fascia and clinical signs: The role of the membranous superficial fascia in the eponymous clinical signs of retroperitoneal catastrophe".Annals of the Royal College of Surgeons of England.95(7): 519–22.doi:10.1308/003588413X13629960048514.PMC5827285.PMID24112501.
