Seizure
| Epileptic seizure | |
|---|---|
| Other names | Epileptic fit,[1]seizure, fit, convulsions[2] |
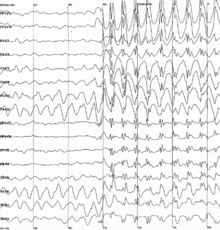 | |
| Generalized 3 Hz spike and wave discharges in anelectroencephalogram(EEG) of a patient with epilepsy | |
| Specialty | Neurology,emergency medicine |
| Symptoms | Variable[3] |
| Complications | Falling, drowning, car accidents, pregnancy complications, emotional health issues[4] |
| Duration | Typically < 2 minutes[5] |
| Types | Focal, generalized; Provoked, unprovoked[6] |
| Causes | Provoked:Low blood sugar,alcohol withdrawal,low blood sodium,fever,brain infection,traumatic brain injury[3][6] Unprovoked:Unknown,brain injury,brain tumor,previousstroke[5][3][6][7] |
| Diagnostic method | Based on symptoms, blood tests,medical imaging,electroencephalography[7] |
| Differential diagnosis | Syncope,psychogenic non-epileptic seizure,migraine aura,transient ischemic attack[3][5] |
| Treatment | Less than 5 min:Place person on their side, remove nearby dangerous objects[8] More than 5 min:Treat as perstatus epilepticus[8] |
| Frequency | ~10% of people (overall worldwide lifetime risk)[5][9] |
Aseizureis a period ofsymptomsdue to abnormally excessive orsynchronous neuronal activityin thebrain.[6]Outward effects vary from uncontrolled shaking movements involving much of the body withloss of consciousness(tonic-clonic seizure), to shaking movements involving only part of the body with variable levels of consciousness (focal seizure), to a subtle momentary loss of awareness (absence seizure).[3]These episodes usually last less than two minutes and it takes some time to return to normal.[5][8]Loss of bladder controlmay occur.[3]
Seizures may be provoked and unprovoked.[6]Provoked seizures are due to a temporary event such aslow blood sugar,alcohol withdrawal,abusing alcohol together with prescription medication,low blood sodium,fever,brain infection,flashing imagesorconcussion.[3][6]Unprovoked seizures occur without a known or fixable cause such that ongoing seizures are likely.[5][3][6][7]Unprovoked seizures may be exacerbated bystressorsleep deprivation.[3]Epilepsydescribes a brain disease in which there has been at least one unprovoked seizure and where there is a high risk of additional seizures in the future.[6]Conditions that look like epileptic seizures but are not include:fainting,nonepileptic psychogenic seizureandtremor.[3]
A seizure that lasts for more than a brief period is amedical emergency.[10]Any seizure lasting longer than five minutes should be treated asstatus epilepticus.[8]A first seizure generally does not require long-term treatment withanti-seizure medicationsunless a specific problem is found onelectroencephalogram(EEG) or brain imaging.[7]Typically it is safe to complete the work-up following a single seizure as anoutpatient.[3]In many, with what appears to be a first seizure, other minor seizures have previously occurred.[11]
Up to 10% of people have had at least one epileptic seizure in their lifetime.[5][9]Provoked seizures occur in about 3.5 per 10,000 people a year while unprovoked seizures occur in about 4.2 per 10,000 people a year.[5]After one seizure, the chance of experiencing a second one is about 40%.[12][13]Epilepsy affects about 1% of the population at any given time.[9]
Any animal that has a brain can have a seizure.[14]
Signs and symptoms
[edit]The signs and symptoms of seizures vary depending on the type.[15]The most common and stereotypical type of seizure isconvulsive(60%), typically called a tonic-clonic seizure.[16]Two-thirds of these begin asfocal seizuresprior to developing into tonic-clonic seizures.[16]The remaining 40% of seizures are non-convulsive, an example of which isabsence seizure.[17]When EEG monitoring shows evidence of a seizure, but no symptoms are present, it is referred to as a subclinical seizure.[18]
Focal seizures
[edit]Focal seizuresoften begin with certain experiences, known as anaura.[15]These may include sensory (including visual, auditory, etc.), cognitive, autonomic,olfactoryor motor phenomena.[19]
In acomplex partial seizure,a person may appear confused or dazed and cannot respond to questions or direction.[19]
Jerking activity may start in a specific muscle group and spread to surrounding muscle groups—known as aJacksonian march.[20]Unusual activities that are not consciously created may occur.[20]These are known asautomatismsand include simple activities like smacking of the lips or more complex activities such as attempts to pick something up.[20]
Generalized seizures
[edit]There are six main types of generalized seizures: tonic-clonic, tonic, clonic, myoclonic, absence, and atonic seizures.[21]They all involve a loss of consciousness and typically happen without warning.[22]
- Tonic-clonic seizures present with a contraction of the limbs followed by their extension, along with arching of the back for 10–30 seconds.[22]A cry may be heard due to contraction of the chest muscles.[22]The limbs then begin to shake in unison.[22]After the shaking has stopped it may take 10–30 minutes for the person to return to normal.[22]
- Tonic seizures produce constant contractions of the muscles.[22]The person may turn blue if breathing is impaired.[22]
- Clonic seizures involve shaking of the limbs in unison.[22]
- Myoclonic seizures involve spasms of muscles in either a few areas or generalized through the body.[22]
- Absence seizures can be subtle, with only a slight turn of the head or eye blinking.[19]The person often does not fall over and may return to normal right after the seizure ends, though there may also be a period of post-ictal disorientation.[19]
- Atonic seizures involve the loss of muscle activity for greater than one second.[20]This typically occurs bilaterally (on both sides of the body).[20]
Duration
[edit]A seizure can last from a few seconds to more than five minutes, at which point it is known asstatus epilepticus.[23]Most tonic-clonic seizures last less than two or three minutes.[23]Absence seizures are usually around 10 seconds in duration.[17]
Postictal
[edit]After the active portion of a seizure, there is typically a period of confusion called thepostictalperiod, before a normallevel of consciousnessreturns.[15]This period usually lasts 3 to 15 minutes,[24]but may last for hours.[25]Other symptoms during this period include: tiredness,headache,difficulty speaking, and abnormal behavior.[25]Psychosisafter a seizure occurs in 6–10% of people.[26][25]
Causes
[edit]Seizures have a number of causes. Of those who have a seizure, about 25% haveepilepsy.[27]A number of conditions are associated with seizures but are not epilepsy including: mostfebrile seizuresand those that occur around an acute infection, stroke, or toxicity.[28]These seizures are known as "acute symptomatic" or "provoked" seizures and are part of the seizure-related disorders.[28]In many the cause is unknown.
Different causes of seizures are common in certain age groups.
- Seizures in babiesare most commonly caused byhypoxic ischemic encephalopathy,central nervous system (CNS) infections, trauma, congenital CNS abnormalities, andmetabolic disorders.
- The most frequent cause of seizures in children is febrile seizures, which happen in 2–5% of children between the ages of six months and five years.[29]
- During childhood, well-defined epilepsy syndromes are generally seen.
- In adolescence and young adulthood, non-compliance with the medication regimen and sleep deprivation are potential triggers.
- Pregnancy and labor and childbirth, and the post-partum, or post-natal period (after birth) can be at-risk times, especially if there are certain complications likepre-eclampsia.
- During adulthood, the likely causes are alcohol related, strokes, trauma, CNS infections, and brain tumors.[30]
- In older adults,cerebrovascular diseaseis a very common cause. Other causes are CNS tumors, head trauma, and other degenerative diseases that are common in the older age group, such asdementia.[31]
Metabolic
[edit]Dehydrationcan trigger epileptic seizures if it is severe enough.[32]A number of disorders including:low blood sugar,low blood sodium,hyperosmolar nonketotic hyperglycemia,high blood sodium,low blood calciumandhigh blood urealevels may cause seizures.[22]As mayhepatic encephalopathyand the genetic disorderporphyria.[22]
Structural
[edit]- Cavernomaorcavernous malformationis a treatable medical condition that can cause seizures, headaches, and brain hemorrhages.
- Arteriovenous malformation(AVM) is a treatable medical condition that can cause seizures, headaches, and brain hemorrhages.
- Space-occupying lesions in the brain (abscesses,tumours). In people withbrain tumours,the frequency of epilepsy depends on the location of the tumor in thecortical region.[33]
Medications
[edit]Both medication anddrug overdosescan result in seizures,[22]as may certain medication anddrug withdrawal.[22]Common drugs involved include:antidepressants,antipsychotics,cocaine,insulin,and thelocal anaestheticlidocaine.[22]Difficulties with withdrawal seizures commonly occur after prolonged alcohol orsedativeuse, a condition known asdelirium tremens.[22]In people who are at risk of developing epileptic seizures, commonherbal medicinessuch asephedra,ginkgo bilobaandwormwoodcan provoke seizures.[34]
Infections
[edit]- Infection with thepork tapeworm,which can causeneurocysticercosis,is the cause of up to half of epilepsy cases in areas of the world where the parasite is common.[35]
- Parasitic infections such as cerebralmalaria.In Nigeria this is one of the most common causes of seizures among children under five years of age.[36]
- Infection,such asencephalitisormeningitis[37]
Stress
[edit]Stress can induce seizures in people withepilepsy,and is a risk factor for developing epilepsy. Severity, duration, and time at which stress occurs during development all contribute to frequency and susceptibility to developing epilepsy. It is one of the most frequently self-reported triggers in patients with epilepsy.[38][39]
Stress exposure results inhormonerelease that mediates its effects in the brain. These hormones act on both excitatory and inhibitory neuralsynapses,resulting in hyper-excitability ofneuronsin the brain. Thehippocampusis known to be a region that is highly sensitive to stress and prone to seizures. This is where mediators of stress interact with their target receptors to produce effects.[40]
Other
[edit]Seizures may occur as a result ofhigh blood pressure,known ashypertensive encephalopathy,or in pregnancy aseclampsiawhen accompanied by either seizures or a decreased level of consciousness.[22]Very high body temperaturesmay also be a cause.[22]Typically this requires a temperature greater than 42 °C (107.6 °F).[22]
- Head injurymay cause non-epilepticpost-traumatic seizuresorpost-traumatic epilepsy
- About 3.5 to 5.5% of people withceliac diseasealso have seizures.[41]
- Seizures in a person with ashuntmay indicate failure
- Hemorrhagicstrokecan occasionally present with seizures,embolicstrokes generally do not (though epilepsy is a common later complication);cerebral venous sinus thrombosis,a rare type of stroke, is more likely to be accompanied by seizures than other types of stroke
- Multiple sclerosismay cause seizures
- Electroconvulsive therapy(ECT) deliberately sets out to induce a seizure for the treatment of major depression.
- Reflex seizureinduced by a specific stimulus ortrigger(extrinsic or intrinsic stimuli)
- For people withphotosensitive epilepsy,exposure to flashing lights or rapid blinking may cause a seizure.[42][43][44]
Mechanism
[edit]Normally, brain electrical activity is non-synchronous.[19]In epileptic seizures, due to problems within the brain,[45]a group of neurons begin firing in an abnormal, excessive,[16]and synchronized manner.[19]This results in a wave of depolarization known as aparoxysmal depolarizing shift.[46]
Normally after anexcitatory neuronfires it becomes more resistant to firing for a period of time.[19]This is due in part from the effect of inhibitory neurons, electrical changes within the excitatory neuron, and the negative effects ofadenosine.[19]In epilepsy the resistance of excitatory neurons to fire during this period is decreased.[19]This may occur due to changes inion channelsor inhibitory neurons not functioning properly.[19]Forty-one ion-channel genes and over 1,600 ion-channel mutations have been implicated in the development of epileptic seizure.[47]These ion channel mutations tend to confer a depolarized resting state to neurons resulting in pathological hyper-excitability.[48]This long-lasting depolarization in individual neurons is due to an influx of Ca2+from outside of the cell and leads to extended opening of Na+channels and repetitive action potentials.[49]The followinghyperpolarizationis facilitated byγ-aminobutyric acid(GABA) receptors orpotassium (K+) channels,depending on the type of cell.[49]Equally important in epileptic neuronal hyper-excitability is the reduction in the activity of inhibitoryGABAergicneurons, an effect known as disinhibition. Disinhibition may result from inhibitory neuron loss, dysregulation of axonal sprouting from the inhibitory neurons in regions of neuronal damage, or abnormal GABAergic signaling within the inhibitory neuron.[50]Neuronal hyper-excitability results in a specific area from which seizures may develop, known as a "seizure focus".[19]Following an injury to the brain, another mechanism of epilepsy may be the up regulation of excitatory circuits or down regulation of inhibitory circuits.[19][51]These secondary epilepsies occur through processes known asepileptogenesis.[19][51]Failure of theblood–brain barriermay also be a causal mechanism.[52]While blood-brain barrier disruption alone does appear to cause epileptogenesis, it has been correlated to increased seizure activity.[53]Furthermore, it has been implicated in chronic epileptic conditions through experiments inducing barrier permeability with chemical compounds.[53]Disruption may lead to fluid leaking out of the blood vessels into the area between cells and driving epileptic seizures.[54]Preliminary findings of blood proteins in the brain after a seizure support this theory.[53]
Focal seizures begin in onehemisphere of the brainwhile generalized seizures begin in both hemispheres.[21]Some types of seizures may change brain structure, while others appear to have little effect.[55]Gliosis,neuronal loss, and atrophy of specific areas of the brain are linked to epilepsy but it is unclear if epilepsy causes these changes or if these changes result in epilepsy.[55]
Seizure activity may be propagated through the brain's endogenous electrical fields.[56]Proposed mechanisms that may cause the spread and recruitment of neurons include an increase in K+from outside the cell,[57][unreliable medical source]and increase of Ca2+in the presynaptic terminals.[49]These mechanisms blunt hyperpolarization and depolarizes nearby neurons, as well as increasing neurotransmitter release.[49]
Diagnosis
[edit]
Seizures may be divided into provoked and unprovoked.[6]Provoked seizures may also be known as "acute symptomatic seizures" or "reactive seizures".[6]Unprovoked seizures may also be known as "reflex seizures".[6]Depending on the presumed causeblood testsandlumbar puncturemay be useful.[7]Hypoglycemiamay cause seizures and should be ruled out. Anelectroencephalogramand brain imaging withCT scanorMRI scanis recommended in the work-up of seizures not associated with a fever.[7][58]
Classification
[edit]Seizure typesare organized by whether the source of the seizure is localized (focal seizures) or distributed (generalized seizures) within the brain.[21]Generalized seizures are divided according to the effect on the body and includetonic-clonic(grand mal),absence(petit mal),myoclonic,clonic,tonic, andatonicseizures.[21][59]Some seizures such asepileptic spasmsare of an unknown type.[21]
Focal seizures (previously calledpartial seizures)[16]are divided intosimple partialorcomplex partial seizure.[21]Current practice no longer recommends this, and instead prefers to describe what occurs during a seizure.[21]
The classification of seizures can also be made according to dynamical criteria, observable in electrophysiological measurements. It is a classification according to their type of onset and offset.[60][61]
Physical examination
[edit]
Most people are in apostictal state(drowsy or confused) following a seizure. They may show signs of other injuries. A bite mark on the side of the tongue helps confirm a seizure when present, but only a third of people who have had a seizure have such a bite.[62]When present in people thought to have had a seizure, this physical sign tentatively increases the likelihood that a seizure was the cause.[63]
Tests
[edit]
Anelectroencephalographyis only recommended in those who likely had an epileptic seizure and may help determine the type of seizure or syndrome present. In children it is typically only needed after a second seizure. It cannot be used to rule out the diagnosis and may be falsely positive in those without the disease. In certain situations it may be useful to prefer the EEG while sleeping or sleep deprived.[64]
Diagnostic imaging byCT scanandMRIis recommended after a first non-febrile seizure to detect structural problems inside the brain.[64]MRI is generally a better imaging test except when intracranial bleeding is suspected.[7]Imaging may be done at a later point in time in those who return to their normal selves while in the emergency room.[7]If a person has a previous diagnosis of epilepsy with previous imaging repeat imaging is not usually needed with subsequent seizures.[64]
In adults, testing electrolytes,blood glucoseand calcium levels is important to rule these out as causes, as is anelectrocardiogram.[64]A lumbar puncture may be useful to diagnose acentral nervous systeminfection but is not routinely needed.[7]Routine antiseizure medical levels in the blood are not required in adults or children.[64]In children additional tests may be required.[64]
A high bloodprolactinlevel within the first 20 minutes following a seizure may be useful to confirm an epileptic seizure as opposed topsychogenic non-epileptic seizure.[65][66]Serum prolactin level is less useful for detecting partial seizures.[67]If it is normal an epileptic seizure is still possible[66]and a serum prolactin does not separate epileptic seizures from syncope.[68]It is not recommended as a routine part of diagnosis epilepsy.[64]
Differential diagnosis
[edit]Differentiating an epileptic seizure from other conditions such assyncopecan be difficult.[15]Other possible conditions that can mimic a seizure include:decerebrate posturing,psychogenic seizures,tetanus,dystonia,migraine headaches,andstrychnine poisoning.[15]In addition, 5% of people with a positivetilt table testmay have seizure-like activity that seems due tocerebral hypoxia.[69]Convulsions may occur due to psychological reasons and this is known as apsychogenic non-epileptic seizure.Non-epileptic seizuresmay also occur due to a number of other reasons.
Prevention
[edit]A number of measures have been attempted to prevent seizures in those at risk. Followingtraumatic brain injuryanticonvulsants decrease the risk of early seizures but not late seizures.[70]
In those with a history offebrile seizures,some medications (bothantipyreticsand anticonvulsants) have been found effective for reducing reoccurrence, however due to the frequency of adverse effects and the benign nature of febrile seizures the decision to use medication should be weighted carefully against potential negative effects.[71]
There is no clear evidence that antiepileptic drugs are effective or not effective at preventing seizures following acraniotomy,[72]followingsubdural hematoma,[73]after astroke,[74][75]or aftersubarachnoid haemorrhage,[76]for both people who have had a previous seizure, and those who have not.
Management
[edit]Potentially sharp or dangerous objects should be moved from the area around a person experiencing a seizure so that the individual is not hurt. After the seizure, if the person is not fully conscious and alert, they should be placed in therecovery position.A seizure longer than five minutes, or two or more seizures occurring within the time of five minutes is a medical emergency known asstatus epilepticus.[23][77]Contrary to a common misconception, bystanders should not attempt to force objects into the mouth of the person having a seizure, as doing so may cause injury to the teeth and gums.[78]
Treatments of a person that is actively seizing follows a progression from initial response, through first line, second line, and third line treatments.[79]The initial response involves ensuring the person is protected from potential harms (such as nearby objects) and managing their airway, breathing, and circulation.[79]Airway management should include placing the person on their side, known as therecovery position,to prevent them from choking.[79]If they are unable to breathe because something is blocking their airway, they may require treatments to open their airway.[79]
Medication
[edit]The first line medication for an actively seizing person is abenzodiazepine,with most guidelines recommendinglorazepam.[58][80]Diazepam and midazolam are alternatives. This may be repeated if there is no effect after 10 minutes.[58]If there is no effect after two doses,barbituratesorpropofolmay be used.[58]
Second-line therapy for adults is phenytoin or fosphenytoin and phenobarbital for children.[81][page needed]Third-line medications include phenytoin for children and phenobarbital for adults.[81][page needed]
Ongoing anti-epileptic medications are not typically recommended after a first seizure except in those with structural lesions in the brain.[58]They are generally recommended after a second one has occurred.[58]Approximately 70% of people can obtain full control with continuous use of medication.[45]Typically one type of anticonvulsant is preferred. Following a first seizure, while immediate treatment with an anti-seizure drug lowers the probability of seizure recurrence up to five years it does not change the risk of death and there are potential side effects.[82]
In seizures related to toxins, up to two doses of benzodiazepines should be used.[83]If this is not effectivepyridoxineis recommended.[83]Phenytoinshould generally not be used.[83]
There is a lack of evidence for preventive anti-epileptic medications in the management of seizures related tointracranial venous thrombosis.[75]
Surgery
[edit]In severe cases, brain surgery can be a treatment option for epilepsy.[84]See alsoEpilepsy Surgery.
Other
[edit]Helmets may be used to provide protection to the head during a seizure. Some claim thatseizure response dogs,a form ofservice dog,can predict seizures.[85]Evidence for this, however, is poor.[85]At present there is not enough evidence to support the use ofcannabisfor the management of seizures, although this is an ongoing area of research.[86][87]There is low quality evidence that aketogenic dietmay help in those who have epilepsy and is reasonable in those who do not improve following typical treatments.[88]
Prognosis
[edit]Following a first seizure, the risk of more seizures in the next two years is around 40%.[12][13]The greatest predictors of more seizures are problems either on the electroencephalogram or on imaging of the brain.[7]In adults, after 6 months of being seizure-free after a first seizure, the risk of a subsequent seizure in the next year is less than 20% regardless of treatment.[89]Up to 7% of seizures that present to the emergency department (ER) are in status epilepticus.[58]In those with a status epilepticus, mortality is between 10% and 40%.[15]Those who have a seizure that is provoked (occurring close in time to an acute brain event or toxic exposure) have a low risk of re-occurrence, but have a higher risk of death compared to those with epilepsy.[90]
Epidemiology
[edit]Approximately 8–10% of people will experience an epileptic seizure during their lifetime.[91]In adults, the risk of seizure recurrence within the five years following a new-onset seizure is 35%; the risk rises to 75% in persons who have had a second seizure.[91]In children, the risk of seizure recurrence within the five years following a single unprovoked seizure is about 50%; the risk rises to about 80% after two unprovoked seizures.[92]In the United States in 2011, seizures resulted in an estimated 1.6 million emergency department visits; approximately 400,000 of these visits were for new-onset seizures.[91]The exact incidence of epileptic seizures in low-income and middle-income countries is unknown, however it probably exceeds that in high-income countries.[93]This may be due to increased risks of traffic accidents, birth injuries, andmalariaand other parasitic infections.[93]
History
[edit]Epileptic seizures were first described in an Akkadian text from 2000 B.C.[94]Early reports of epilepsy often saw seizures and convulsions as the work of "evil spirits".[95]The perception of epilepsy, however, began to change in the time of Ancient Greek medicine. The term "epilepsy" itself is a Greek word, which is derived from the verb "epilambanein", meaning "to seize, possess, or afflict".[94]Although the Ancient Greeks referred to epilepsy as the "sacred disease",this perception of epilepsy as a" spiritual "disease was challenged by Hippocrates in his workOn the Sacred Disease,who proposed that the source of epilepsy was from natural causes rather than supernatural ones.[95]
Early surgical treatment of epilepsy was primitive in Ancient Greek, Roman and Egyptian medicine.[96]The 19th century saw the rise of targeted surgery for the treatment of epileptic seizures, beginning in 1886 with localized resections performed by SirVictor Horsley,a neurosurgeon in London.[95]Another advancement was that of the development by the Montreal procedure by Canadian neurosurgeonWilder Penfield,which involved use of electrical stimulation among conscious patients to more accurately identify and resect the epileptic areas in the brain.[95]
Society and culture
[edit]Economics
[edit]Seizures result in direct economic costs of about one billion dollars in the United States.[7]Epilepsy results in economic costs in Europe of around €15.5 billion in 2004.[16]In India, epilepsy is estimated to result in costs of US$1.7 billion or 0.5% of the GDP.[45]They make up about 1% of emergency department visits (2% for emergency departments for children) in the United States.[30]
Driving
[edit]Many areas of the world require a minimum of six months from the last seizure before people can drive a vehicle.[7]
Research
[edit]Scientific work into the prediction of epileptic seizures began in the 1970s. Several techniques and methods have been proposed, but evidence regarding their usefulness is still lacking.[97]
Two promising areas includegene therapy,[98]and seizure detection andseizure prediction.[99]
Gene therapy for epilepsy consists of employing vectors to deliver pieces of genetic material to areas of the brain involved in seizure onset.[98]
Seizure prediction is a special case of seizure detection in which the developed systems is able to issue a warning before the clinical onset of the epileptic seizure.[97][99]
Computational neuroscience has been able to bring a new point of view on the seizures by considering the dynamical aspects.[61]
References
[edit]- ^Shorvon S (2009).Epilepsy.OUP Oxford. p. 1.ISBN9780199560042.
- ^"Epileptic Seizures - National Library of Medicine".PubMed Health.Retrieved16 October2018.
- ^abcdefghijkMisulis KE, Murray EL (2017).Essentials of Hospital Neurology.Oxford University Press. p. Chapter 19.ISBN9780190259433.
- ^Mayo Clinic Staff."Seizures – Symptoms and causes".Mayo Clinic.
- ^abcdefghFerri FF (2018).Ferri's Clinical Advisor 2019 E-Book: 5 Books in 1.Elsevier Health Sciences. p. 959.ISBN9780323550765.
- ^abcdefghijkFisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, et al. (April 2014)."ILAE official report: a practical clinical definition of epilepsy".Epilepsia.55(4): 475–482.doi:10.1111/epi.12550.PMID24730690.S2CID35958237.
- ^abcdefghijklWilden JA, Cohen-Gadol AA (August 2012). "Evaluation of first nonfebrile seizures".American Family Physician.86(4): 334–340.PMID22963022.
- ^abcd"The Epilepsies and Seizures: Hope Through Research".National Institute of Neurological Disorders and Stroke.Retrieved16 October2018.
- ^abc"Epilepsy".World Health Organization.9 February 2023.Retrieved4 June2023.
- ^Schachter SC, Shafer PL, Sirven JI (5 November 2013)."What Is A Seizure Emergency".epilepsy.
- ^Angus-Leppan H (April 2014). "First seizures in adults".BMJ.348:g2470.doi:10.1136/bmj.g2470.PMID24736280.S2CID31709502.
- ^abNeligan, Aidan; Adan, Guleed; Nevitt, Sarah J; Pullen, Angie; Sander, Josemir W; Bonnett, Laura; Marson, Anthony G (23 January 2023). Cochrane Epilepsy Group (ed.)."Prognosis of adults and children following a first unprovoked seizure".Cochrane Database of Systematic Reviews.2023(1): CD013847.doi:10.1002/14651858.CD013847.pub2.PMC9869434.PMID36688481.
- ^ab"Epilepsy: what are the chances of having a second seizure?".NIHR Evidence.National Institute for Health and Care Research. 2023.doi:10.3310/nihrevidence_59456.S2CID260965684.
- ^"I Think My Pet Had a Seizure. Now What?".Veterinary Medicine at Illinois.Retrieved6 June2024.
- ^abcdefShearer P."Seizures and Status Epilepticus: Diagnosis and Management in the Emergency Department".Emergency Medicine Practice.Archivedfrom the original on 30 December 2010.
- ^abcdeNational Institute for Health and Clinical Excellence (January 2012)."Chapter 1: Introduction"(PDF).The Epilepsies: The diagnosis and management of the epilepsies in adults and children in primary and secondary care.National Clinical Guideline Centre. pp. 21–28.Archived(PDF)from the original on 16 December 2013.
- ^abHughes JR (August 2009). "Absence seizures: a review of recent reports with new concepts".Epilepsy & Behavior.15(4): 404–412.doi:10.1016/j.yebeh.2009.06.007.PMID19632158.S2CID22023692.
- ^Sokol DK, Markand ON, Daly EC, Luerssen TG, Malkoff MD (July 2000)."Near infrared spectroscopy (NIRS) distinguishes seizure types".Seizure.9(5): 323–327.doi:10.1053/seiz.2000.0406.PMID10933986.
- ^abcdefghijklmMcPhee SJ, Hammer GD, eds. (2010). "7".Pathophysiology of disease: an introduction to clinical medicine(6th ed.). New York: McGraw-Hill Medical.ISBN978-0-07-162167-0.
- ^abcdeBradley WG (2012). "67".Bradley's neurology in clinical practice(6th ed.). Philadelphia, PA: Elsevier/Saunders.ISBN978-1-4377-0434-1.
- ^abcdefgNational Institute for Health and Clinical Excellence (January 2012)."Chapter 9: Classification of seizures and epilepsy syndromes"(PDF).The Epilepsies: The diagnosis and management of the epilepsies in adults and children in primary and secondary care.National Clinical Guideline Centre. pp. 119–129.Archived(PDF)from the original on 16 December 2013.
- ^abcdefghijklmnopqrGreenberg DA, Aminoff MJ, Simon RP (2012). "12".Clinical neurology(8th ed.). New York: McGraw-Hill Medical.ISBN978-0-07-175905-2.
- ^abcTrinka E, Höfler J, Zerbs A (September 2012). "Causes of status epilepticus".Epilepsia.53(Suppl 4): 127–138.doi:10.1111/j.1528-1167.2012.03622.x.PMID22946730.S2CID5294771.
- ^Holmes TR (2008).Handbook of epilepsy(4th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 34.ISBN978-0-7817-7397-3.
- ^abcPanayiotopoulos CP (2010).A clinical guide to epileptic syndromes and their treatment based on the ILAE classifications and practice parameter guidelines(Rev. 2nd ed.). [London]: Springer. p. 445.ISBN978-1-84628-644-5.
- ^James W. Wheless, ed. (2009).Advanced therapy in epilepsy.Shelton, Conn.: People's Medical Pub. House. p. 443.ISBN978-1-60795-004-2.
- ^Stasiukyniene V, Pilvinis V, Reingardiene D, Janauskaite L (2009)."[Epileptic seizures in critically ill patients]".Medicina.45(6): 501–507.doi:10.3390/medicina45060066.PMID19605972.
- ^abThurman DJ, Beghi E, Begley CE, Berg AT, Buchhalter JR, Ding D, et al. (September 2011)."Standards for epidemiologic studies and surveillance of epilepsy".Epilepsia.52(Suppl 7): 2–26.doi:10.1111/j.1528-1167.2011.03121.x.PMID21899536.S2CID8505004.
- ^Graves RC, Oehler K, Tingle LE (January 2012). "Febrile seizures: risks, evaluation, and prognosis".American Family Physician.85(2): 149–153.PMID22335215.
- ^abMartindale JL, Goldstein JN, Pallin DJ (February 2011). "Emergency department seizure epidemiology".Emergency Medicine Clinics of North America.29(1): 15–27.doi:10.1016/j.emc.2010.08.002.PMID21109099.
- ^Harrison's Principles of Medicine. 15th edition
- ^"diet and nutrition".8 May 2013.Archivedfrom the original on 29 June 2015.
- ^Hildebrand J (July 2004). "Management of epileptic seizures".Current Opinion in Oncology.16(4): 314–317.doi:10.1097/01.cco.0000127720.17558.38.PMID15187884.S2CID12828909.
- ^Bauer, Derek; Quigg, Mark (April 2019)."Optimizing Management of Medically Responsive Epilepsy".CONTINUUM: Lifelong Learning in Neurology.25(2): 343–361.doi:10.1212/CON.0000000000000709.ISSN1080-2371.PMID30921013.S2CID85563793.
- ^Bhalla D, Godet B, Druet-Cabanac M, Preux PM (June 2011). "Etiologies of epilepsy: a comprehensive review".Expert Review of Neurotherapeutics.11(6): 861–876.doi:10.1586/ern.11.51.PMID21651333.S2CID21190601.
- ^"Management of Convulsion in Children, a Health concern in Nigeria".Public Health Nigeria.October 2018. Archived fromthe originalon 18 October 2018.Retrieved18 October2018.
- ^Carlson N (22 January 2012).Physiology of Behavior.Neurological Disorders. Vol. 11th edition. Pearson. p. 550.ISBN978-0-205-23939-9.
- ^Nakken KO, Solaas MH, Kjeldsen MJ, Friis ML, Pellock JM, Corey LA (February 2005). "Which seizure-precipitating factors do patients with epilepsy most frequently report?".Epilepsy & Behavior.6(1): 85–89.doi:10.1016/j.yebeh.2004.11.003.PMID15652738.S2CID36696690.
- ^Haut SR, Hall CB, Masur J, Lipton RB (November 2007). "Seizure occurrence: precipitants and prediction".Neurology.69(20): 1905–1910.doi:10.1212/01.wnl.0000278112.48285.84.PMID17998482.S2CID27433395.
- ^Gunn BG, Baram TZ (November 2017)."Stress and Seizures: Space, Time and Hippocampal Circuits".Trends in Neurosciences.40(11): 667–679.doi:10.1016/j.tins.2017.08.004.PMC5660662.PMID28916130.
- ^Bushara KO (April 2005)."Neurologic presentation of celiac disease".Gastroenterology.128(4 Suppl 1): S92–S97.doi:10.1053/j.gastro.2005.02.018.PMID15825133.
- ^"Photosensitive epilepsy | Epilepsy Society".epilepsysociety.org.uk.23 February 2020.Retrieved8 June2023.
- ^"Photosensitivity and Seizures".Epilepsy Foundation.Retrieved8 June2023.
- ^Burlo, F.; Barbi, E.; Carrozzi, M.; Zanus, C. (16 November 2022)."Case report: A relevant misdiagnosis: Photosensitive epilepsy mimicking a blinking tic".Frontiers in Pediatrics.10:918420.doi:10.3389/fped.2022.918420.PMC9709211.PMID36467468.
- ^abc"Epilepsy".Fact Sheets.World Health Organization.October 2012.Archivedfrom the original on 11 March 2016.Retrieved24 January2013.
- ^Somjen GG (2004).Ions in the Brain Normal Function, Seizures, and Stroke.New York: Oxford University Press. p. 167.ISBN978-0-19-803459-9.
- ^Wei F, Yan LM, Su T, He N, Lin ZJ, Wang J, et al. (August 2017)."Ion Channel Genes and Epilepsy: Functional Alteration, Pathogenic Potential, and Mechanism of Epilepsy".Neuroscience Bulletin.33(4): 455–477.doi:10.1007/s12264-017-0134-1.PMC5567559.PMID28488083.
- ^Ropper A (2014).Adams and Victor's Principles of Neurology (10th ed., p. Chapter 16. Epilepsy and Other Seizure Disorders).New York: McGraw-Hill.
- ^abcdLowenstein DH. Seizures and Epilepsy. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J. eds. (2018)Harrison's Principles of Internal Medicine, 20eNew York, NY: McGraw-Hill.
- ^Liu YQ, Yu F, Liu WH, He XH, Peng BW (December 2014)."Dysfunction of hippocampal interneurons in epilepsy".Neuroscience Bulletin.30(6): 985–998.doi:10.1007/s12264-014-1478-4.PMC5562563.PMID25370443.
- ^abGoldberg EM, Coulter DA (May 2013)."Mechanisms of epileptogenesis: a convergence on neural circuit dysfunction".Nature Reviews. Neuroscience.14(5): 337–349.doi:10.1038/nrn3482.PMC3982383.PMID23595016.
- ^Oby E, Janigro D (November 2006)."The blood-brain barrier and epilepsy".Epilepsia.47(11): 1761–1774.doi:10.1111/j.1528-1167.2006.00817.x.PMID17116015.S2CID15074513.
- ^abcvan Vliet EA, Aronica E, Gorter JA (February 2015). "Blood-brain barrier dysfunction, seizures and epilepsy".Seminars in Cell & Developmental Biology.38:26–34.doi:10.1016/j.semcdb.2014.10.003.PMID25444846.
- ^Marchi N, Banjara M, Janigro D (February 2016)."Blood-brain barrier, bulk flow, and interstitial clearance in epilepsy".Journal of Neuroscience Methods.260:118–124.doi:10.1016/j.jneumeth.2015.06.011.PMC4835226.PMID26093166.
- ^abJerome Engel Jr.; Timothy A. Pedley, eds. (2008).Epilepsy: a comprehensive textbook(2nd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 483.ISBN978-0-7817-5777-5.
- ^Qiu C, Shivacharan RS, Zhang M, Durand DM (December 2015)."Can Neural Activity Propagate by Endogenous Electrical Field?".The Journal of Neuroscience.35(48): 15800–15811.doi:10.1523/JNEUROSCI.1045-15.2015.PMC4666910.PMID26631463.
electric fields can be solely responsible for spike propagation at... This phenomenon could be important to explain the slow propagation of epileptic activity and other normal propagations at similar speeds.
- ^Depannemaecker D, Ivanov A, Lillo D, Spek L, Bernard C, Jirsa V (17 February 2021)."A unified physiological framework of transitions between seizures, sustained ictal activity and depolarization block at the single neuron level":2020.10.23.352021.doi:10.1101/2020.10.23.352021.S2CID225962412.
{{cite journal}}:Cite journal requires|journal=(help) - ^abcdefg"Current Guidelines For Management of Seizures in the Emergency Department"(PDF).Archivedfrom the original on 30 December 2010.
- ^Simon D. Shorvon (2004).The treatment of epilepsy(2nd ed.). Malden, Mass.: Blackwell Pub.ISBN978-0-632-06046-7.
- ^Saggio ML, Crisp D, Scott JM, Karoly P, Kuhlmann L, Nakatani M, et al. (July 2020)."A taxonomy of seizure dynamotypes".eLife.9:e55632.doi:10.7554/eLife.55632.PMC7375810.PMID32691734.
- ^abDepannemaecker D, Destexhe A, Jirsa V, Bernard C (August 2021)."Modeling seizures: From single neurons to networks".Seizure.90:4–8.doi:10.1016/j.seizure.2021.06.015.PMID34219016.S2CID235468072.
- ^Peeters SY, Hoek AE, Mollink SM, Huff JS (April 2014). "Syncope: risk stratification and clinical decision making".Emergency Medicine Practice.16(4): 1–22, quiz 22–3.PMID25105200.
- ^Brigo F, Nardone R, Bongiovanni LG (October 2012)."Value of tongue biting in the differential diagnosis between epileptic seizures and syncope".Seizure.21(8): 568–572.doi:10.1016/j.seizure.2012.06.005.PMID22770819.
- ^abcdefgNational Institute for Health and Clinical Excellence (January 2012)."4"(PDF).The Epilepsies: The diagnosis and management of the epilepsies in adults and children in primary and secondary care.National Clinical Guideline Centre. pp. 57–83.
- ^Luef G (October 2010). "Hormonal alterations following seizures".Epilepsy & Behavior.19(2): 131–133.doi:10.1016/j.yebeh.2010.06.026.PMID20696621.S2CID945952.
- ^abAhmad S, Beckett MW (March 2004)."Value of serum prolactin in the management of syncope".Emergency Medicine Journal.21(2): 3e–3.doi:10.1136/emj.2003.008870.PMC1726305.PMID14988379.
- ^Shukla G, Bhatia M, Vivekanandhan S, Gupta N, Tripathi M, Srivastava A, et al. (August 2004). "Serum prolactin levels for differentiation of nonepileptic versus true seizures: limited utility".Epilepsy & Behavior.5(4): 517–521.doi:10.1016/j.yebeh.2004.03.004.PMID15256189.S2CID2381873.
- ^Chen DK, So YT, Fisher RS (September 2005)."Use of serum prolactin in diagnosing epileptic seizures: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology".Neurology.65(5): 668–675.doi:10.1212/01.wnl.0000178391.96957.d0.PMID16157897.
- ^Passman R, Horvath G, Thomas J, Kruse J, Shah A, Goldberger J, Kadish A (September 2003)."Clinical spectrum and prevalence of neurologic events provoked by tilt table testing".Archives of Internal Medicine.163(16): 1945–1948.doi:10.1001/archinte.163.16.1945.PMID12963568.
- ^Greenhalgh J, Weston J, Dundar Y, Nevitt SJ, Marson AG (April 2020)."Antiepileptic drugs as prophylaxis for postcraniotomy seizures".The Cochrane Database of Systematic Reviews.4(4): CD007286.doi:10.1002/14651858.CD007286.pub5.PMC7195181.PMID32343399.
- ^Offringa M, Newton R, Nevitt SJ, Vraka K (June 2021)."Prophylactic drug management for febrile seizures in children".The Cochrane Database of Systematic Reviews.2021(6): CD003031.doi:10.1002/14651858.CD003031.pub4.PMC8207248.PMID34131913.
- ^Greenhalgh, Janette; Weston, Jennifer; Dundar, Yenal; Nevitt, Sarah; Marson, Anthony (28 April 2020)."Antiepileptic drugs as prophylaxis for postcraniotomy seizures".The Cochrane Database of Systematic Reviews.4(4): CD007286.doi:10.1002/14651858.CD007286.pub5.ISSN1469-493X.PMC7195181.PMID32343399.
- ^Ratilal BO, Pappamikail L, Costa J, Sampaio C (June 2013)."Anticonvulsants for preventing seizures in patients with chronic subdural haematoma".The Cochrane Database of Systematic Reviews.6(6): CD004893.doi:10.1002/14651858.CD004893.pub3.PMC7388908.PMID23744552.
- ^Chang, Richard S.; Leung, William Cy; Vassallo, Michael; Sykes, Lucy; Battersby Wood, Emma; Kwan, Joseph (7 February 2022)."Antiepileptic drugs for the primary and secondary prevention of seizures after stroke".The Cochrane Database of Systematic Reviews.2022(2): CD005398.doi:10.1002/14651858.CD005398.pub4.ISSN1469-493X.PMC8819727.PMID35129214.
- ^abPrice M, Günther A, Kwan JS (April 2016)."Antiepileptic drugs for the primary and secondary prevention of seizures after intracranial venous thrombosis".The Cochrane Database of Systematic Reviews.2016(4): CD005501.doi:10.1002/14651858.CD005501.pub4.hdl:10722/226344.PMC7265129.PMID27098266.
- ^Marigold R, Günther A, Tiwari D, Kwan J (June 2013)."Antiepileptic drugs for the primary and secondary prevention of seizures after subarachnoid haemorrhage".The Cochrane Database of Systematic Reviews.6(6): CD008710.doi:10.1002/14651858.CD008710.pub2.hdl:10722/194540.PMC6885058.PMID23740537.
- ^Al-Mufti F, Claassen J (October 2014). "Neurocritical care: status epilepticus review".Critical Care Clinics.30(4): 751–764.doi:10.1016/j.ccc.2014.06.006.PMID25257739.
- ^O'connor A (22 April 2008)."The Claim: During a Seizure, You Can Swallow Your Tongue".The New York Times.Archivedfrom the original on 6 March 2017.
- ^abcdBetjemann JP (December 2015)."Current Trends in Treatment of Status Epilepticus and Refractory Status Epilepticus".Seminars in Neurology.35(6): 621–628.doi:10.1055/s-0035-1564304.PMID26595862.
- ^De Waele L, Boon P, Ceulemans B, Dan B, Jansen A, Legros B, et al. (December 2013)."First line management of prolonged convulsive seizures in children and adults: good practice points".Acta Neurologica Belgica.113(4): 375–380.doi:10.1007/s13760-013-0247-x.hdl:1854/LU-4182539.PMID24019121.S2CID17641491.
- ^abMarx, J. A., Hockberger, R. S., Walls, R. M., Adams, J., & Rosen, P. (Eds.). (2013). Rosen's emergency medicine: concepts and clinical practice (8th ed). Philadelphia: Mosby/Elsevier.
- ^Leone MA, Giussani G, Nevitt SJ, Marson AG, Beghi E (May 2021)."Immediate antiepileptic drug treatment, versus placebo, deferred, or no treatment for first unprovoked seizure".The Cochrane Database of Systematic Reviews.2021(5): CD007144.doi:10.1002/14651858.CD007144.pub3.PMC8094016.PMID33942281.
- ^abcSharma AN, Hoffman RJ (February 2011). "Toxin-related seizures".Emergency Medicine Clinics of North America.29(1): 125–139.doi:10.1016/j.emc.2010.08.011.PMID21109109.
- ^"Epilepsy surgery | Epilepsy Society".epilepsysociety.org.uk.23 February 2020.Retrieved15 June2024.
- ^abDoherty MJ, Haltiner AM (January 2007). "Wag the dog: skepticism on seizure alert canines".Neurology.68(4): 309.CiteSeerX10.1.1.1003.1543.doi:10.1212/01.wnl.0000252369.82956.a3.PMID17242343.S2CID33328776.
- ^Gloss D, Vickrey B (March 2014)."Cannabinoids for epilepsy".The Cochrane Database of Systematic Reviews.2014(3): CD009270.doi:10.1002/14651858.CD009270.pub3.PMC7120304.PMID24595491.
- ^Belendiuk KA, Baldini LL, Bonn-Miller MO (April 2015)."Narrative review of the safety and efficacy of marijuana for the treatment of commonly state-approved medical and psychiatric disorders".Addiction Science & Clinical Practice.10(1): 10.doi:10.1186/s13722-015-0032-7.PMC4636852.PMID25896576.
- ^Martin-McGill, Kirsty J.; Bresnahan, Rebecca; Levy, Robert G.; Cooper, Paul N. (24 June 2020)."Ketogenic diets for drug-resistant epilepsy".The Cochrane Database of Systematic Reviews.2020(6): CD001903.doi:10.1002/14651858.CD001903.pub5.ISSN1469-493X.PMC7387249.PMID32588435.
- ^Bonnett LJ, Tudur-Smith C, Williamson PR, Marson AG (December 2010)."Risk of recurrence after a first seizure and implications for driving: further analysis of the Multicentre study of early Epilepsy and Single Seizures".BMJ.341:c6477.doi:10.1136/bmj.c6477.PMC2998675.PMID21147743.
- ^Neligan A, Hauser WA, Sander JW (2012). "The epidemiology of the epilepsies".Epilepsy.Handbook of Clinical Neurology. Vol. 107. pp. 113–33.doi:10.1016/B978-0-444-52898-8.00006-9.ISBN9780444528988.PMID22938966.;Sander JW, Shorvon SD (November 1996)."Epidemiology of the epilepsies".Journal of Neurology, Neurosurgery, and Psychiatry.61(5): 433–443.doi:10.1136/jnnp.61.5.433.PMC1074036.PMID8965090.
- ^abcGavvala JR, Schuele SU (December 2016). "New-Onset Seizure in Adults and Adolescents: A Review".JAMA.316(24): 2657–2668.doi:10.1001/jama.2016.18625.PMID28027373.
- ^Camfield P, Camfield C (June 2015)."Incidence, prevalence and aetiology of seizures and epilepsy in children".Epileptic Disorders.17(2): 117–123.doi:10.1684/epd.2015.0736.PMID25895502.S2CID20719640.
- ^abBa-Diop A, Marin B, Druet-Cabanac M, Ngoungou EB, Newton CR, Preux PM (October 2014)."Epidemiology, causes, and treatment of epilepsy in sub-Saharan Africa".The Lancet. Neurology.13(10): 1029–1044.doi:10.1016/S1474-4422(14)70114-0.PMC5497080.PMID25231525.
- ^abMagiorkinis E, Sidiropoulou K, Diamantis A (January 2010). "Hallmarks in the history of epilepsy: epilepsy in antiquity".Epilepsy & Behavior.17(1): 103–108.doi:10.1016/j.yebeh.2009.10.023.PMID19963440.S2CID26340115.
- ^abcdAli R, Connolly ID, Feroze AH, Awad AJ, Choudhri OA, Grant GA (June 2016). "Epilepsy: A Disruptive Force in History".World Neurosurgery.90:685–690.doi:10.1016/j.wneu.2015.11.060.PMID26709155.
- ^Meador KJ, Loring DW, Flanigin HF (January 1989). "History of epilepsy surgery".Journal of Epilepsy.2(1): 21–25.doi:10.1016/0896-6974(89)90054-6.ISSN0896-6974.
- ^abLitt B, Echauz J (May 2002). "Prediction of epileptic seizures".The Lancet. Neurology.1(1): 22–30.doi:10.1016/S1474-4422(02)00003-0.PMID12849542.S2CID10109539.
- ^abWalker MC, Schorge S, Kullmann DM, Wykes RC, Heeroma JH, Mantoan L (September 2013)."Gene therapy in status epilepticus".Epilepsia.54(Suppl 6): 43–45.doi:10.1111/epi.12275.PMID24001071.S2CID13942394.
- ^abMormann F, Andrzejak RG, Elger CE, Lehnertz K (February 2007)."Seizure prediction: the long and winding road".Brain.130(Pt 2): 314–333.doi:10.1093/brain/awl241.PMID17008335.
