Neurodevelopmental disorder
This article has multiple issues.Please helpimprove itor discuss these issues on thetalk page.(Learn how and when to remove these template messages)
|
| Neurodevelopmental disorder | |
|---|---|
| Specialty | Psychiatry,neurology |
Neurodevelopmental disordersare a group of conditions that begin to emerge during childhood (or thedevelopment of the nervous system). According to theAmerican Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders, Fifth Edition, (DSM-5) published in 2013, these conditions generally appear inearlychildhood, usually before children start school, and can persist into adulthood.[1]The key characteristic of all these disorders is that they negatively impact a person's functioning in one or more domains of life (personal, social, academic, occupational) depending on the disorder and deficits it has caused. All of these disorders and their levels of impairment exist on a spectrum, and affected individuals can experience varying degrees of symptoms and deficits, despite having the same diagnosis.[1][2]
The DSM-5 classifies neurodevelopmental disorders into six overarching groups.
- Intellectual disability(intellectual development disorder)
- Communication disorders
- Autism spectrum disorder(ASD)
- Attention-deficit/hyperactivity disorder(ADHD)
- Neurodevelopmentalmotor disorders
- Specific learning disorders
These disorders are commonly comorbid conditions, meaning that a person affected by one of these disorders will usually meet criteria for a second disorder.[1][2]
Classification[edit]
Intellectual disability (intellectual development disorder)[edit]
Intellectual disabilities (IDs),or intellectual development disorder, are defined by the DSM-5 as "deficits in general mental abilities".[1]They affect a person's ability to process information, learn or retain information, think critically or abstractly, and solve problems.[1]They ultimately inhibit a person's ability to adapt to their surroundings, to the extent that individuals may fail to meet milestones of independent functioning or social responsibility in one or more activities of daily living.[1]Global developmental delay(GDD) is categorized under intellectual disability and "is diagnosed when an individual fails to meet expected developmental milestones in several areas of intellectual functioning."[1]
Communication disorders[edit]
Autism spectrum disorder (ASD)[edit]
Attention-deficit/hyperactivity disorder (ADHD)[edit]
Attention deficit hyperactivity disorder(ADHD)
Neurodevelopmental motor disorders[edit]
Motor disordersincludingdevelopmental coordination disorder,stereotypic movement disorder,andtic disorders(such asTourette's syndrome), and CAS -Apraxia of speech
Specific learning disorders[edit]
Currently being researched[edit]
There areneurodevelopmentalresearch projects examining potential new classifications of disorders including:
- Nonverbal learning disorder(NLD or NVLD), a neurodevelopmental disorder thought to be linked to white matter in the right hemisphere of the brain and generally considered to include (a) low visuospatial intelligence; (b) discrepancy between verbal and visuospatial intelligence; (c) visuoconstructive and fine-motor coordination skills; (d) visuospatial memory tasks; (e) reading better than mathematical achievement; and (f) socioemotional skills.[3][4][5]While Nonverbal learning disorder is not categorized in the ICD or DSM as an discrete classification, "the majority of researchers and clinicians agree that the profile of NLD clearly exists (but see Spreen, 2011, for an exception[6]), but they disagree on the need for a specific clinical category and on the criteria for its identification. "[7]
Presentation[edit]
Consequences[edit]
The multitude of neurodevelopmental disorders span a wide range of associated symptoms and severity, resulting in different degrees of mental, emotional, physical, and economic consequences for individuals, and in turn families, social groups, and society.[8]
Causes[edit]
Thedevelopment of the nervous systemis tightly regulated and timed; it is influenced by both genetic programs and the prenatal environment. Any significant deviation from the normal developmental trajectory early in life can result in missing or abnormal neuronal architecture or connectivity.[9]Because of the temporal and spatial complexity of the developmental trajectory, there are many potential causes of neurodevelopmental disorders that may affect different areas of the nervous system at different times and ages. These range from social deprivation,geneticandmetabolic diseases,immune disorders,infectious diseases,nutritionalfactors,physical trauma,and toxic and prenatal environmental factors. Some neurodevelopmental disorders, such asautismand otherpervasive developmental disorders,are considered multifactorialsyndromeswhich have many causes that converge to a more specific neurodevelopmental manifestation.[10]Some deficits may be predicted from observed deviations in the maturation patterns of the infant gutmicrobiome.[11]
Social deprivation[edit]
Deprivation from social and emotional care causes severe delays in brain and cognitive development.[12]Studies with children growing up in Romanian orphanages duringNicolae Ceauşescu's regime reveal profound effects ofsocial deprivationandlanguage deprivationon the developing brain. These effects are time-dependent. The longer children stayed in negligent institutional care, the greater the consequences. By contrast, adoption at an early age mitigated some of the effects of earlierinstitutionalization (abnormal psychology).[13]
Genetic disorders[edit]

A prominent example of a genetically determined neurodevelopmental disorder isTrisomy21, also known asDown syndrome.This disorder usually results from an extrachromosome 21,[14]although in uncommon instances it is related to otherchromosomal abnormalitiessuch astranslocationof the genetic material. It is characterized by shortstature,epicanthal (eyelid) folds, abnormalfingerprints,andpalm prints,heart defects,poormuscle tone(delay of neurological development), andintellectual disabilities(delay of intellectual development).[15]
Less commonly known genetically determined neurodevelopmental disorders includeFragile X syndrome.Fragile X syndrome was first described in 1943 by Martin and Bell, studying persons with family history ofsex-linked"mental defects".[16]Rett syndrome,another X-linked disorder, produces severe functional limitations.[17]Williams syndromeis caused by small deletions of genetic material fromchromosome 7.[18] The most common recurrent Copy Number Variant disorder is22q11.2 deletion syndrome(formerly DiGeorge or velocardiofacial syndrome), followed byPrader-Willi syndromeandAngelman syndrome.[19]
Immune dysfunction[edit]
Immune reactions duringpregnancy,both maternal and of the developing child, may produce neurodevelopmental disorders. One typical immune reaction in infants and children isPANDAS,[20]orPediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infection.[21]Another disorder isSydenham's chorea,which results in more abnormal movements of the body and fewer psychological sequellae. Both are immune reactions against brain tissue that follow infection byStreptococcusbacteria. Susceptibility to these immune diseases may be genetically determined,[22]so sometimes several family members may have one or both of them following anepidemicof Strep infection.[citation needed]
Infectious diseases[edit]
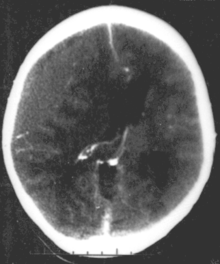
Systemic infections can result in neurodevelopmental consequences, when they occur in infancy and childhood of humans, but would not be called a primary neurodevelopmental disorder. For exampleHIV[23]Infections of the head and brain, likebrain abscesses,meningitisorencephalitishave a high risk of causing neurodevelopmental problems and eventually a disorder. For example,measlescan progress tosubacute sclerosing panencephalitis.
A number ofinfectious diseasescan be transmitted congenitally (either before or at birth), and can cause serious neurodevelopmental problems, as for example the virusesHSV,CMV,rubella (congenital rubella syndrome),Zika virus,or bacteria likeTreponema pallidumincongenital syphilis,which may progress toneurosyphilisif it remains untreated. Protozoa likePlasmodium[23]orToxoplasmawhich can cause congenitaltoxoplasmosiswith multiple cysts in the brain and other organs, leading to a variety of neurological deficits.
Some cases ofschizophreniamay be related to congenital infections, though the majority are of unknown causes.[24]
Metabolic disorders[edit]
Metabolic disordersin either the mother or the child can cause neurodevelopmental disorders. Two examples arediabetes mellitus(amultifactorial disorder) andphenylketonuria(aninborn error of metabolism). Many such inherited diseases may directly affect the child'smetabolismand neural development[25]but less commonly they can indirectly affect the child duringgestation.(See alsoteratology).
In a child,type 1 diabetescan produce neurodevelopmental damage by the effects of excess or insufficientglucose.The problems continue and may worsen throughout childhood if the diabetes is not well controlled.[26]Type 2 diabetesmay be preceded in its onset by impaired cognitive functioning.[27]
A non-diabeticfetuscan also be subjected to glucose effects if its mother has undetectedgestational diabetes.Maternal diabetes causes excessive birth size, making it harder for the infant to pass through the birth canal without injury or it can directly produce early neurodevelopmental deficits. Usually the neurodevelopmental symptoms will decrease in later childhood.[28]
Phenylketonuria,also known as PKU, can induce neurodevelopmental problems and children with PKU require a strict diet to prevent intellectual disability and other disorders. In the maternal form ofPKU,excessive maternalphenylalaninecan be absorbed by the fetus even if the fetus has not inherited the disease. This can produce intellectual disability and other disorders.[29][30]
Nutrition[edit]
Nutrition disordersand nutritional deficits may cause neurodevelopmental disorders, such asspina bifida,and the rarely occurringanencephaly,both of which areneural tube defectswith malformation and dysfunction of thenervous systemand its supporting structures, leading to serious physical disability and emotional sequelae. The most common nutritional cause of neural tube defects isfolic aciddeficiency in the mother, a B vitamin usually found in fruits, vegetables, whole grains, and milk products.[31][32](Neural tube defects are also caused by medications and other environmental causes, many of which interfere with folate metabolism, thus they are considered to have multifactorial causes.)[33][34]Another deficiency,iodine deficiency,produces a spectrum of neurodevelopmental disorders ranging from mild emotional disturbance to severe intellectual disability. (see alsocongenital iodine deficiency syndrome).[35]
Excesses in both maternal and infant diets may cause disorders as well, with foods orfood supplementsproving toxic in large amounts. For instance in 1973 K.L. Jones and D.W. Smith of theUniversity of WashingtonMedical School inSeattlefound a pattern of "craniofacial, limb, and cardiovascular defects associated with prenatal onset growth deficiency and developmental delay" in children ofalcoholicmothers, now calledfetal alcohol syndrome,It has significant symptom overlap with several other entirely unrelated neurodevelopmental disorders.[36]
Physical trauma[edit]
Brain trauma in the developing human is a common cause (over 400,000 injuries per year in the US alone, without clear information as to how many produce developmental sequellae)[37]of neurodevelopmental syndromes. It may be subdivided into two major categories,congenital injury(including injury resulting from otherwise uncomplicated premature birth)[38]and injury occurring in infancy or childhood. Common causes of congenital injury areasphyxia(obstruction of thetrachea),hypoxia(lack of oxygen to the brain), and themechanical traumaof thebirth processitself.[39]
Placenta[edit]
Although it not clear yet as strong is the correlation betweenplacentaand brain, a growing number of studies are linking placenta to fetal brain development.[40]
Diagnosis[edit]
Neurodevelopmental disorders are diagnosed by evaluating the presence of characteristic symptoms or behaviors in a child, typically after a parent, guardian, teacher, or other responsible adult has raised concerns to a doctor.[41]
Neurodevelopmental disorders may also be confirmed bygenetic testing.Traditionally, disease related genetic and genomic factors are detected bykaryotype analysis,which detects clinically significant genetic abnormalities for 5% of children with a diagnosed disorder. As of 2017[update],chromosomal microarray analysis(CMA) was proposed to replace karyotyping because of its ability to detect smaller chromosome abnormalities andcopy-number variants,leading to greater diagnostic yield in about 20% of cases.[19]TheAmerican College of Medical Genetics and Genomicsand theAmerican Academy of Pediatricsrecommend CMA as standard of care in the US.[19]
Management[edit]
This section is empty.You can help byadding to it.(July 2023) |
See also[edit]
- Developmental disability
- Epigenetics
- Microcephaly
- Teratology
- TRPM3-related neurodevelopmental disorders
References[edit]
- ^abcdefgDiagnostic and statistical manual of mental disorders: DSM-5(5th ed.). Washington: American psychiatric association. 2013.ISBN978-0-89042-554-1.
- ^abMorris-Rosendahl DJ, Crocq MA (March 2020)."Neurodevelopmental disorders-the history and future of a diagnostic concept".Dialogues in Clinical Neuroscience.22(1): 65–72.doi:10.31887/DCNS.2020.22.1/macrocq.PMC7365295.PMID32699506.
- ^Mammarella IC, Cornoldi C (2020). "Nonverbal learning disability (developmental visuospatial disorder)".Neurocognitive Development: Disorders and Disabilities.Handbook of Clinical Neurology. Vol. 174. pp. 83–91.doi:10.1016/B978-0-444-64148-9.00007-7.ISBN9780444641489.PMID32977898.S2CID221939377.
- ^Incháustegui MV (2019-06-18)."Nonverbal Learning Disabilities (Nld) – Clinical Description about Neurodevelopmental Disabilities".Archives in Neurology & Neuroscience.4(1).doi:10.33552/ANN.2019.04.000579.
- ^Mammarella IC, Cornoldi C (2020). "Nonverbal learning disability (developmental visuospatial disorder)".Neurocognitive Development: Disorders and Disabilities.Handbook of Clinical Neurology. Vol. 174. Elsevier. pp. 83–91.doi:10.1016/b978-0-444-64148-9.00007-7.ISBN978-0-444-64148-9.PMID32977898.S2CID221939377.
- ^Spreen O (September 2011)."Nonverbal learning disabilities: a critical review".Child Neuropsychology.17(5): 418–443.doi:10.1080/09297049.2010.546778.PMID21462003.S2CID31974898.Archivedfrom the original on 2021-07-20.Retrieved2021-04-29.
- ^Mammarella IC, Cornoldi C (2014-05-04). "An analysis of the criteria used to diagnose children with Nonverbal Learning Disability (NLD)".Child Neuropsychology.20(3): 255–280.doi:10.1080/09297049.2013.796920.hdl:11577/2668053.PMID23705673.S2CID34107811.
- ^Morris-Rosendahl DJ, Crocq MA (March 2020)."Neurodevelopmental disorders-the history and future of a diagnostic concept".Dialogues in Clinical Neuroscience.22(1): 65–72.doi:10.31887/DCNS.2020.22.1/macrocq.PMC7365295.PMID32699506.
- ^Pletikos M, Sousa AM, Sedmak G, Meyer KA, Zhu Y, Cheng F, et al. (January 2014)."Temporal specification and bilaterality of human neocortical topographic gene expression".Neuron.81(2): 321–332.doi:10.1016/j.neuron.2013.11.018.PMC3931000.PMID24373884.
- ^Samaco RC, Hogart A, LaSalle JM (February 2005)."Epigenetic overlap in autism-spectrum neurodevelopmental disorders: MECP2 deficiency causes reduced expression of UBE3A and GABRB3".Human Molecular Genetics.14(4): 483–492.doi:10.1093/hmg/ddi045.PMC1224722.PMID15615769.
- ^Sizemore, Nicholas; Oliphant, Kaitlyn; Zheng, Ruolin; Martin, Camilia R.; Claud, Erika C.; Chattopadhyay, Ishanu (2024-04-12)."A digital twin of the infant microbiome to predict neurodevelopmental deficits".Science Advances.10(15): eadj0400.doi:10.1126/sciadv.adj0400.ISSN2375-2548.PMC11006218.PMID38598636.
- ^van IJzendoorn MH, Palacios J, Sonuga-Barke EJ, Gunnar MR, Vorria P, McCall RB, et al. (December 2011)."Children in Institutional Care: Delayed Development and Resilience".Monographs of the Society for Research in Child Development.76(4): 8–30.doi:10.1111/j.1540-5834.2011.00626.x.PMC4130248.PMID25125707.
- ^Nelson CA, Zeanah CH, Fox NA, Marshall PJ, Smyke AT, Guthrie D (December 2007). "Cognitive recovery in socially deprived young children: the Bucharest Early Intervention Project".Science.318(5858): 1937–1940.Bibcode:2007Sci...318.1937N.doi:10.1126/science.1143921.PMID18096809.S2CID1460630.[permanent dead link]
- ^Diamandopoulos K, Green J (October 2018). "Down syndrome: An integrative review".Journal of Neonatal Nursing.24(5): 235–241.doi:10.1016/j.jnn.2018.01.001.S2CID57620027.
- ^"Facts about down syndrome".National Association of Down Syndrome.Archived fromthe originalon 2012-04-03.
- ^Martin JP, Bell J (July 1943)."A Pedigree of Mental Defect Showing Sex-Linkage".Journal of Neurology and Psychiatry.6(3–4): 154–157.doi:10.1136/jnnp.6.3-4.154.PMC1090429.PMID21611430.
- ^Amir RE, Van den Veyver IB, Wan M, Tran CQ, Francke U, Zoghbi HY (October 1999). "Rett syndrome is caused by mutations in X-linked MECP2, encoding methyl-CpG-binding protein 2".Nature Genetics.23(2): 185–188.doi:10.1038/13810.PMID10508514.S2CID3350350.
- ^Merla G, Howald C, Henrichsen CN, Lyle R, Wyss C, Zabot MT, et al. (August 2006)."Submicroscopic deletion in patients with Williams-Beuren syndrome influences expression levels of the nonhemizygous flanking genes".American Journal of Human Genetics.79(2): 332–341.doi:10.1086/506371.PMC1559497.PMID16826523.
- ^abcMartin CL, Ledbetter DH (June 2017)."Chromosomal Microarray Testing for Children With Unexplained Neurodevelopmental Disorders".JAMA.317(24): 2545–2546.doi:10.1001/jama.2017.7272.PMC7058144.PMID28654998.
- ^Pavone P, Bianchini R, Parano E, Incorpora G, Rizzo R, Mazzone L, Trifiletti RR (February 2004). "Anti-brain antibodies in PANDAS versus uncomplicated streptococcal infection".Pediatric Neurology.30(2): 107–110.doi:10.1016/S0887-8994(03)00413-2.hdl:2108/194065.PMID14984902.
- ^Dale RC, Heyman I, Giovannoni G, Church AW (October 2005)."Incidence of anti-brain antibodies in children with obsessive-compulsive disorder".The British Journal of Psychiatry.187(4): 314–319.doi:10.1192/bjp.187.4.314.PMID16199788.
- ^Swedo SE (December 2001)."Genetics of childhood disorders: XXXIII. Autoimmunity, part 6: poststreptococcal autoimmunity".Journal of the American Academy of Child and Adolescent Psychiatry.40(12): 1479–1482.doi:10.1097/00004583-200112000-00021.PMID11765296.Archivedfrom the original on 2021-07-20.Retrieved2008-08-17.
- ^abBoivin MJ, Kakooza AM, Warf BC, Davidson LL, Grigorenko EL (November 2015)."Reducing neurodevelopmental disorders and disability through research and interventions".Nature.527(7578): S155–S160.Bibcode:2015Natur.527S.155B.doi:10.1038/nature16029.PMID26580321.
- ^Brown AS (April 2006)."Prenatal infection as a risk factor for schizophrenia".Schizophrenia Bulletin.32(2): 200–202.doi:10.1093/schbul/sbj052.PMC2632220.PMID16469941.
- ^Richardson AJ, Ross MA (July 2000). "Fatty acid metabolism in neurodevelopmental disorder: a new perspective on associations between attention-deficit/hyperactivity disorder, dyslexia, dyspraxia and the autistic spectrum".Prostaglandins, Leukotrienes, and Essential Fatty Acids.63(1–2): 1–9.doi:10.1054/plef.2000.0184.PMID10970706.
- ^Northam EA, Anderson PJ, Jacobs R, Hughes M, Warne GL, Werther GA (September 2001)."Neuropsychological profiles of children with type 1 diabetes 6 years after disease onset".Diabetes Care.24(9): 1541–1546.doi:10.2337/diacare.24.9.1541.PMID11522696.
- ^Olsson GM, Hulting AL, Montgomery SM (March 2008)."Cognitive function in children and subsequent type 2 diabetes".Diabetes Care.31(3): 514–516.doi:10.2337/dc07-1399.PMC2453642.PMID18083794.[permanent dead link]
- ^Ornoy A, Wolf A, Ratzon N, Greenbaum C, Dulitzky M (July 1999)."Neurodevelopmental outcome at early school age of children born to mothers with gestational diabetes".Archives of Disease in Childhood. Fetal and Neonatal Edition.81(1): F10–F14.doi:10.1136/fn.81.1.F10.PMC1720965.PMID10375355.
- ^Lee PJ, Ridout D, Walter JH, Cockburn F (February 2005)."Maternal phenylketonuria: report from the United Kingdom Registry 1978-97".Archives of Disease in Childhood.90(2): 143–146.doi:10.1136/adc.2003.037762.PMC1720245.PMID15665165.
- ^Rouse B, Azen C, Koch R, Matalon R, Hanley W, de la Cruz F, et al. (March 1997). "Maternal Phenylketonuria Collaborative Study (MPKUCS) offspring: facial anomalies, malformations, and early neurological sequelae".American Journal of Medical Genetics.69(1): 89–95.doi:10.1002/(SICI)1096-8628(19970303)69:1<89::AID-AJMG17>3.0.CO;2-K.PMID9066890.
- ^"Folic Acid".March of Dimes.Archivedfrom the original on 2021-08-26.Retrieved2014-11-10.
- ^"Folate (Folacin, Folic Acid)".Ohio State University Extension.Archivedfrom the original on 2021-08-26.Retrieved2008-08-06.
- ^"Folic scid: topic home".Centers for Disease Control and Prevention.U.S. Department of Health and Human Services.Archivedfrom the original on 2021-08-26.Retrieved2008-08-02.
- ^"The basics about spina bifida".Centers for Disease Control and Prevention.U.S. Department of Health and Human Services.Archivedfrom the original on 2021-08-26.Retrieved2008-08-02.
- ^Skeaff SA (February 2011)."Iodine deficiency in pregnancy: the effect on neurodevelopment in the child".Nutrients.3(2): 265–273.doi:10.3390/nu3020265.PMC3257674.PMID22254096.
- ^Fetal alcohol syndrome: guidelines for referral and diagnosis (PDF).Archived2009-04-23 at theWayback MachineCDC (July 2004). Retrieved on 2007-04-11
- ^"Facts About TBI"(PDF).U.S. Centers for Disease Control and Prevention.Archivedfrom the original on 2021-08-26.Retrieved2008-08-06.
- ^Murray RM, Lewis SW (September 1987)."Is schizophrenia a neurodevelopmental disorder?".British Medical Journal.295(6600): 681–682.doi:10.1136/bmj.295.6600.681.PMC1247717.PMID3117295.
- ^Collins KA, Popek E (December 2018)."Birth Injury: Birth Asphyxia and Birth Trauma".Academic Forensic Pathology.8(4): 788–864.doi:10.1177/1925362118821468.PMC6491540.PMID31240076.
- ^Kratimenos P, Penn AA (August 2019)."Placental programming of neuropsychiatric disease".Pediatric Research.86(2): 157–164.doi:10.1038/s41390-019-0405-9.PMID31003234.S2CID124094051.
- ^Neurodevelopmental Disorders(PDF),America's Children and the Environment (3 ed.), EPA, August 2017, p. 12,archived(PDF)from the original on 2021-07-20,retrieved2019-07-10
Further reading[edit]
- Tager-Flusberg H(1999).Neurodevelopmental disorders.Cambridge, Massachusetts: MIT Press.ISBN978-0-262-20116-2.
- Brooks DR, Fleischhacker WW (2006).Neurodevelopmental Disorders.Berlin: Springer.ISBN978-3-211-26291-7.
External links[edit]
- Neurodevelopmental DisordersatCurlie
- A Review of Neurodevelopmental Disorders– Medscape review


