Uterine rupture
| Uterine rupture | |
|---|---|
| Specialty | Obstetrics |
| Symptoms | Increased pain, vaginal bleeding, change in contractions[1][2] |
| Usual onset | Duringlabor[3] |
| Risk factors | Vaginal birth after cesarean section,other uterine scars,obstructed labor,induction of labor,trauma,cocaineuse[1][4] |
| Diagnostic method | Supported by a rapid drop in the baby's heart rate[1] |
| Treatment | Surgery[1] |
| Prognosis | 0.1%-10% risk of maternal death,[5]6% risk of infant death[1] |
| Frequency | 1 in 12,000 vaginal deliveries with a normal uterus[1] 1 in 280 withvaginal birth after cesarean section[1] |
Uterine ruptureis when the muscular wall of theuterustears duringpregnancyorchildbirth.[3]Symptoms, while classically including increased pain, vaginal bleeding, or a change incontractions,are not always present.[1][2]Disability or death of the mother or baby may result.[1][3]
Risk factors includevaginal birth after cesarean section(VBAC), other uterine scars,obstructed labor,induction of labor,trauma,andcocaineuse.[1][4]While typically rupture occurs duringlaborit may occasionally happen earlier in pregnancy.[3][1]Diagnosis may be suspected based on a rapid drop in the baby's heart rate during labor.[1][4]Uterinedehiscenceis a less severe condition in which there is only incomplete separation of the old scar.[1]
Treatment involves rapid surgery to control bleeding and delivery of the baby.[1]Ahysterectomymay be required to control the bleeding.[1]Blood transfusionsmay be given to replace blood loss.[1]Women who have had a prior rupture are generally recommended to haveC-sectionsin subsequent pregnancies.[6]
Rates of uterine rupture during vaginal birth following one previousC-section,done by the typical technique, are estimated at 0.9%.[1]Rates are greater among those who have had multiple prior C-sections or an atypical type of C-section.[1]In those who do have uterine scarring, the risk during a vaginal birth is about 1 per 12,000.[1]Risk of death of the baby is about 6%.[1]Those in thedeveloping worldappear to be affected more often and have worse outcomes.[7][3]
Signs and symptoms
[edit]Symptoms of a rupture may be initially quite subtle. An old cesarean scar may undergodehiscence;with further labor the woman may experience abdominal pain and vaginal bleeding, though these signs are difficult to distinguish from normal labor. Often a deterioration of the fetal heart rate is a leading sign, but the cardinal sign of uterine rupture is loss of fetal station on manual vaginal exam. Intra-abdominal bleeding can lead tohypovolemic shockand death. Although the associated maternal mortality is now less than one percent, the fetal mortality rate is between two and six percent when rupture occurs in the hospital.
In pregnancy uterine rupture may cause a viableabdominal pregnancy.This is what accounts for most abdominal pregnancy births.
- Abdominal painand tenderness. The pain may not be severe; it may occur suddenly at the peak of a contraction. The woman may describe a feeling that something "gave way" or "ripped."
- Chest pain,pain between the scapulae, or pain on inspiration—Pain occurs because of the irritation of blood below the woman's diaphragm
- Hypovolemic shockcaused by bleeding, evidenced by falling blood pressure,tachycardia,tachypnea, pallor, cool and clammy skin, and anxiety. The fall in blood pressure is often a late sign of haemorrhage
- Signs associated with fetal oxygenation, such as late deceleration, reduced variability, tachycardia, andbradycardia
- Absent fetal heart sounds with a large disruption of the placenta; absent fetal heart activity by ultrasound examination
- Cessation of uterine contractions
- Palpationof the fetus outside the uterus (usually occurs only with a large, complete rupture). The fetus is likely to be dead at this point.
- Signs of an abdominal pregnancy
- Post-term pregnancy
Risk factors
[edit]A uterine scar from a previouscesarean sectionis the most common risk factor. (In one review, 52% had previous cesarean scars.)[8]Other forms of uterine surgery that result in full-thickness incisions (such as amyomectomy), dysfunctional labor, labor augmentation byoxytocinorprostaglandins,and highparitymay also set the stage for uterine rupture. In 2006, an extremely rare case of uterine rupture in a first pregnancy with no risk factors was reported.[9]
Uterine rupture during pregnancy without a prior cesarean section is one of the major diagnostic criterion for vascularEhlers-Danlos syndrome(vEDS).[10]
Mechanism
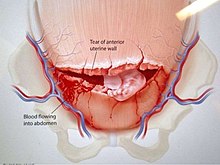
[edit]In an incomplete rupture theperitoneumis still intact. With a complete rupture the contents of the uterus spill into the peritoneal cavity or thebroad ligament.
Treatment
[edit]Emergency exploratorylaparotomywith cesarean delivery accompanied by fluid andblood transfusionare indicated for the management of uterine rupture. Depending on the nature of the rupture and the condition of the patient, the uterus may be either repaired or removed (cesarean hysterectomy). Delay in management places both mother and child at significant risk.
See also
[edit]References
[edit]- ^abcdefghijklmnopqrstToppenberg, KS; Block WA, Jr (1 September 2002). "Uterine rupture: what family physicians need to know".American Family Physician.66(5): 823–8.PMID12322775.
- ^abLang, CT; Landon, MB (March 2010). "Uterine rupture as a source of obstetrical hemorrhage".Clinical Obstetrics and Gynecology.53(1): 237–51.doi:10.1097/GRF.0b013e3181cc4538.PMID20142660.
- ^abcdeMurphy, DJ (April 2006). "Uterine rupture".Current Opinion in Obstetrics & Gynecology.18(2): 135–40.doi:10.1097/01.gco.0000192989.45589.57.PMID16601473.S2CID23617249.
- ^abcMirza, FG; Gaddipati, S (April 2009). "Obstetric emergencies".Seminars in Perinatology.33(2): 97–103.doi:10.1053/j.semperi.2009.01.003.PMID19324238.
- ^Togioka, Brandon M.; Tonismae, Tiffany (June 27, 2022)."Uterine Rupture".StatPearls.PMID32644635.Retrieved5 March2023.
- ^Larrea, NA; Metz, TD (January 2018). "Pregnancy After Uterine Rupture".Obstetrics and Gynecology.131(1): 135–137.doi:10.1097/AOG.0000000000002373.PMID29215521.
- ^Berhe, Y; Wall, LL (November 2014). "Uterine rupture in resource-poor countries".Obstetrical & Gynecological Survey.69(11): 695–707.doi:10.1097/OGX.0000000000000123.PMID25409161.S2CID22593593.
- ^Chibber R, El-Saleh E, Fadhli RA, Jassar WA, Harmi JA (March 2010). "Uterine rupture and subsequent pregnancy outcome - how safe is it? A 25-year study".J Matern Fetal Neonatal Med.23(5): 421–4.doi:10.3109/14767050903440489.PMID20230321.S2CID13566623.
- ^Walsh CA, O'Sullivan RJ, Foley ME (2006). "Unexplained prelabor uterine rupture in a term primigravida".Obstetrics and Gynecology.108(3 Pt 2): 725–7.doi:10.1097/01.AOG.0000195065.38149.11.PMID17018479.S2CID8021433.
- ^Byers, Peter H. (2019).Vascular Ehlers-Danlos Syndrome.University of Washington, Seattle.PMID20301667.
